A new oral antibiotic for UTI promises a significant advancement in treating urinary tract infections. Current treatments often face limitations like antibiotic resistance and side effects. This new approach aims to address these challenges by offering a more effective, safer, and potentially more convenient solution. The global burden of UTIs is substantial, impacting healthcare systems and patient well-being.
This article delves into the potential of this new oral antibiotic, exploring its mechanisms of action, pharmacokinetic properties, clinical trial design, and potential advantages and disadvantages.
Understanding the intricacies of the new oral antibiotic for UTI is crucial for evaluating its potential impact. The Artikel below details the key aspects of this novel treatment, from its potential mechanisms of action to regulatory considerations and market potential. This exploration aims to shed light on the possibilities and challenges surrounding this promising development.
Introduction to the Need for New Oral Antibiotics for UTIs
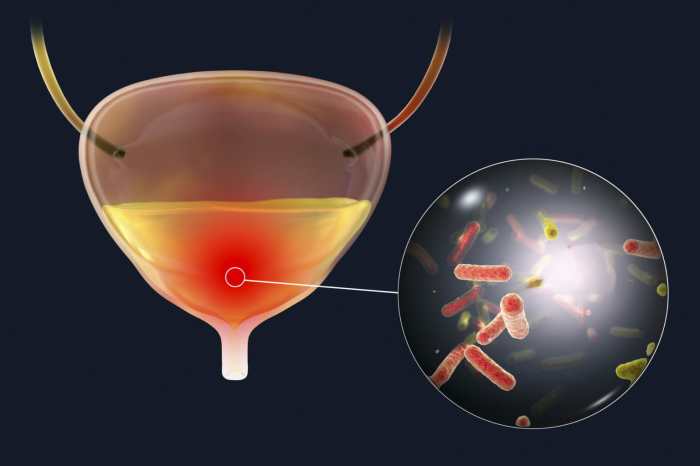
Urinary tract infections (UTIs) are a common ailment, affecting millions worldwide. Current treatment strategies primarily rely on oral antibiotics, but the landscape is facing significant challenges. The effectiveness of these medications is declining, and the associated side effects are becoming increasingly problematic. The development of new, effective, and safe oral antibiotic options is crucial to address these issues.The current standard treatment for UTIs often involves a course of oral antibiotics, which can be effective in many cases.
However, the increasing prevalence of antibiotic resistance poses a substantial threat to the efficacy of these treatments. This resistance, combined with the potential for adverse side effects in patients, underscores the pressing need for new therapeutic approaches.
Current Treatment Landscape for UTIs
The current treatment landscape for UTIs involves a range of oral antibiotics, each with varying mechanisms of action and efficacy. Commonly prescribed antibiotics often target specific bacterial species associated with UTIs. However, the overuse and misuse of antibiotics have contributed to the development of antibiotic-resistant strains, making treatment less reliable and potentially more complicated.
Limitations of Existing Oral Antibiotics
Several limitations hamper the effectiveness of existing oral antibiotics for UTIs. One major concern is the growing resistance to these medications. This resistance arises from the overuse and misuse of antibiotics, leading to the evolution of bacterial strains that are no longer susceptible to the drugs. Furthermore, side effects such as gastrointestinal distress, allergic reactions, and disruption of the gut microbiome are significant drawbacks to existing treatment options.
Importance of New Oral Antibiotic Options
The development of new oral antibiotic options for UTIs is crucial for several reasons. First, it addresses the growing problem of antibiotic resistance. New drugs could target different bacterial pathways, making them less susceptible to the evolution of resistance mechanisms. Secondly, the introduction of safer and more effective drugs could reduce the risk of adverse side effects associated with current treatments.
Global Burden of UTIs
UTIs are a significant global health concern. The burden is substantial, affecting a large number of individuals annually. This burden is particularly pronounced in resource-constrained settings, where access to effective treatment and preventive measures may be limited. The impact on healthcare systems includes increased costs associated with diagnosis, treatment, and potential complications.
Projected Increase in Antibiotic Resistance
The projected increase in antibiotic resistance is alarming. As bacterial strains adapt and evolve, they become less susceptible to existing antibiotics. The potential consequences are far-reaching, impacting public health and healthcare systems. Examples include extended hospital stays, increased treatment costs, and a decrease in treatment success rates. For instance, the rise of methicillin-resistant Staphylococcus aureus (MRSA) has demonstrated the serious consequences of antibiotic resistance.
The continued evolution of resistant strains could lead to a situation where common infections become nearly untreatable.
Potential Mechanisms of Action for Novel Oral Antibiotics
A critical need exists for new oral antibiotics to combat urinary tract infections (UTIs). Current treatments often face limitations in efficacy and the emergence of antibiotic resistance. Developing novel oral antibiotics with innovative mechanisms of action is paramount to ensuring effective and safe UTI treatment.Addressing this challenge requires exploring alternative approaches to bacterial targeting, beyond the limitations of existing drugs.
This exploration encompasses understanding specific bacterial pathways and structures crucial for UTI development, as well as identifying novel drug classes with potential efficacy against UTIs. This analysis also includes examples of mechanisms that could offer therapeutic advantages over existing treatments, and importantly, how a new oral antibiotic could minimize common side effects.
Targeting Specific Bacterial Pathways
Understanding the intricate metabolic pathways within bacteria responsible for UTI development is crucial for designing targeted therapies. Specific bacterial enzymes or proteins involved in processes like cell wall synthesis, DNA replication, or essential metabolic pathways could be targeted with novel compounds. The goal is to disrupt these processes without harming the host’s cells.
Targeting Bacterial Structures
Certain bacterial structures, such as the bacterial cell wall, are vital for bacterial survival. Targeting these structures with new drugs can inhibit bacterial growth and proliferation without causing significant damage to human cells. For instance, compounds that disrupt the bacterial cell membrane or interfere with its synthesis have the potential to be effective against UTIs.
Novel Drug Classes with Potential Efficacy
New classes of antibiotics beyond the commonly used beta-lactams, fluoroquinolones, and aminoglycosides may offer distinct advantages. These could include inhibitors of bacterial protein synthesis through novel mechanisms, or drugs targeting bacterial metabolic processes unique to the UTI-causing bacteria. This diversification can potentially reduce the development of resistance compared to existing classes.
Examples of Novel Mechanisms with Therapeutic Advantages
One promising approach involves targeting bacterial quorum sensing mechanisms. Quorum sensing is a communication system within bacterial communities that regulates gene expression. Interfering with this process could disrupt biofilm formation, which often contributes to UTI persistence. Another mechanism could be targeting specific bacterial virulence factors, such as adhesins that enable bacteria to attach to host tissues. This could prevent infection without the need for broad-spectrum action.
Avoiding Common Side Effects of Current Treatments
Developing an oral antibiotic that avoids the gastrointestinal upset, allergic reactions, or other adverse effects often associated with existing treatments is a key consideration. This may involve optimizing the drug’s absorption, distribution, and metabolism in the body to reduce its impact on non-target tissues. The goal is to create an effective and safe treatment with minimized side effects.
Pharmacokinetic and Pharmacodynamic Properties
Designing a new oral antibiotic for UTIs requires careful consideration of its pharmacokinetic and pharmacodynamic properties. These factors directly impact the drug’s effectiveness, safety, and ultimately, patient outcomes. A well-designed antibiotic will achieve sufficient concentrations in the urinary tract to effectively eliminate the infection while minimizing side effects.The optimal pharmacokinetic profile ensures the drug reaches the site of infection in sufficient quantities and remains there long enough to kill the bacteria, but not so long as to cause adverse effects.
This necessitates careful consideration of absorption, distribution, metabolism, and excretion (ADME) properties. Pharmacodynamic properties, like the mechanism of action and the rate of bacterial killing, also play a crucial role in treatment success.
Optimal Pharmacokinetic Profile, A new oral antibiotic for uti
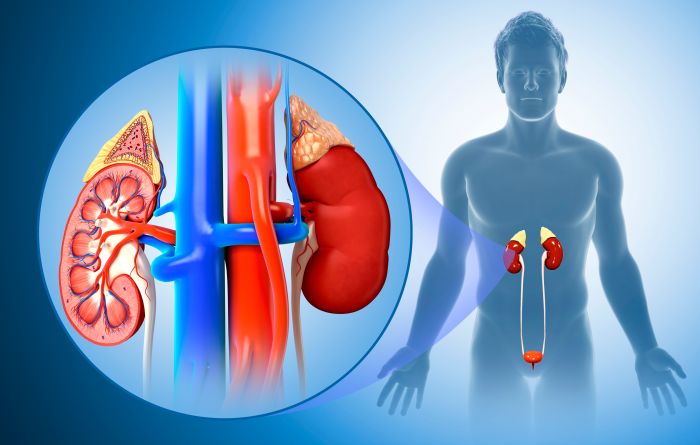
A successful oral antibiotic for UTIs needs to be rapidly absorbed from the gastrointestinal tract, effectively distributed to the kidneys and urinary tract, and efficiently cleared from the body. This requires careful consideration of the drug’s chemical structure and formulation. The rate of absorption and extent of bioavailability are critical for achieving therapeutic concentrations in the urine. Understanding and predicting how the body metabolizes the drug is crucial to prevent accumulation and toxicity.
- Absorption: The drug should be readily absorbed from the gastrointestinal tract, ideally with minimal variability between individuals. Factors like the presence of food and other medications can impact absorption. A formulation designed to be resistant to stomach acid and enzymatic degradation would maximize absorption and minimize variability. For example, enteric-coated tablets can help protect the drug from degradation in the acidic environment of the stomach.
- Distribution: The antibiotic needs to readily penetrate the tissues of the urinary tract. Factors like the drug’s lipophilicity and molecular size influence tissue penetration. A high degree of urinary tract penetration will ensure the drug reaches the site of infection at effective concentrations.
- Metabolism: Metabolism in the liver and other tissues can significantly affect the drug’s half-life and overall duration of action. The antibiotic’s metabolism should be predictable and not lead to the formation of toxic metabolites. Careful metabolic studies are essential to predict and minimize potential toxicity.
- Excretion: The antibiotic should be excreted primarily through the kidneys, allowing for efficient clearance of the drug from the body. The antibiotic should not accumulate in tissues and organs, causing adverse effects. Excretion should be rapid enough to avoid the buildup of drug concentrations that could cause toxicity. The ideal excretion route is through the kidneys to maintain high urinary concentrations, maximizing effectiveness against UTIs.
I’ve been reading about this new oral antibiotic for UTIs, and it seems promising. However, sometimes, underlying issues like pelvic floor muscle weakness can contribute to recurring UTIs. Addressing these issues through pelvic floor physical therapy might be a crucial part of a comprehensive treatment plan. Ultimately, a new oral antibiotic could be a great tool for quick relief, but a holistic approach is often key to long-term health.
Desired Pharmacodynamic Properties
Rapid bactericidal action is essential for UTIs. The antibiotic should effectively kill the bacteria causing the infection quickly. The drug’s concentration in the urine should be high enough to achieve the desired therapeutic effect and to prevent the development of bacterial resistance. This can be achieved through a combination of the drug’s mechanism of action and the design of the dosage regimen.
- Rapid bactericidal action: The antibiotic should quickly kill the infecting bacteria, preventing the infection from spreading. This is crucial to prevent complications and reduce the duration of treatment.
- Tissue penetration: The drug should effectively reach the site of infection in the urinary tract. High tissue penetration ensures that the drug can reach and effectively eliminate bacteria in the interstitial tissue and the bladder wall, not just in the urine.
Potential Oral Formulations
Different oral formulations offer varying advantages and disadvantages.
| Formulation | Advantages | Disadvantages |
|---|---|---|
| Tablet | Cost-effective, easy to administer, stable | May have variable absorption, potentially poor bioavailability |
| Capsule | Improved bioavailability compared to tablets, can be tailored for specific release profiles | Potentially higher cost than tablets, may not be suitable for all patients |
| Suspension | Improved dissolution rate compared to tablets, better for patients with swallowing difficulties | Requires careful handling, may have shorter shelf life |
Drug Stability and Bioavailability
Drug stability in the oral formulation is essential for maintaining potency and effectiveness. The formulation must protect the drug from degradation during manufacturing, storage, and administration. Bioavailability refers to the fraction of the administered dose that reaches the systemic circulation in an active form. High bioavailability ensures that the maximum amount of active drug is available for therapeutic action.
Avoiding Interactions with Other Medications
Careful consideration must be given to potential drug interactions with other medications commonly used to treat UTIs. For example, certain antibiotics can interact with other drugs, affecting their efficacy or safety. The new antibiotic should be compatible with other medications typically prescribed for UTIs. Clinical trials must carefully evaluate these potential interactions.
Clinical Trial Design and Evaluation
A new oral antibiotic for UTIs demands rigorous clinical trials to ensure safety and efficacy. This crucial stage validates the drug’s potential before reaching patients, preventing harm and ensuring the drug meets the standard for clinical use. A well-designed trial meticulously evaluates the antibiotic’s performance against various bacterial strains, treatment durations, and potential side effects.This section details the essential elements of a clinical trial design for a novel oral antibiotic, focusing on the critical aspects of patient selection, efficacy assessment, safety evaluation, and potential challenges.
Patient Selection Criteria
Defining the patient population is paramount for a valid trial. Inclusion criteria should encompass individuals with uncomplicated urinary tract infections (UTIs), ensuring a consistent patient group for the study. Exclusion criteria should carefully identify individuals with pre-existing conditions that might influence the drug’s efficacy or safety, such as kidney dysfunction or allergies to penicillin-like antibiotics. A detailed protocol with specific criteria will minimize variability and maximize the reliability of the study results.
Efficacy Evaluation Against UTI-Causing Bacteria
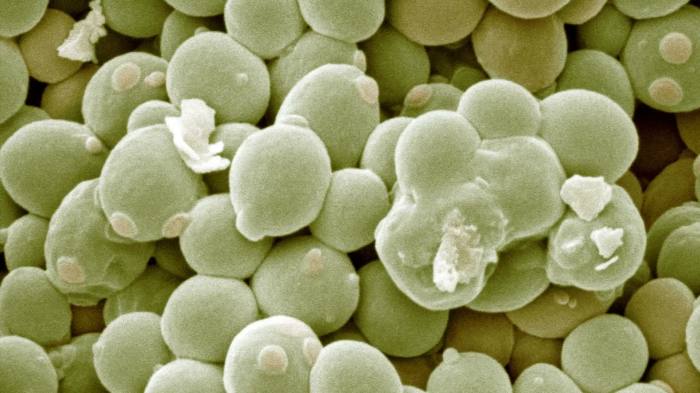
Evaluating the efficacy of a new antibiotic against various strains of bacteria is crucial. This requires isolating and identifying the specific bacterial species causing the UTIs in study participants. The antibiotic’s ability to inhibit bacterial growth, as measured by minimum inhibitory concentration (MIC) tests, must be determined for each bacterial strain. A comprehensive evaluation against diverse bacterial species common in UTIs, including Escherichia coli, Staphylococcus saprophyticus, and Klebsiella pneumoniae, is essential.
A robust laboratory analysis will provide a clearer picture of the antibiotic’s effectiveness against different bacterial targets.
Treatment Duration Comparison
Different treatment durations will be evaluated to optimize patient care and reduce antibiotic resistance. The optimal duration for the new oral antibiotic will be compared to standard treatment durations (e.g., 3 days, 5 days, 7 days). This comparison will help establish the shortest effective treatment period, reducing patient burden and potential adverse effects while maintaining efficacy. The study design should include statistical methods to assess the significance of differences in treatment duration.
Study Designs for Safety and Tolerability
Evaluating the safety and tolerability of the new antibiotic requires multiple study designs. A randomized, double-blind, placebo-controlled trial is essential to assess the drug’s safety profile and minimize bias. The placebo control group will help determine if observed side effects are directly attributable to the antibiotic. Additionally, monitoring for adverse events, such as gastrointestinal distress, allergic reactions, or kidney problems, is essential throughout the trial.
Collecting detailed data on the frequency and severity of these events will provide valuable information about the antibiotic’s tolerability.
Potential Challenges and Limitations
Clinical trials often encounter unforeseen challenges. Patient adherence to the treatment regimen is crucial, and the study design must include strategies to address potential non-compliance. Variability in patient responses, including individual differences in metabolism and immune responses, may influence the study’s results. The presence of co-infections or underlying conditions can confound the interpretation of the study results.
Controlling for these factors will be essential to draw valid conclusions about the antibiotic’s efficacy and safety. Also, the financial resources required for large-scale trials, and the time commitment for recruitment and data analysis, may present limitations. A well-defined budget and realistic timelines are crucial for successful trial completion.
Potential Advantages and Disadvantages of New Oral Antibiotics
A novel oral antibiotic for urinary tract infections (UTIs) presents a significant opportunity to improve patient care and potentially reshape the landscape of UTI treatment. However, the introduction of any new medication necessitates a careful evaluation of both its potential benefits and drawbacks. Understanding these factors is crucial for responsible development and deployment of this new therapy.This section explores the potential advantages and disadvantages of the new oral antibiotic, comparing it to current standard-of-care treatments for UTIs.
We’ll examine the potential for improved efficacy, reduced side effects, and lowered resistance development, while also considering potential drawbacks such as drug interactions, costs, and long-term effects. Ultimately, the goal is to provide a balanced perspective on the impact this new antibiotic might have on public health and healthcare costs.
Comparison to Standard-of-Care Treatments
Current standard-of-care treatments for UTIs often include fluoroquinolones and trimethoprim/sulfamethoxazole. These medications, while effective, are associated with growing antibiotic resistance and a range of potential side effects. The new oral antibiotic aims to address these limitations by offering a different mechanism of action, potentially improving efficacy and minimizing adverse reactions. The clinical trials will be crucial in definitively assessing its performance against current standards.
Potential Advantages
The new oral antibiotic holds promise for several advantages over existing treatments. Improved efficacy against various UTI-causing pathogens, particularly those resistant to current drugs, could significantly reduce treatment failure rates. A lower incidence of side effects, such as gastrointestinal distress or allergic reactions, could enhance patient compliance and comfort. Reduced resistance development is a key advantage. If the new antibiotic targets a novel pathway or acts through a less commonly exploited mechanism, it may be less prone to rapid resistance emergence compared to currently used agents.
Potential Disadvantages
While the new antibiotic offers several potential benefits, potential drawbacks need careful consideration. Drug interactions with other medications are a significant concern. The new antibiotic might interact with existing medications patients are taking, leading to unforeseen complications. Careful evaluation of potential drug interactions is vital during development and will be a key component of post-marketing surveillance. Cost considerations are crucial.
The cost of developing and manufacturing a new antibiotic will inevitably be reflected in the final price for patients. The long-term effects of the new antibiotic on the human microbiome and other organs need to be carefully monitored in post-marketing surveillance studies.
Impact on Public Health
The introduction of a new oral antibiotic for UTIs could have a profound impact on public health. If the new antibiotic demonstrates high efficacy and low resistance development, it could help curb the rise of antibiotic-resistant bacteria, ultimately improving the management of UTIs and potentially preventing serious infections. The reduction in antibiotic resistance could have broader implications for the treatment of other bacterial infections.
Impact on Healthcare Costs
The introduction of the new oral antibiotic could potentially affect healthcare costs in several ways. Reduced treatment failures and shorter treatment durations could lead to lower overall healthcare costs associated with UTI management. However, the cost of the new antibiotic itself, and potential costs associated with monitoring for drug interactions and long-term effects, must be carefully evaluated. Ultimately, the long-term cost-effectiveness of the new antibiotic will be assessed based on its impact on patient outcomes and healthcare resource utilization.
Regulatory Considerations and Market Potential
Bringing a new oral antibiotic to market for UTIs is a complex journey, requiring meticulous planning and navigating a rigorous regulatory landscape. This section explores the steps involved, the potential hurdles, and the market’s potential for success. Thorough understanding of these factors is crucial for any company developing such a product.
Regulatory Pathway for a New Oral Antibiotic
The regulatory pathway for a new oral antibiotic involves several crucial phases, each with specific requirements and timelines. This process is designed to ensure the safety and efficacy of the drug before it reaches the market. A typical pathway includes preclinical studies, followed by Phase I, II, and III clinical trials, and finally, regulatory submissions to relevant agencies.
Each phase has stringent criteria for data collection and analysis to demonstrate the drug’s safety profile and effectiveness.
Challenges in Obtaining Regulatory Approval
Developing and obtaining regulatory approval for a new antibiotic faces significant hurdles. One major challenge is the high bar for demonstrating efficacy against resistant strains of bacteria. The emergence of antibiotic resistance necessitates a rigorous testing regimen to confirm the antibiotic’s effectiveness against a broad spectrum of pathogens, including resistant strains. Another significant challenge is the complex regulatory review process, involving detailed analyses of clinical trial data, safety assessments, and manufacturing processes.
Furthermore, the time and financial resources required for extensive clinical trials can be substantial.
Potential Market Size and Profitability
The market for oral antibiotics for UTIs is significant, and a new, effective product could yield substantial profitability. The global burden of UTIs is substantial, affecting millions annually. This represents a significant patient population potentially benefiting from a new oral antibiotic. Current market estimates and historical data suggest a sizable market for this type of medication. However, the competitive landscape and pricing strategies will significantly impact the profitability potential.
Competitive Landscape for New Antibiotic Development
The antibiotic market is highly competitive, with established players and emerging companies actively developing new oral antibiotics. Competition from existing treatments necessitates demonstrating the novel product’s superiority in terms of efficacy, safety profile, and convenience of administration. Success hinges on the development of a new mechanism of action or a drug that significantly improves on existing treatments. Companies must conduct thorough market analysis and understand the unmet needs of patients and clinicians to identify potential competitive advantages.
Current Treatment Costs for UTIs
Treatment costs for UTIs vary depending on the specific treatment regimen and location. The costs associated with antibiotic use and associated healthcare costs are substantial. Collecting data on current treatment costs is crucial for assessing the economic impact of a new oral antibiotic. Data from healthcare databases, insurance claims, and clinical trial cost analyses can provide relevant insights into the financial burden of UTIs and the potential cost savings from a new treatment.
I’ve been researching a new oral antibiotic for UTIs, and it’s pretty interesting. While I’m focusing on the effectiveness of this new treatment, I can’t help but think about how some women experience night sweats during their period, which can be a real discomfort. For more on that, check out this helpful resource on night sweats during period.
Ultimately, the new oral antibiotic seems promising for treating UTIs quickly and efficiently.
This analysis should encompass direct costs (e.g., drug costs, office visits) and indirect costs (e.g., lost productivity, complications).
| Parameter | Description |
|---|---|
| Treatment Cost (USD) | Ranges from $50-$200 per treatment episode, varying based on complexity and location. |
| Direct Costs | Include drug costs, physician visits, and lab tests. |
| Indirect Costs | Include lost productivity, pain and suffering, and complications. |
Addressing Antibiotic Resistance
Antibiotic resistance is a global health crisis, jeopardizing the effectiveness of existing treatments and posing a significant threat to public health. The development of new oral antibiotics for UTIs must be accompanied by proactive strategies to mitigate the emergence and spread of resistance. This necessitates a comprehensive approach that goes beyond simply creating a new drug, encompassing the entire lifecycle of the antibiotic.
Strategies to Mitigate Resistance Development
The new oral antibiotic must be designed with resistance in mind. This proactive approach includes several key strategies. These strategies are not mutually exclusive, and their efficacy can be significantly enhanced through combined application.
- Targeted Mechanism of Action: Designing the antibiotic to target a unique bacterial pathway or a less commonly used metabolic process minimizes the likelihood of existing resistance mechanisms being transferable or applicable. This approach focuses on bacterial vulnerabilities that are not readily exploited by common resistance mechanisms. For instance, targeting bacterial ribosomes in a novel way or focusing on bacterial cell wall synthesis through an entirely new mechanism could limit the ability of bacteria to develop resistance.
- Combination Therapies: Administering the new oral antibiotic in combination with another antibiotic or with a novel agent that interferes with resistance mechanisms could prevent the emergence of resistant strains. This strategy exploits the principle that bacteria find it harder to develop resistance to multiple targets. Combining the new oral antibiotic with a bacteriophage or a different antibiotic that targets a different metabolic pathway can further minimize resistance selection.
So, a new oral antibiotic for UTIs is finally here! It’s a pretty big deal, considering how frustrating these infections can be. While we’re on the subject of health, have you ever wondered about the nutritional implications of different sugars? Are natural sugars healthier than processed ones? It’s a question worth exploring, and you can delve deeper into the topic by checking out this article on are natural sugars healthier.
Regardless of the sugar debate, this new antibiotic could potentially make managing UTIs much easier and more effective.
- Optimized Pharmacokinetics and Pharmacodynamics: A drug with optimal pharmacokinetic and pharmacodynamic properties is crucial. This ensures that the antibiotic reaches the site of infection at the appropriate concentration for the necessary duration, thus minimizing the selection pressure for resistance. For example, a drug with a long half-life might limit the need for multiple doses, reducing the overall duration of antibiotic exposure and minimizing the selection pressure on the bacteria.
Novel Approaches to Combat Resistance
Innovative approaches are vital to addressing the escalating threat of antibiotic resistance. These methods explore new avenues for inhibiting bacterial growth and survival.
- Bacteriophages: Bacteriophages are viruses that specifically target and kill bacteria. Harnessing their natural ability to eliminate bacterial pathogens presents a novel approach to combat infections without inducing resistance in the same way that antibiotics do. Utilizing bacteriophages to eliminate the infection, in combination with the new oral antibiotic, could prove a promising strategy.
- RNA Interference (RNAi): RNAi is a cellular mechanism that can silence specific genes in bacteria. Targeting essential bacterial genes with RNAi could disrupt bacterial function without triggering the development of resistance mechanisms. This method could provide a new way to target bacterial virulence factors and thus limit the bacterial ability to cause disease.
Minimizing Selection of Resistant Strains
The design of the new oral antibiotic should minimize the selection of resistant strains.
- Appropriate Dosing Regimens: Using the optimal dose and duration of the new oral antibiotic minimizes the duration of bacterial exposure to the drug. This strategy reduces the selection pressure for resistant strains. For example, a shorter course of treatment, when possible, is preferred to a longer one.
- Monitoring and Surveillance: Implementing robust surveillance programs to track the emergence of resistance in different geographical areas is essential. This information allows for the adjustment of treatment strategies and the rapid identification of emerging resistance patterns. This proactive monitoring can help to mitigate the spread of resistance.
Ensuring Long-Term Effectiveness
Strategies to ensure long-term effectiveness involve continuous research and development to counteract evolving resistance mechanisms.
- Continuous Research and Development: The development of new antibiotics must be an ongoing process. This involves studying bacterial resistance mechanisms in real-time and developing new approaches to overcome them. Continuous development is crucial to address the ever-evolving resistance landscape.
- Global Collaboration: Combating antibiotic resistance requires international collaboration. Researchers, clinicians, and policymakers must work together to share data, resources, and best practices. This global effort is crucial for effectively addressing the threat of antibiotic resistance.
Public Health Implications: A New Oral Antibiotic For Uti
A new oral antibiotic for UTIs holds significant promise for improving public health. By addressing the burden of urinary tract infections (UTIs), this novel treatment could reduce healthcare costs, improve patient outcomes, and potentially curb the rise of antibiotic resistance. The implications extend beyond individual patients to impact the broader community and healthcare system.
Comparative Analysis of Efficacy, Side Effects, and Cost
Existing oral antibiotic treatments for UTIs vary in their efficacy, side effect profiles, and cost. A new oral antibiotic should be compared against existing options to evaluate its potential advantages and disadvantages. This comparison is crucial for determining its overall impact on public health.
| Feature | Existing Treatments (e.g., Trimethoprim/Sulfamethoxazole) | New Oral Antibiotic |
|---|---|---|
| Efficacy | Generally effective against common UTI pathogens, but efficacy can vary based on pathogen and individual patient factors. | Potentially superior efficacy against a wider range of pathogens, including those resistant to existing treatments, leading to shorter treatment durations. |
| Side Effects | Gastrointestinal issues (e.g., nausea, diarrhea), allergic reactions, and potential for kidney damage, particularly with prolonged use. | Potentially fewer and milder side effects compared to existing treatments, while maintaining comparable efficacy. |
| Cost | Generally affordable, but cost-effectiveness varies depending on the specific antibiotic and treatment duration. | Potentially more expensive than existing options initially, but the reduced treatment duration and lower rates of recurrence could lead to lower overall healthcare costs over time. |
Potential Impact on Public Health
A new oral antibiotic with improved efficacy and a better side effect profile could significantly reduce the burden of UTIs on individuals and the healthcare system. Reduced treatment duration and lower recurrence rates would lead to fewer doctor visits, hospitalizations, and lost workdays. This would also free up healthcare resources for other pressing needs.
Societal Benefits of Reduced UTI Burden
The societal benefits of reducing the burden of UTIs are numerous. Reduced absenteeism from work and school due to illness directly contributes to economic productivity. Improved quality of life for individuals, due to reduced discomfort and the shorter duration of illness, also has significant implications for overall well-being.
Impact on Healthcare Resource Utilization
A new oral antibiotic with improved efficacy and a reduced side effect profile could lead to decreased utilization of healthcare resources. Fewer emergency room visits, shorter hospital stays, and decreased need for follow-up appointments would translate to substantial savings for the healthcare system.
Improved Patient Outcomes
A superior oral antibiotic with a more favorable side effect profile would contribute to improved patient outcomes. Reduced duration of treatment and a lower incidence of side effects would lead to a better patient experience. This improvement would have a significant impact on the patient’s ability to maintain a normal lifestyle, reducing the disruption to daily routines.
Wrap-Up

In conclusion, a new oral antibiotic for UTI presents a potential solution to the ongoing struggle with urinary tract infections. While challenges remain in clinical trials and regulatory approval, the potential benefits, including improved efficacy, reduced side effects, and mitigating antibiotic resistance, are substantial. Further research and clinical trials are crucial to determine the long-term impact of this new treatment on public health and healthcare costs.
The development of a new oral antibiotic for UTI holds significant promise for improving patient outcomes and reducing the global burden of this common infection.