How herbs can affect thyroid disease is a complex and fascinating area of study. Thyroid function is crucial for many bodily processes, and imbalances can lead to a range of symptoms. Understanding how certain herbs might interact with the thyroid gland, whether positively or negatively, is essential for anyone considering using them to support their thyroid health. This exploration delves into the potential effects of various herbs, examining their mechanisms of action, potential interactions with medications, and the importance of professional guidance.
This comprehensive guide will cover a variety of herbs, including turmeric, ginger, ashwagandha, and ginseng, examining their potential impacts on thyroid function. It will also address the critical issue of potential interactions with thyroid medications, highlighting the need for careful consideration and consultation with a healthcare professional before incorporating any herbal remedies into your thyroid management plan.
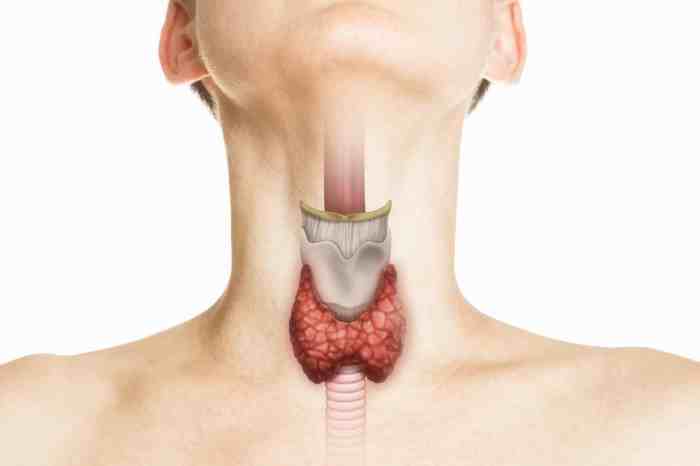
Introduction to Thyroid Disease and Herbs
The thyroid gland, a butterfly-shaped organ located in the neck, plays a crucial role in regulating metabolism throughout the body. It produces hormones, primarily thyroxine (T4) and triiodothyronine (T3), that influence various bodily functions, including heart rate, body temperature, and energy levels. These hormones are essential for maintaining a healthy weight, energy levels, and overall well-being. Disruptions in thyroid function can lead to a variety of health issues, collectively known as thyroid disorders.Thyroid disorders are broadly categorized into two main types: hypothyroidism and hyperthyroidism.
Hypothyroidism occurs when the thyroid gland doesn’t produce enough hormones, leading to a slowed metabolism. Conversely, hyperthyroidism is characterized by an overactive thyroid gland, resulting in an accelerated metabolism. Both conditions can have a significant impact on an individual’s health and well-being, and the symptoms can vary widely.
Types of Thyroid Disease
Hypothyroidism is often characterized by fatigue, weight gain, cold intolerance, constipation, dry skin, and hair loss. Conversely, hyperthyroidism can manifest as nervousness, weight loss, heat intolerance, increased heart rate, and tremors. These symptoms can be subtle or quite pronounced, and it’s crucial to seek medical attention for proper diagnosis and treatment. Accurate diagnosis often involves blood tests to measure thyroid hormone levels.
Mechanisms of Herbal Influence
Herbs may potentially influence thyroid function through various mechanisms, including their effects on hormone production, metabolism, and absorption. Some herbs contain compounds that can stimulate or inhibit thyroid hormone production. Others may affect the conversion of T4 to T3, an important step in thyroid hormone activity. However, it’s essential to understand that the effects of herbs on the thyroid are not always well-understood, and more research is needed to fully elucidate their mechanisms of action.
Common Herbs and Potential Effects
| Herb Name | Potential Effect | Supporting Evidence |
|---|---|---|
| Ashwagandha | May support thyroid function, potentially by reducing stress and inflammation. | Some studies suggest potential benefits, but more research is needed. |
| Ginger | May have a slight effect on thyroid function, but further studies are required. | Limited evidence is available. |
| Kelp | May increase thyroid hormone levels, though this effect is not consistent across studies. | Some studies have reported potential increases in thyroid hormone, but results are mixed and further research is needed. |
| Turmeric | Potential anti-inflammatory effects, which might indirectly support thyroid health. | Limited research, primarily focusing on anti-inflammatory properties, rather than direct thyroid effects. |
| Lemon Balm | May have an impact on thyroid hormone levels, but more studies are required. | Limited research, with mixed results. |
Note that this table presents potential effects, and individual responses may vary. It is crucial to consult with a healthcare professional before using any herbs, especially if you have an existing thyroid condition. Self-treating thyroid conditions can be risky.
Exploring Specific Herbs and Their Effects
Herbal remedies have long been used to support overall health, and some people believe certain herbs can positively impact thyroid function. However, it’s crucial to remember that herbs are not a substitute for medical treatment. Consulting with a healthcare professional is essential before incorporating any herbal supplements into your thyroid management plan. These supplements may interact with medications or have unintended consequences.
Potential Effects of Turmeric on Thyroid Function
Turmeric, known for its vibrant color and potent anti-inflammatory properties, contains curcumin, a compound with antioxidant and anti-inflammatory effects. Some studies suggest that curcumin may influence thyroid hormone levels, although the mechanisms are not fully understood. Preliminary research indicates that curcumin might potentially increase the production of thyroid hormones. However, more robust clinical trials are needed to confirm these findings and establish optimal dosage and duration of use.
It’s important to note that these effects are still under investigation, and the long-term consequences are not definitively known.
Comparison of Turmeric and Ginger Effects on Thyroid Function
Ginger, another commonly used spice, also possesses anti-inflammatory and antioxidant properties. Compared to turmeric, ginger’s potential impact on thyroid function is less extensively studied. While both herbs have demonstrated antioxidant properties, their specific effects on thyroid hormone production and regulation require further investigation. More research is needed to fully understand the comparative effects of these herbs on thyroid health.
Herbal remedies can sometimes influence thyroid function, but it’s crucial to remember that they aren’t a replacement for professional medical advice. While some herbs might offer potential benefits, it’s important to consider how they interact with other health conditions, such as those affecting the skin. For instance, choosing the right skin care emollients and moisturizers skin care emollients moisturizers can significantly impact overall well-being, potentially affecting the thyroid’s response to treatment.
Ultimately, the role of herbs in managing thyroid disease should always be discussed with a doctor.
Potential Benefits of Ashwagandha on Thyroid Function
Ashwagandha, an adaptogenic herb, is often used to reduce stress and improve overall well-being. Some studies suggest that ashwagandha may positively influence thyroid function by modulating stress responses, which could indirectly impact thyroid hormone levels. However, the precise mechanisms by which ashwagandha affects the thyroid remain unclear, and more robust clinical trials are necessary to establish a conclusive link.
It’s crucial to note that individual responses to ashwagandha can vary.
While herbs can potentially influence thyroid function, it’s crucial to remember that they’re not a replacement for medical treatment. For example, some herbs might interact with medications for conditions like stage 3 lung cancer overview, which is a serious concern. It’s always best to consult with a healthcare professional before incorporating any new herbal remedies into your thyroid health management plan.
Potential Effects of Ginseng on Thyroid Function
Ginseng, another popular adaptogenic herb, has been used for centuries to support energy levels and immune function. Research on ginseng’s impact on thyroid function is limited, but some studies suggest that it might influence thyroid hormone metabolism. However, further investigation is needed to understand the extent of these potential effects and to determine optimal dosages and safety considerations. It’s crucial to remember that the evidence supporting ginseng’s impact on thyroid function is still preliminary.
Potential Interactions Between Herbs and Thyroid Medications
| Herb | Medication | Potential Interaction | Severity |
|---|---|---|---|
| Turmeric | Thyroid hormone replacement therapy (e.g., levothyroxine) | May potentially decrease absorption of thyroid hormones | Moderate |
| Ginger | Thyroid hormone replacement therapy (e.g., levothyroxine) | Potential interaction on thyroid hormone absorption, but more research is needed | Low |
| Ashwagandha | Thyroid hormone replacement therapy (e.g., levothyroxine) | May slightly alter thyroid hormone levels, but needs more research | Low |
| Ginseng | Thyroid hormone replacement therapy (e.g., levothyroxine) | May potentially interfere with thyroid hormone absorption, but more research is needed | Moderate |
The table above presents potential interactions between herbs and thyroid medications. It’s crucial to consult with a healthcare professional to assess any possible interactions based on your specific circumstances and medications. The severity of potential interactions can vary depending on the individual and the specific combination of herbs and medications. This table is not exhaustive and should not be considered a definitive guide.
Mechanisms of Action and Interactions
Understanding how herbs interact with the thyroid system is crucial for safe and effective use. While some herbs may offer potential support, their effects on thyroid hormone production are not always predictable and can sometimes interfere with prescribed medications. A careful and informed approach, coupled with guidance from a healthcare professional, is essential.
Specific Mechanisms of Herbal Action
Herbs can potentially influence thyroid function through various mechanisms, including impacting iodine uptake, affecting thyroid hormone synthesis, and potentially modulating thyroid-stimulating hormone (TSH) levels. These interactions can be complex and not fully understood in all cases. For example, some herbs might increase iodine uptake, which could be beneficial for those with iodine deficiency, but detrimental for those with hyperthyroidism.
Similarly, herbs impacting TSH levels could influence the thyroid’s response to hormonal signals.
Certain herbs can potentially influence thyroid function, but it’s crucial to remember that they’re not a replacement for medical advice. For example, some herbs might help regulate thyroid hormones, while others could interfere with medication. A balanced diet, rich in nutrients like magnesium, is vital for overall health. Knowing which fruits contain magnesium, like bananas and avocados, can help you incorporate this important mineral into your daily intake.
What fruit has magnesium ? Ultimately, consulting with a healthcare professional is key when exploring the use of herbs to support thyroid health. They can help you navigate the potential benefits and risks.
Potential Interactions with Thyroid Medications
Herbs can interact with thyroid medications, potentially altering their effectiveness or causing adverse effects. For instance, some herbs may interfere with the absorption of thyroid hormones. Furthermore, some herbs might impact the body’s metabolism of thyroid medication, leading to fluctuations in hormone levels. These interactions can be unpredictable and require careful monitoring. It is critical to inform your doctor about all supplements and herbal remedies you are using to avoid potentially harmful drug interactions.
Potential Risks Associated with Herbal Use
Using herbs for thyroid conditions carries potential risks. Some herbs may contain compounds that interfere with thyroid hormone production or disrupt the delicate balance of thyroid hormones in the body. This can lead to unwanted side effects, exacerbating pre-existing conditions or even causing new ones. Furthermore, the quality and potency of herbal products can vary significantly, making it difficult to predict their effects accurately.
Importance of Professional Consultation
Before using any herbs for thyroid-related conditions, consulting a healthcare professional is absolutely vital. A doctor can assess your specific condition, evaluate the potential risks and benefits of using specific herbs, and determine if the herb is safe for you. They can also help you understand potential interactions with other medications you may be taking. This precaution is crucial to avoid exacerbating existing thyroid issues or causing new complications.
Comparison of Mechanisms of Action for Selected Herbs
| Herb | Mechanism | Supporting Evidence |
|---|---|---|
| Ashwagandha | Potentially modulating TSH levels, influencing thyroid hormone synthesis, and impacting oxidative stress. | Some studies suggest potential benefits, but more rigorous research is needed. |
| Ginger | May influence iodine uptake and thyroid hormone metabolism. | Limited studies exist; further research is required. |
| Kelp | High in iodine, potentially increasing iodine intake. | Should be used with caution, as excessive iodine intake can harm thyroid function in susceptible individuals. |
Research and Evidence
The use of herbs for thyroid health is a fascinating area, but robust scientific evidence is crucial to validate claims. While anecdotal experiences and traditional knowledge are valuable, rigorous research is necessary to understand the mechanisms and effects of these remedies on thyroid function. This section delves into the current state of research on herbal interventions for thyroid conditions, highlighting both promising findings and limitations in existing studies.Existing research on herbal remedies for thyroid conditions is not always comprehensive.
Often, studies are small-scale, lacking the statistical power to draw definitive conclusions. Further, there may be inconsistencies in study methodologies and reporting practices, making it difficult to compare results across different investigations. This necessitates careful evaluation of the quality and design of each study.
Current Research on Herbal Remedies and Thyroid Function
Research regarding the effects of herbs on thyroid function is ongoing, but the evidence is not always conclusive. Studies investigating the impact of specific herbs on thyroid hormone levels, or the regulation of thyroid function, are not consistently conclusive or easily comparable. Many studies are limited by small sample sizes, lack of standardization in herbal preparations, or the absence of a control group.
The importance of rigorously designed studies using standardized herbal extracts is paramount to obtain more reliable results.
Clinical Trials and Studies Investigating Herbs and Thyroid Function
Several studies have explored the potential effects of herbs on thyroid function. For example, research has investigated the impact of ashwagandha on thyroid function in individuals with hypothyroidism. However, the results are not always consistent across studies. Other studies have investigated the potential benefits of ginseng on thyroid hormone levels in healthy individuals, but more research is required to understand the long-term effects and interactions with existing medical conditions.
Strengths and Limitations of Existing Research
A key strength of some studies is the focus on specific mechanisms of action. Some studies investigate how herbs may influence thyroid hormone production or metabolism, offering potential insights into the underlying biological processes. However, limitations are often apparent in the methodology employed. These include inconsistent standardization of herbal preparations, lack of long-term follow-up, and insufficient sample sizes to draw robust conclusions.
Importance of High-Quality, Peer-Reviewed Research
High-quality, peer-reviewed research is essential for evaluating the safety and efficacy of herbal remedies. Peer review ensures that studies are rigorously scrutinized by experts in the field before publication, reducing the risk of flawed or misleading results. This process helps to establish the credibility and reliability of the research findings.
Summary Table: Research Findings on Herbs for Hypothyroidism
| Herb | Study Type | Results | Limitations |
|---|---|---|---|
| Ashwagandha | Small-scale clinical trial | Some studies suggest potential benefits in managing symptoms, but results are not consistent and often limited by sample size. | Standardized extract not always used, long-term effects not fully explored. |
| Ginseng | In vitro and animal studies | Some studies suggest potential modulation of thyroid hormone levels, but human clinical trials are lacking. | Extrapolation to humans is not always straightforward, and standardization of extracts is crucial. |
| Turmeric | In vitro studies | Preliminary evidence suggests potential anti-inflammatory effects that could indirectly benefit thyroid health. | Lack of human clinical trials on thyroid function, specific mechanisms not fully understood. |
Safety and Precautions

Using herbs for thyroid conditions can be a tempting option, but it’s crucial to approach it with caution. While many herbs show promise in supporting thyroid health, their effects aren’t always predictable, and interactions with medications or underlying health conditions can be significant. Before incorporating any herbal remedy into your thyroid management plan, consulting a healthcare professional is essential.The complexity of the human body and the individual variability in responses to herbal supplements highlight the need for personalized guidance.
Self-treating with herbs without proper medical supervision can lead to adverse effects, potentially worsening existing thyroid issues or causing new problems. It’s vital to understand the potential risks and benefits before embarking on any herbal therapy.
Potential Side Effects and Adverse Reactions
Herbal remedies, even those considered safe in general, can interact with existing medications or conditions, potentially leading to adverse effects. Certain herbs can interfere with thyroid hormone production or function, requiring careful monitoring and adjustments to treatment plans. Some herbs, if not used properly, may have negative interactions with prescription medications used to manage thyroid issues, potentially impacting the effectiveness of the medication or increasing the risk of side effects.
Individualized Treatment Plans and Professional Guidance
Thyroid conditions are highly individualized. What works for one person might not work for another, and herbal remedies are no exception. An experienced healthcare professional, preferably an endocrinologist or a practitioner with expertise in herbal medicine, can assess your specific needs and recommend appropriate herbs, dosages, and duration of use. They can also monitor your response to the treatment and make necessary adjustments.
They can also assess for potential drug interactions with existing medications.
Table of Common Herbs and Potential Side Effects
It is crucial to remember that this table is for informational purposes only and does not constitute medical advice. Always consult with a healthcare professional before using any herbal remedies for thyroid conditions.
| Herb | Potential Side Effect | Severity |
|---|---|---|
| Ashwagandha | Low blood pressure, nausea, or skin rashes | Mild to Moderate |
| Guggul | Diarrhea, indigestion, or skin irritation | Mild to Moderate |
| Coleus Forskohlii | Increased heart rate, palpitations, or insomnia | Mild to Moderate |
| Lemon Balm | Allergic reactions, such as skin rashes or hives | Mild |
| Ginger | Mild digestive upset, such as nausea or heartburn | Mild |
| Turmeric | Mild digestive upset, such as nausea or heartburn | Mild |
| Thyme | Possible interaction with blood thinners; allergic reactions | Mild to Moderate |
Diet and Lifestyle Factors
A healthy lifestyle plays a crucial role in managing thyroid conditions and supporting overall well-being. The interplay between diet, stress, exercise, and sleep significantly impacts thyroid function. Understanding these factors empowers individuals to take proactive steps toward optimal thyroid health.Proper nutrition, stress management, regular exercise, and adequate sleep are not merely beneficial adjuncts to thyroid treatment; they are integral components of a comprehensive management strategy.
By incorporating these lifestyle elements into daily routines, individuals can significantly influence their thyroid health trajectory.
Balanced Diet for Thyroid Support, How herbs can affect thyroid disease
A balanced diet rich in essential nutrients is fundamental for supporting healthy thyroid function. Iodine, selenium, zinc, and vitamins are crucial for the production and regulation of thyroid hormones. Crucially, a diet rich in fruits, vegetables, whole grains, and lean proteins provides the necessary vitamins and minerals, promoting overall health and supporting thyroid function. Avoid processed foods, excessive sugar, and refined grains, as these can negatively impact thyroid health.
Stress Management for Thyroid Conditions
Chronic stress can negatively impact the endocrine system, potentially affecting thyroid function. Implementing stress-reduction techniques like meditation, yoga, deep breathing exercises, and spending time in nature can effectively mitigate the detrimental effects of stress. These practices can help regulate cortisol levels and promote a healthier hormonal balance, which can, in turn, support thyroid health.
Exercise and Thyroid Function
Regular exercise contributes to overall health and can positively influence thyroid function. Moderate-intensity aerobic exercises, such as brisk walking, swimming, or cycling, can enhance metabolic function, improve nutrient absorption, and contribute to overall well-being. Strength training exercises, focusing on building muscle mass, also contribute to improved metabolism, supporting healthy thyroid function.
Significance of Adequate Sleep for Thyroid Function
Adequate sleep is essential for the body’s natural hormonal balance, including thyroid function. Insufficient sleep can disrupt the body’s natural rhythm and potentially affect the production and regulation of thyroid hormones. Aiming for 7-9 hours of quality sleep each night is vital for optimal thyroid health. Consistent sleep patterns are crucial for maintaining hormonal balance.
Dietary Recommendations for Thyroid Conditions
| Food Type | Nutrient Content | Benefits |
|---|---|---|
| Leafy Greens (Spinach, Kale) | Vitamins A, C, K, Folate, Iron, Calcium | Support overall health, provide essential vitamins and minerals, contribute to thyroid health |
| Fatty Fish (Salmon, Tuna) | Omega-3 Fatty Acids, Iodine, Vitamin D | Essential for thyroid hormone production, promote overall health, support healthy immune function |
| Brazil Nuts | Selenium | Crucial for thyroid hormone synthesis, supports antioxidant defense, essential for optimal thyroid function |
| Yogurt | Calcium, Protein, Probiotics | Contributes to overall health, essential for bone health, supports digestive health |
| Whole Grains (Oats, Brown Rice) | Fiber, Vitamins, Minerals | Promote healthy digestion, provide sustained energy, support overall well-being |
Note: This table provides a general overview. Consulting with a registered dietitian or healthcare professional is recommended for personalized dietary recommendations tailored to individual needs and specific thyroid conditions.
Ultimate Conclusion: How Herbs Can Affect Thyroid Disease

In conclusion, while herbs may offer potential support for thyroid health, they should not be considered a replacement for conventional medical treatments. The interplay between herbs and thyroid function is multifaceted and not fully understood. Always prioritize consultation with a healthcare professional before introducing any herbal supplements, especially if you are already taking thyroid medications. A balanced approach, combining professional medical guidance with mindful herbal choices, can be beneficial in supporting your overall thyroid well-being.
Understanding the potential risks and benefits is key to making informed decisions about your health.