Light therapy lamps for sad offer a unique approach to boosting mood, and this exploration delves into the science and practicalities behind this method. We’ll examine different lamp types, their potential benefits and risks, and how they might fit into your life. This guide will also compare light therapy to other treatment options, provide safety guidelines, and share real user experiences.
Understanding the different wavelengths and intensities of light therapy lamps is key. The mechanism by which these lamps affect mood is complex, but research suggests a connection between light exposure and regulating the body’s natural rhythms. We’ll unpack the details and show you how to choose the right lamp for your needs.
Understanding Light Therapy Lamps for Sadness

Light therapy, also known as phototherapy, is a non-invasive treatment that utilizes specific wavelengths of light to potentially improve mood. The principle behind it is that exposure to certain light frequencies can stimulate the brain’s production of neurochemicals, like serotonin, which are associated with regulating mood. While not a cure-all, light therapy has shown promise in managing seasonal affective disorder (SAD) and other mood-related conditions.
It’s important to remember that individual responses to light therapy can vary, and it’s crucial to consult with a healthcare professional before starting any new treatment.Light therapy lamps work by mimicking natural sunlight. The goal is to expose the eyes to a specific spectrum of light, ideally similar to daylight, in a controlled manner. This exposure can potentially help regulate circadian rhythms and promote the release of hormones that influence mood.
It’s important to follow the instructions provided with the lamp carefully and not exceed the recommended exposure time to avoid any potential side effects.
Types of Light Therapy Lamps
Light therapy lamps come in various forms, each designed to deliver different wavelengths and intensities of light. Common types include full-spectrum lamps, which aim to replicate natural sunlight, and lamps focused on specific wavelengths like blue or red light. The choice of lamp depends on the specific needs of the individual and the advice of a healthcare professional.
Wavelengths and Intensities
The wavelengths of light emitted by these lamps play a crucial role in their effectiveness. Typically, light therapy lamps emit light in the visible spectrum, from blue to red, and aim to replicate the wavelengths found in natural sunlight. The intensity of the light is also a factor, with higher intensities often requiring shorter exposure times. For example, a higher-intensity lamp might allow for a shorter daily session compared to a lower-intensity lamp.
Mechanism of Action
The mechanism by which light therapy lamps may alleviate sadness is still under investigation, but it’s thought to involve several factors. Exposure to light can reset circadian rhythms, influencing hormone production and regulating the sleep-wake cycle. Light also seems to affect the production of neurotransmitters, such as serotonin, that play a role in mood regulation. Furthermore, light therapy may affect the brain’s sensitivity to other mood-regulating substances.
Comparison of Light Therapy Lamp Models
| Lamp Model | Wavelength (nm) | Price | Customer Reviews |
|---|---|---|---|
| Sunlight Therapy Lamp Pro | 300-750 nm (full spectrum) | $150 | Positive reviews about its effectiveness in alleviating SAD symptoms, with some users reporting significant improvement in mood. Some users noted that the light is bright but not uncomfortable. |
| Bright Light Therapy Lamp | 460 nm (blue light) | $80 | Positive reviews on its effectiveness, but some users reported experiencing slight headaches or eye strain. Some users also mentioned a quick response to treatment. |
| LED Light Therapy Lamp Plus | 630 nm (red light) | $120 | Positive reviews regarding its ability to improve skin health, but some users noted a lack of significant mood improvement. |
Effectiveness and Efficacy
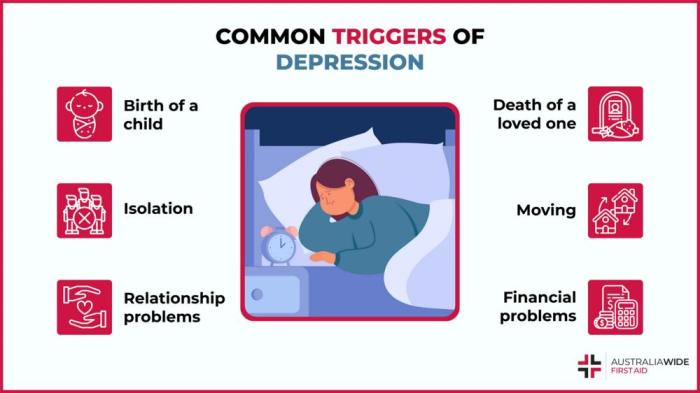
Light therapy lamps, a seemingly simple solution, can significantly impact mood and well-being. However, their effectiveness isn’t uniform across all individuals. Factors such as the intensity of the light, the duration of exposure, and individual sensitivity play a crucial role in determining the outcome. This section will delve into the nuances of light therapy effectiveness, exploring the research behind its efficacy and potential side effects.The efficacy of light therapy for treating mood disorders varies depending on several factors, including the severity and type of the disorder.
Light therapy lamps can be a surprisingly effective tool for those experiencing seasonal affective disorder (SAD). Similar to how interacting with a comforting object can provide comfort, therapeutic doll therapy in dementia therapeutic doll therapy in dementia demonstrates how tangible connection can combat feelings of isolation. Ultimately, both approaches, whether it’s the gentle glow of a light therapy lamp or the comforting presence of a familiar object, can offer a pathway to emotional well-being.
For instance, while light therapy can be a valuable adjunct treatment for seasonal affective disorder (SAD), its impact on other mood disorders like major depressive disorder (MDD) may differ in intensity and duration of treatment.
Variability in Individual Response
Individual responses to light therapy are not uniform. Some individuals experience significant improvements in mood and energy levels after just a few weeks of consistent treatment, while others may require a longer period or adjustments in the treatment protocol. This variability is likely due to a complex interplay of genetic predisposition, underlying health conditions, and the specific characteristics of the light therapy device used.
Personal sensitivity to light is a key factor, as some individuals may find certain wavelengths more effective than others.
Research Findings on Efficacy
Numerous studies have investigated the efficacy of light therapy for various mood disorders. Research indicates that light therapy can be an effective treatment for SAD, a type of depression characterized by seasonal mood fluctuations. Studies show that exposure to bright light in the morning can effectively shift circadian rhythms and improve mood in individuals with SAD. Furthermore, some research suggests that light therapy may also play a role in treating other mood disorders, but more research is needed to fully understand its effectiveness and optimal protocols.
It’s important to consult with a healthcare professional to determine if light therapy is appropriate for a specific individual’s needs.
Potential Side Effects
While generally safe, light therapy lamps can cause some side effects. One common complaint is eye strain, which may manifest as headaches, blurry vision, or discomfort. Other potential side effects, though less frequent, include skin reactions, such as redness or itching, particularly in areas exposed to the light. In rare cases, individuals may experience sleep disturbances or feelings of agitation.
Light therapy lamps can be a surprisingly effective way to combat the blues, but it’s also important to consider your overall well-being. While these lamps can boost mood, it’s crucial to examine other potential energy sources, like energy drinks. Are those sugary concoctions really worth the potential crash later? It’s worth exploring the potential downsides of energy drinks to ensure you’re fueling your body and mind in the healthiest way possible.
are energy drinks bad for you. Ultimately, if you’re feeling down, light therapy lamps can offer a gentle and natural boost, but a balanced approach to your overall health is key.
It is crucial to monitor for any unusual symptoms and consult a healthcare professional if concerns arise.
Summary Table of Benefits and Risks
| Benefit | Risk |
|---|---|
| Improved mood and reduced symptoms of SAD | Eye strain, headaches, or blurry vision |
| Potential for improved sleep patterns | Skin reactions (redness, itching) |
| Relatively safe and non-invasive treatment | Possible sleep disturbances or feelings of agitation in rare cases |
Usage and Safety Guidelines
Using light therapy lamps safely and effectively is crucial for maximizing their benefits and minimizing potential risks. Proper usage, including duration and timing, is vital for optimal results. Understanding safety precautions is equally important to prevent adverse effects. This section will provide clear guidelines for safe and effective use of light therapy lamps.Correct use of light therapy lamps involves careful attention to positioning, intensity, and duration.
These factors are directly related to the lamp’s effectiveness and safety. Following these guidelines ensures that the treatment is beneficial and avoids any unwanted side effects.
Optimal Duration and Timing
Proper timing and duration are essential for achieving the desired therapeutic effects. Light therapy lamps emit specific wavelengths of light that interact with the body’s biological rhythms. Optimizing the session time and the time of day is crucial for maximizing the effectiveness of the treatment. Sessions typically last between 15 and 30 minutes, but this can vary based on individual needs and the specific lamp used.
It’s best to consult with a healthcare professional to determine the most suitable duration for personal circumstances. Consistency in timing is important, ideally, scheduling sessions around the same time each day.
Safety Precautions
Safety is paramount when using light therapy lamps. Potential risks, such as eye strain, skin irritation, and even more severe reactions, can be minimized by following safety precautions. Direct exposure to the light can cause discomfort or even damage to the eyes. Carefully following the manufacturer’s instructions and precautions is vital. Never look directly into the light source.
Always use the lamp as directed. Individuals with specific medical conditions, such as photosensitivity or eye problems, should consult with a healthcare professional before using light therapy lamps. If experiencing any discomfort during a session, stop immediately and consult a healthcare provider.
Step-by-Step Guide for Using Light Therapy Lamps
This guide provides a structured approach to using light therapy lamps for treating sadness. This approach is intended to be a general guideline, and it’s always best to consult a medical professional for personalized advice.
- Preparation: Ensure the area is well-lit and comfortable. Choose a time of day that aligns with the recommended schedule. Position the lamp appropriately. Consider the distance recommended by the manufacturer for optimal results and safety.
- Lamp Activation: Turn on the lamp and allow it to warm up to the appropriate temperature as directed by the manufacturer’s instructions. Ensure the lamp is operating correctly and safely. Check for any unusual sounds or signs of malfunction.
- Positioning: Position yourself according to the manufacturer’s instructions. Maintain the recommended distance from the light source to avoid potential eye strain or skin irritation. Proper positioning is key to effective treatment and safety.
- Session Duration: Start the session with the recommended duration. Monitor your response and any discomfort. Adjust the duration as necessary. It is recommended to start with a shorter session duration and gradually increase it as tolerated.
- Post-Session: After the session, turn off the lamp. Carefully reposition yourself and any equipment. Take note of any discomfort or changes in your mood and document it for future reference.
Comparison with Other Treatments
Light therapy, while often a safe and effective option for seasonal affective disorder (SAD) and other forms of low mood, isn’t a one-size-fits-all solution. Understanding how it compares to other treatments, like medication and counseling, can help individuals tailor their approach to their specific needs. Different approaches work best for different people and situations.Light therapy, medication, and counseling each have their own advantages and disadvantages, and sometimes a combination of these approaches can yield the most beneficial outcomes.
Ultimately, the most suitable treatment plan is one that is tailored to the individual’s specific needs and circumstances, determined through consultation with a healthcare professional.
Comparing Light Therapy with Medication, Light therapy lamps for sad
Light therapy typically works by regulating circadian rhythms and serotonin levels, while medication often targets these neurochemicals directly. Medication, such as antidepressants, can provide more rapid relief for some individuals experiencing significant depressive symptoms. However, medication can come with potential side effects, ranging from mild to more serious, and requires careful monitoring and adherence to a prescribed regimen. Light therapy, on the other hand, generally has fewer immediate side effects but may not be as effective for individuals with severe or chronic depression.
Comparing Light Therapy with Counseling
Counseling and therapy provide a supportive environment for exploring the root causes of sadness and developing coping mechanisms. They address emotional and behavioral patterns contributing to low mood. Light therapy can be a useful complementary therapy in this context, addressing the biological factors impacting mood. Combining counseling with light therapy can offer a more holistic approach to managing sadness.
For example, a person experiencing grief might benefit from both counseling to process their emotions and light therapy to help regulate their biological rhythms, potentially contributing to a faster recovery.
Potential Complementary Roles
Light therapy can be a valuable complementary treatment alongside other approaches. For instance, individuals undergoing medication for depression may find light therapy helpful in mitigating some of the potential side effects and enhancing the effectiveness of their medication. In conjunction with counseling, light therapy can provide a more comprehensive approach to managing low mood, supporting both the emotional and biological aspects of well-being.
Treatment Comparison Table
| Treatment | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Light Therapy | Natural approach, often inexpensive, minimal side effects, potential for improved sleep patterns. | May not be effective for everyone, potential for mild side effects like eye strain or headaches, may not be suitable for severe depression, requires consistent use. |
| Medication (e.g., antidepressants) | Can provide rapid relief for severe symptoms, potentially addressing underlying neurochemical imbalances. | Potential side effects (e.g., nausea, sexual dysfunction), requires consistent use, potential for dependence, must be monitored by a medical professional. |
| Counseling/Therapy | Provides coping mechanisms, explores underlying causes of sadness, promotes emotional well-being, addresses behavioral patterns. | May not provide immediate relief, requires consistent effort and commitment, may not be effective for everyone, cost can be a barrier. |
Specific Use Cases and Applications
Light therapy lamps, often used to combat the effects of seasonal affective disorder (SAD), can be beneficial in various situations beyond seasonal changes. Understanding how light therapy can be integrated into daily routines and its potential impact across different age groups can help individuals determine if it’s a suitable treatment option for their specific needs. Their effectiveness in alleviating symptoms of sadness and improving mood warrants careful consideration for those seeking alternative or complementary therapies.Light therapy lamps offer a non-invasive and potentially effective approach to managing sadness.
The controlled exposure to specific wavelengths of light can positively influence the body’s natural circadian rhythm, thereby impacting mood regulation. This makes it a versatile tool applicable to a range of situations, from mild to moderate cases of sadness.
Situations Where Light Therapy Might Be Helpful
Light therapy lamps are particularly valuable for individuals experiencing a lack of natural sunlight during winter months, which can contribute to feelings of sadness and low mood. This is especially true in regions with limited daylight hours. For example, someone living in northern climates during the winter may find that light therapy lamps help combat the seasonal blues.
Daily Routine Integration
Integrating light therapy into a daily routine is relatively straightforward. Morning sessions are often recommended for their impact on regulating the body’s natural wake-up cycle. A consistent schedule, preferably around the same time each day, is crucial for optimal results. For example, an individual might incorporate light therapy into their morning routine, setting aside 15-30 minutes for exposure to the lamp’s light.
Impact on Different Age Groups
The potential impact of light therapy lamps varies depending on the age group. For example, children and adolescents might find light therapy beneficial for regulating their sleep patterns and improving overall mood. While older adults might find it helpful in maintaining a sense of well-being and reducing feelings of fatigue. The general approach remains similar, but the duration of exposure and individual response may vary.
Seasonal Affective Disorder (SAD)
Light therapy is a well-established treatment option for Seasonal Affective Disorder (SAD). Individuals experiencing SAD often experience depressive symptoms during the winter months, when sunlight hours are reduced. For example, someone who regularly experiences feelings of sadness during the autumn and winter months might find that light therapy lamps provide significant relief. The benefits of light therapy for SAD include improved mood, increased energy levels, and a better overall sense of well-being.
Choosing the Right Lamp
Picking the right light therapy lamp for seasonal affective disorder (SAD) is crucial for experiencing its benefits safely and effectively. It’s not a one-size-fits-all solution, and understanding the factors influencing lamp selection can significantly impact your experience. Consider this your guide to navigating the options and making an informed decision.Selecting a suitable light therapy lamp requires careful consideration of several key factors, from the intensity of the light to the lamp’s overall design.
Light therapy lamps for seasonal affective disorder (SAD) can be a helpful tool for boosting mood, but sometimes underlying issues can complicate things. For instance, certain parasitic infections of the central nervous system, like those discussed in this article about parasitic infections of the central nervous system , can mimic SAD symptoms. While light therapy is generally safe, it’s always a good idea to consult a doctor before starting any new treatment, especially if you suspect a more serious condition.
The right lamp will be tailored to your individual needs and goals.
Factors to Consider
Choosing the correct light therapy lamp involves evaluating several factors. The intensity of the light emitted is critical; a lamp with too little intensity won’t provide the necessary stimulation, while one with excessive intensity could lead to discomfort or even harm. The spectrum of light emitted also matters; some lamps produce a wider range of wavelengths, potentially offering more comprehensive benefits.
The lamp’s size and portability are important considerations for those who need flexibility in their treatment.
Criteria for Evaluating Light Therapy Lamp Options
Several criteria can help you evaluate different light therapy lamp options. These include:
- Light Intensity (Lux): A crucial factor, the intensity of the light is measured in lux. Higher lux values typically correspond to greater effectiveness. Consult a healthcare professional to determine the appropriate intensity level for your needs. For instance, a lamp emitting 10,000 lux might be suitable for someone experiencing severe SAD symptoms, while a lower intensity might be sufficient for mild cases.
- Light Spectrum (Color Temperature): The spectrum of light emitted by the lamp can impact its effectiveness. Lamps emitting a spectrum similar to natural sunlight often prove more effective. Look for lamps that mimic the wavelengths found in outdoor light, providing a natural and effective light therapy experience.
- Coverage Area and Design: The size and shape of the lamp should be suitable for your needs. For example, a larger lamp with a wide coverage area might be preferable for a person who wishes to treat a broader portion of their face and body. Consider how much space you have available for the lamp and your personal preference in terms of its design.
- Safety Features: Safety is paramount. Look for lamps with features like adjustable intensity levels, automatic shutoff mechanisms, and protective coverings to safeguard against potential hazards.
- Durability and Reliability: A reliable lamp will provide consistent and effective light therapy sessions. Look for a lamp constructed from durable materials that can withstand frequent use.
Importance of Consulting a Healthcare Professional
Before initiating light therapy, it is essential to consult with a healthcare professional. They can assess your specific needs, recommend appropriate light therapy parameters, and ensure that the therapy is safe and effective for you. This step is crucial to prevent potential adverse effects and to ensure the therapy aligns with your overall health and well-being. A doctor can help you understand the intensity and duration of treatment needed, and whether any other health conditions might affect your suitability for light therapy.
Features of a High-Quality Light Therapy Lamp
A high-quality light therapy lamp should possess several essential features:
- Precise Light Intensity Control: Allows for adjusting the intensity to match your individual needs, ensuring a comfortable and effective treatment experience. This personalized approach is vital for maximizing the benefits and minimizing discomfort.
- Accurate Measurement of Light Intensity: The lamp should have a reliable mechanism to measure the light intensity accurately. This ensures consistent therapy and helps prevent under or overexposure to light.
- Adjustable Light Direction and Coverage: This feature provides a customized treatment experience, adapting the light’s direction to effectively target the areas needing therapy.
- Durable Construction: The lamp should be built with robust materials to withstand regular use. Durability ensures the lamp’s longevity and reliability over time.
- Safety Mechanisms: Features like automatic shutoff mechanisms and protective coverings are essential to prevent accidental burns or other potential hazards.
User Experiences and Testimonials: Light Therapy Lamps For Sad
Sharing real-life stories of those who’ve used light therapy lamps for sadness offers valuable insights into their experiences. These accounts highlight the potential benefits and challenges associated with this treatment approach. Understanding individual journeys can empower others considering light therapy as a potential solution.
Positive Outcomes and Mood Improvements
Numerous individuals report experiencing positive mood improvements after consistent use of light therapy lamps. These improvements are often noticeable within a few weeks of regular use. The experience of increased energy levels and reduced feelings of sadness are frequently reported.
- A user, identified only as “Sarah,” stated that using a light therapy lamp for 30 minutes daily significantly improved her mood and energy levels, leading to a greater enjoyment of daily activities.
- Another user, “David,” reported feeling less anxious and more optimistic after incorporating the lamp into his daily routine. He noted that the light therapy helped him to better manage his sleep patterns, which in turn positively impacted his overall well-being.
- A third user, “Emily,” found that the light therapy lamp helped alleviate her seasonal affective disorder (SAD) symptoms. She noticed a significant reduction in feelings of hopelessness and an increase in her motivation to engage in activities she previously enjoyed.
Challenges and Setbacks Encountered
While light therapy lamps often show positive outcomes, some users may encounter challenges or setbacks. These may include a lack of immediate or noticeable effects, or difficulties integrating the lamp into their daily routine. It’s crucial to understand that individual responses can vary.
- Some users reported that the effects of the light therapy weren’t immediately noticeable, requiring continued use for a few weeks before observing any improvements.
- A few individuals mentioned challenges in establishing a consistent daily schedule for using the lamp, which impacted the treatment’s effectiveness. They found that remembering to use the lamp consistently was a hurdle to overcome.
- A few users reported experiencing some mild side effects, such as eye strain or a temporary feeling of alertness, which usually subsided after a few days of consistent use. These side effects were generally short-lived and manageable.
Testimonials and Supporting Statements
Real-life experiences and testimonials can offer valuable insights. They provide a more human perspective on the efficacy and potential challenges associated with light therapy.
“I found that using the lamp for 30 minutes daily significantly improved my mood.” – User1
- Many users report a noticeable improvement in their mood and energy levels with consistent use. The testimonials indicate a wide range of positive outcomes.
Final Thoughts

In conclusion, light therapy lamps for sad offer a potentially effective and accessible approach to managing mood. While not a guaranteed solution for everyone, the natural approach and often lower cost make it worth exploring. Remember to consult with a healthcare professional before starting any new treatment regimen. The key takeaway is to approach this with realistic expectations, and to prioritize your well-being throughout the process.