The history of surgery timeline sets the stage for this enthralling narrative, offering readers a glimpse into the evolution of surgical techniques throughout history. From ancient civilizations to modern marvels, this journey explores the incredible advancements, the courageous pioneers, and the constant quest for better healing. We’ll uncover the fascinating stories behind the development of surgical procedures, the innovative tools and materials used, and the profound impact on human health.
This timeline traces the remarkable progress in surgical practices across different eras. It will highlight the ingenuity of early surgeons, the influence of scientific breakthroughs, and the pivotal role of anatomy and physiology in shaping modern surgical approaches. We’ll examine the development of crucial surgical innovations and the ongoing quest to improve surgical outcomes.
Early Surgical Practices
The history of surgery stretches back millennia, with ancient civilizations developing rudimentary yet surprisingly effective techniques for treating injuries and illnesses. These early practices, though vastly different from modern procedures, offer valuable insights into the evolution of medical knowledge and the human desire to alleviate suffering. From the meticulous embalming practices of ancient Egypt to the complex surgical knowledge of the Greeks, early civilizations laid the groundwork for the field of surgery we know today.
Surgical Techniques in Ancient Civilizations
Ancient surgical practices varied considerably across different cultures. Egyptian surgeons, for example, demonstrated a remarkable understanding of anatomy, likely derived from their extensive mummification rituals. Mesopotamian medical texts, such as the Edwin Smith Papyrus, reveal a more systematic approach to diagnosis and treatment, with specific procedures described for various injuries. Greek physicians, particularly those in the Hippocratic tradition, emphasized observation and a more holistic approach to healing, incorporating philosophical and ethical considerations alongside practical techniques.
These differing approaches highlight the diverse cultural contexts that shaped the development of early surgery.
Tools and Materials Used in Early Procedures
The tools and materials available to ancient surgeons were limited by the technology of their time. Egyptian surgeons, for instance, used bronze scalpels, bone instruments, and even sharpened obsidian blades for incisions. Mesopotamian texts describe the use of stone instruments, as well as bone and bronze tools for treating wounds. Greek physicians often relied on similar materials, with bronze or iron tools, along with bone and metal instruments for specific tasks.
The choice of materials and the design of tools influenced the precision and effectiveness of surgical interventions.
Comparison of Surgical Practices Across Cultures
While ancient surgical practices shared some commonalities, significant differences existed between civilizations. Egyptian surgeons, known for their embalming procedures, possessed a detailed knowledge of anatomy. Mesopotamian surgeons, as evident from the Edwin Smith Papyrus, focused on practical procedures and diagnosis. Greek surgeons, in contrast, emphasized a more holistic approach to healing, incorporating philosophical and ethical considerations into their practice.
These differences reflect the unique cultural values and priorities of each civilization.
Examples of Surgical Treatments in Ancient Times
Ancient surgical treatments addressed a wide range of ailments. Egyptian medical texts describe treatments for fractures, wounds, and even some forms of eye diseases. Mesopotamian medical records reveal procedures for treating head injuries, wounds, and abscesses. Greek physicians documented treatments for various injuries and illnesses, including fractures, dislocations, and surgical procedures for specific ailments. These examples demonstrate the diverse range of conditions that ancient surgeons attempted to treat, highlighting their ingenuity and resilience.
Major Surgical Procedures in Ancient Civilizations
| Civilization | Procedure | Description | Tools |
|---|---|---|---|
| Egypt | Trepanation | Drilling a hole in the skull to relieve pressure or treat head injuries. | Bronze or bone instruments, obsidian blades. |
| Mesopotamia | Wound Treatment | Cleaning and bandaging of wounds, treatment of fractures. | Stone, bone, and bronze instruments. |
| Greece | Amputation | Removal of a limb due to injury or disease. | Bronze or iron tools, bone instruments. |
The Evolution of Surgical Techniques
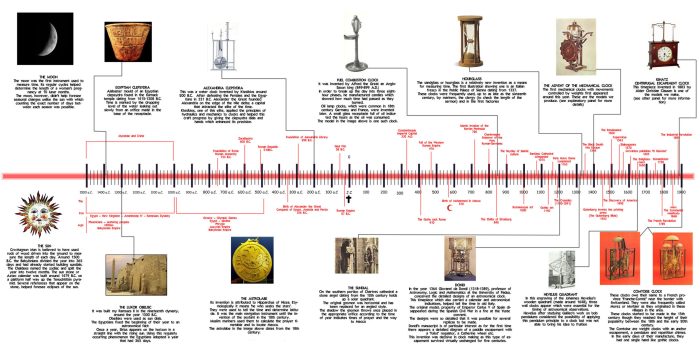
Surgical practice, from its earliest forms to the modern era, reflects a fascinating journey of innovation and adaptation. Driven by necessity and fueled by a thirst for understanding the human body, surgeons have constantly refined their methods, improving outcomes and expanding the boundaries of what’s possible. This evolution is deeply intertwined with scientific progress, medical advancements, and the contributions of influential figures.The progression of surgical techniques is a testament to the relentless pursuit of knowledge and the tireless efforts of those dedicated to healing.
From rudimentary procedures to sophisticated operations, the development of surgical methods mirrors the broader advancements in scientific understanding, particularly in anatomy and physiology. This evolution has not only enhanced the safety and effectiveness of surgical interventions but also broadened the scope of treatable conditions.
Impact of Scientific Advancements
Scientific advancements have profoundly shaped surgical techniques. The discovery of anesthesia, for instance, revolutionized surgical procedures, enabling surgeons to perform operations without the excruciating pain previously endured by patients. Similarly, the development of sterile techniques, based on microbiological understanding, dramatically reduced the risk of infection, a major cause of mortality in earlier surgical practices. The meticulous study of human anatomy and physiology has provided a deeper understanding of the body’s intricate workings, leading to more precise and targeted surgical interventions.
The use of imaging technologies like X-rays and CT scans has further improved surgical precision, allowing surgeons to visualize internal structures before and during operations.
Contributions of Key Figures
Numerous individuals have significantly contributed to the development of surgical techniques. William Halsted, a renowned surgeon in the late 19th and early 20th centuries, pioneered advancements in surgical techniques and surgical training. His meticulous attention to detail and commitment to asepsis (sterile techniques) dramatically improved surgical outcomes. Joseph Lister, a British surgeon, made significant contributions to antiseptic surgery, demonstrating the importance of preventing infection during surgical procedures.
His work built upon the burgeoning field of microbiology, significantly altering surgical practices and saving countless lives. These figures, among others, played crucial roles in advancing the art and science of surgery.
Comparison of Surgical Methods
Surgical methods differed considerably between the ancient period, the Middle Ages, and the Renaissance. Ancient surgical techniques, often relying on rudimentary instruments and limited understanding of anatomy, focused primarily on addressing external injuries and wounds. The Middle Ages saw a decline in surgical knowledge in some regions, with reliance on traditional practices and a lack of significant anatomical advancements.
The Renaissance marked a turning point, with renewed interest in human anatomy, leading to more sophisticated surgical instruments and procedures. The rediscovery and study of classical texts, like those of Galen, played a vital role in this transition.
Role of Anatomy and Physiology
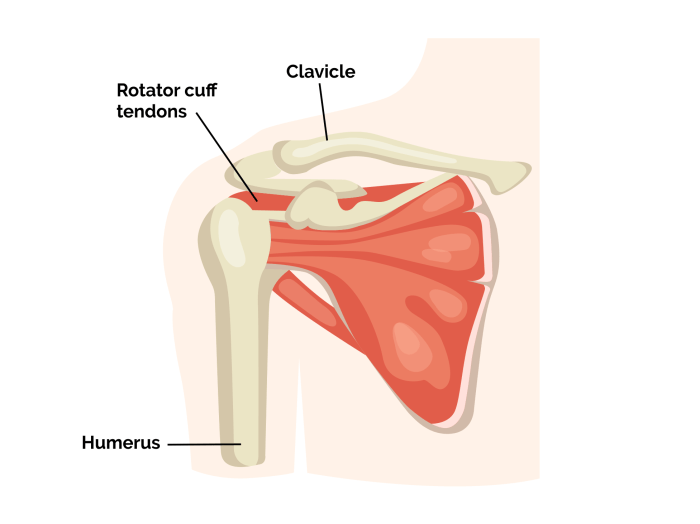
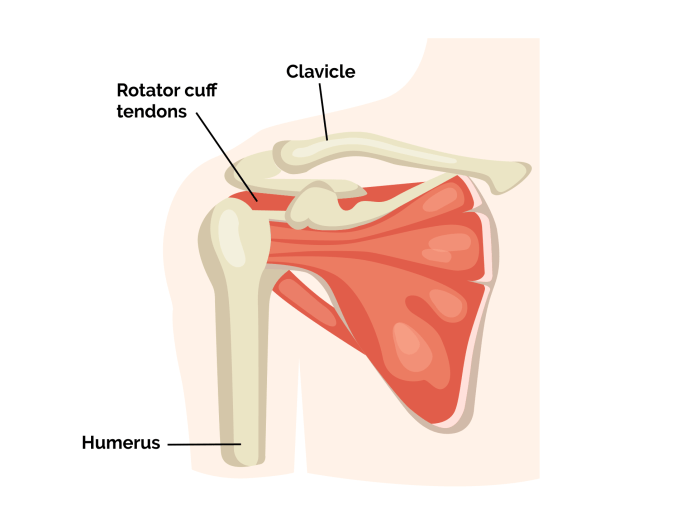
The evolution of surgery is intrinsically linked to the study of anatomy and physiology. A deeper understanding of the human body’s structure and function allowed surgeons to develop more precise and targeted procedures. Knowledge of the circulatory system, for example, facilitated the development of techniques for blood vessel repair and cardiovascular surgeries. The detailed study of tissues and organs allowed surgeons to understand the effects of surgical interventions and to refine their techniques accordingly.
Anatomical studies provided the foundation for surgical procedures, and physiological knowledge enabled a better comprehension of the body’s response to surgical trauma.
Timeline of Surgical Techniques
| Period | Event | Description | Key Figure |
|---|---|---|---|
| Ancient Egypt (c. 3000 BCE) | Trepanation | Drilling holes in the skull to treat various ailments. | Unknown |
| Ancient Greece (c. 500 BCE) | Hippocrates | Emphasis on observation and diagnosis. Development of surgical instruments. | Hippocrates |
| Medieval Europe (c. 500-1500 CE) | Decline in anatomical knowledge | Surgical practices often relied on traditional methods and limited understanding of human anatomy. | Various |
| Renaissance (c. 1400-1600 CE) | Vesalius’s anatomical work | Andreas Vesalius’s accurate anatomical drawings and dissections corrected errors in Galen’s work, paving the way for more precise surgery. | Andreas Vesalius |
| 19th Century | Anesthesia and Antiseptics | The introduction of anesthesia and antiseptic techniques revolutionized surgical procedures, reducing pain and infection risks. | William Morton, Joseph Lister |
| 20th Century | Imaging and Minimally Invasive Techniques | Developments in imaging techniques (X-rays, CT scans) and minimally invasive surgical procedures improved precision and recovery times. | Numerous |
Surgical Innovations and Discoveries
The 18th and 19th centuries witnessed a dramatic transformation in surgical practices, driven by groundbreaking innovations in instruments, techniques, and understanding of the human body. These advancements were critical in paving the way for modern surgery, fundamentally changing the approach to treating disease and injury. The development of anesthesia, sterilization, and improved surgical instruments drastically reduced patient suffering and mortality.
Surgical Instruments and Techniques
Significant progress in surgical instruments occurred during this period. The development of more precise and versatile tools allowed for more delicate and effective procedures. Metal became a more common material in surgical instruments, leading to improvements in durability and functionality. Furthermore, designs began to incorporate ergonomic principles, enhancing surgeon comfort and control during operations. These developments reflected a growing understanding of anatomy and the specific needs of different surgical procedures.
Impact of Anesthesia
The discovery and application of anesthesia revolutionized surgical practice. Prior to the widespread use of anesthesia, surgical procedures were often incredibly painful and traumatic experiences for patients. The introduction of ether and chloroform as anesthetic agents allowed surgeons to perform more extensive and complex operations, leading to a significant reduction in patient suffering. This dramatic shift in patient experience allowed for greater precision and efficiency in surgical procedures.
For instance, the ability to perform prolonged operations without the patient experiencing excruciating pain opened up new avenues in surgical intervention.
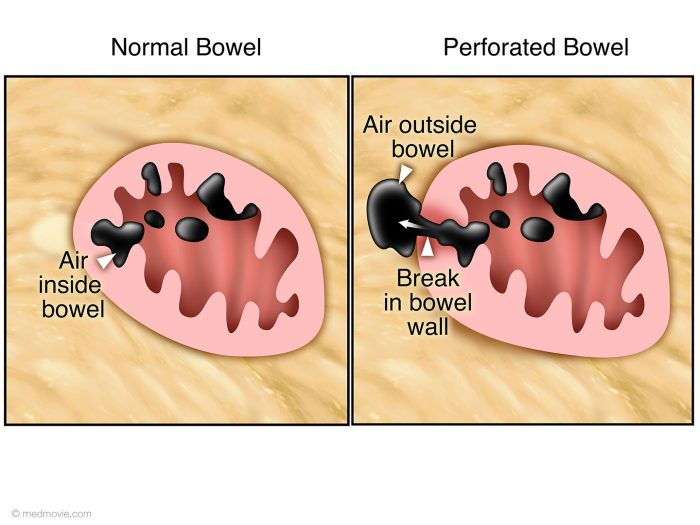
Development of Sterilization Techniques
The understanding of the role of infection in surgical complications spurred the development of sterilization techniques. Before the advent of antiseptic procedures, surgical wounds were frequently infected, leading to high mortality rates. The pioneering work of Joseph Lister, who advocated for the use of carbolic acid as a disinfectant, marked a turning point in surgical practice. Lister’s meticulous attention to surgical cleanliness significantly reduced post-operative infections and drastically improved surgical outcomes.
This change in approach demonstrably improved the success rates of various surgical interventions.
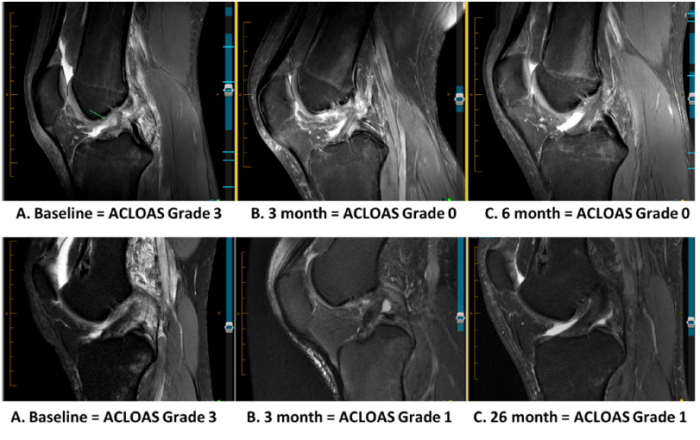
Evolution of Surgical Approaches to Specific Body Systems, The history of surgery timeline
Surgical approaches to various body systems underwent substantial changes. In cardiovascular surgery, the development of techniques for blood vessel repair and heart valve replacement represented major advances. Neurological surgery saw the development of procedures for treating brain tumors and other neurological disorders. These developments were driven by an increasing understanding of the complex functions of these systems, allowing for more targeted and effective surgical interventions.
For instance, improved surgical techniques for brain tumors became possible due to a better understanding of brain anatomy and improved surgical instruments.
Comparison of Surgical Approaches for Appendectomy
| Period | Approach | Description | Advantages/Disadvantages |
|---|---|---|---|
| Pre-1800s | Open | Large incision made to directly access the appendix. | Advantages: Relatively straightforward. Disadvantages: High risk of infection, significant pain, long recovery time. |
| Late 1800s | Open | Improved techniques for incision and wound closure, but still a large incision. | Advantages: Improved wound management, reduced infection risk compared to earlier times. Disadvantages: Still a major surgical procedure. |
| Early 1900s | Laparoscopic | Small incisions using specialized instruments and video visualization. | Advantages: Minimally invasive, less pain, faster recovery. Disadvantages: Requires specialized training, potentially more complex technique. |
| Modern | Robotic-assisted | Utilizes robotic arms for enhanced precision and dexterity. | Advantages: Extreme precision, improved visualization, potentially less scarring. Disadvantages: High initial cost, requires specialized equipment and training. |
Modern Surgical Practices: The History Of Surgery Timeline
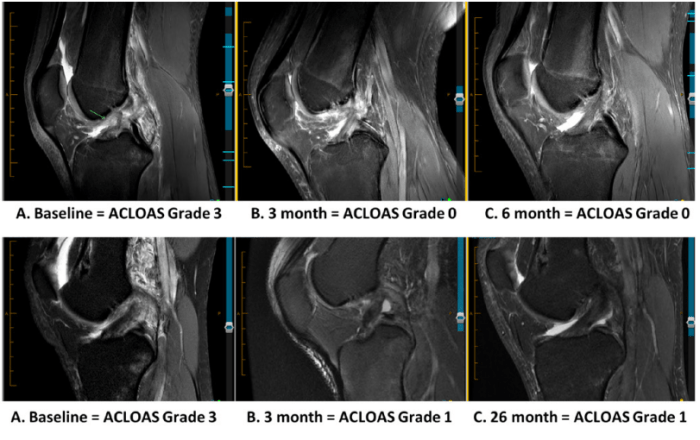
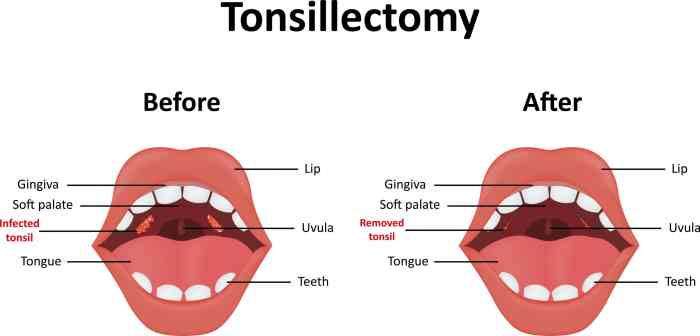
The 20th and 21st centuries witnessed a dramatic transformation in surgical practices, driven by technological advancements, a deeper understanding of the human body, and a shift towards evidence-based medicine. Surgical procedures became increasingly precise, less invasive, and safer, ultimately leading to improved patient outcomes. This era also saw the rise of specialized surgical fields, each focusing on particular areas of the body or types of procedures.
Advancements in Surgical Technology
Modern surgical technology has revolutionized the field, enabling more precise and less invasive procedures. Microsurgery, utilizing specialized instruments and magnification, allows for intricate operations on small structures, such as blood vessels and nerves. Laparoscopic surgery, employing small incisions and specialized cameras, minimizes trauma and recovery time for many procedures. Robotic surgery, incorporating advanced robotic arms and 3D visualization, provides enhanced dexterity, precision, and control, expanding the scope of minimally invasive surgery.
Impact of Medical Imaging
Medical imaging techniques have become integral to surgical planning and execution. Techniques like X-rays, CT scans, MRIs, and ultrasounds provide detailed anatomical information, enabling surgeons to visualize internal structures and assess the extent of pathology before surgery. This pre-operative imaging facilitates accurate surgical planning, allowing surgeons to develop tailored surgical strategies, potentially reducing complications and improving outcomes. Furthermore, intraoperative imaging allows for real-time visualization during surgery, enhancing precision and facilitating precise tissue dissection.
Tracing the history of surgery through time is fascinating, revealing remarkable advancements. From ancient trepanations to modern robotic procedures, the timeline is a testament to human ingenuity. However, understanding the trajectory of a disease like Parkinson’s, especially at its end stage, is also critical. Knowing the hospice criteria for end-stage Parkinson’s disease, for instance, end stage Parkinson’s disease hospice criteria , helps provide crucial support and care for patients and families.
This knowledge complements the broader historical context of surgical development.
Role of Evidence-Based Medicine
Evidence-based medicine plays a crucial role in modern surgical practice. Surgical procedures are continually evaluated and refined based on rigorous clinical trials and research. This rigorous evaluation leads to the adoption of techniques and approaches that have been proven effective and safe. The focus on data-driven decision-making has led to improvements in patient safety and surgical outcomes, reducing the incidence of complications and improving patient recovery times.
Surgeons are expected to stay updated on the latest research and clinical guidelines to ensure they are employing the most effective and evidence-supported strategies.
Key Surgical Specialties
Numerous surgical specialties cater to diverse needs. Cardiothoracic surgeons focus on the heart and lungs, performing complex procedures like heart transplants and valve replacements. Neurosurgeons address conditions affecting the brain and spinal cord, undertaking delicate operations for tumors, trauma, and other neurological disorders. General surgeons provide comprehensive surgical care for a broad range of conditions, while orthopedic surgeons specialize in musculoskeletal issues, addressing injuries and conditions affecting bones, joints, and muscles.
Ophthalmologists, though often considered medical specialists, perform many surgical procedures for eye conditions.
Surgical Techniques for Specific Conditions
Minimally invasive techniques are increasingly employed for various conditions. Hernia repair, for instance, can be performed laparoscopically or robotically, resulting in smaller incisions, less pain, and quicker recovery times compared to traditional open procedures. Similarly, gallbladder removal, appendectomy, and many other procedures are increasingly performed using minimally invasive approaches.
Impact of Technologies on Surgical Outcomes
| Technology | Application | Benefits | Limitations |
|---|---|---|---|
| Microsurgery | Fine-scale procedures on blood vessels, nerves, and tissues | Increased precision, improved outcomes in delicate procedures | Requires specialized training and equipment, potentially longer operating time |
| Laparoscopic Surgery | Minimally invasive procedures for various organs | Smaller incisions, less pain, quicker recovery | Limited dexterity compared to open surgery, not suitable for all procedures |
| Robotic Surgery | Enhanced precision, 3D visualization, tremor reduction | Improved accuracy, reduced surgeon fatigue, potential for remote surgery | High initial cost, potential for technical malfunctions, requires specialized training |
| Medical Imaging (CT, MRI, Ultrasound) | Pre-operative planning, intraoperative guidance | Accurate diagnosis, improved surgical planning, real-time visualization | Radiation exposure (CT), potential for contrast reactions (MRI), limitations in real-time resolution |
Surgical Procedures Through Time
Surgical procedures have evolved dramatically over the centuries, reflecting advancements in medical understanding, technology, and surgical techniques. From rudimentary attempts to address injuries and illnesses to sophisticated operations utilizing advanced instruments and anesthesiology, the journey of surgery is a testament to human ingenuity and resilience. This evolution is not just about the tools, but also the profound shift in our understanding of the human body and the ways we can intervene to heal.The progression of surgical techniques has been deeply intertwined with the broader societal and technological contexts of each era.
Changes in materials, sterilization practices, and the understanding of anatomy and physiology have continuously refined surgical approaches. This section explores the historical development of specific surgical procedures, highlighting the challenges and successes encountered along the way.
Cataract Surgery
The treatment of cataracts, a clouding of the eye’s lens, showcases the evolution of surgical intervention. Early attempts were often crude and ineffective, leading to significant vision loss or blindness in many cases.
Tracing the history of surgical techniques reveals fascinating advancements over time. From ancient trepanations to modern robotic procedures, surgical innovation has dramatically improved patient outcomes. Understanding these historical milestones is crucial to appreciating the complexity of modern procedures, such as those used to treat prostate cancer, particularly the different types of prostate cancer. This knowledge also helps us appreciate the long journey of surgical progress and the tireless efforts of surgeons throughout history.
“Ancient Egyptian texts describe attempts to remove cataracts, though the methods were rudimentary and often resulted in further damage.”
Early methods often involved attempts to manually remove the clouded lens, which were inherently dangerous and frequently unsuccessful. The development of better surgical instruments and an understanding of eye anatomy paved the way for more precise and effective techniques. Modern cataract surgery employs phacoemulsification, a minimally invasive procedure that precisely removes the clouded lens and replaces it with an artificial intraocular lens, significantly improving visual acuity and quality of life.
Fracture Repair
The treatment of fractures, broken bones, demonstrates a progression from basic stabilization to complex procedures.
“In ancient civilizations, fractures were often treated with splints made of various materials, such as wood or animal bones.”
Early attempts focused on stabilizing the broken bone using external supports, like splints. The understanding of bone healing and fracture mechanics evolved over time, leading to the development of more advanced techniques. Modern fracture repair incorporates the use of specialized plates, screws, and other internal fixation devices, ensuring accurate alignment and promoting rapid healing. The introduction of imaging techniques like X-rays significantly enhanced the ability to diagnose and treat fractures effectively.
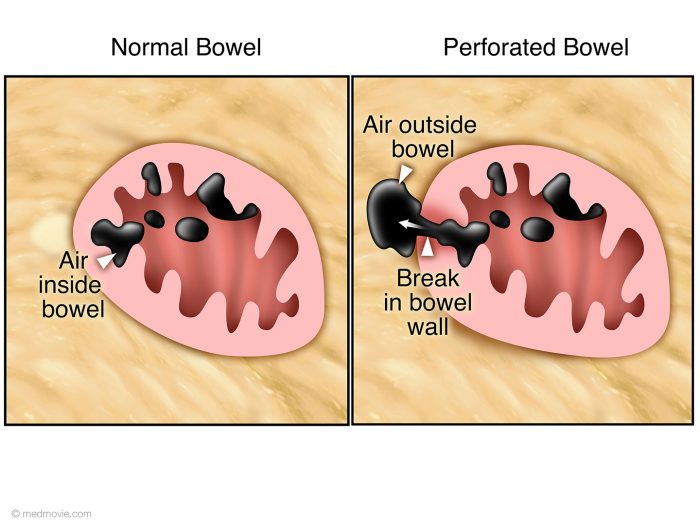
Appendicitis
Appendicitis, an inflammation of the appendix, has presented unique challenges in surgical intervention.
“The early surgical treatment of appendicitis was fraught with significant risk due to a lack of understanding of the condition and the limitations of surgical techniques.”
Early interventions were often limited to attempts at conservative treatment. The recognition of appendicitis as a surgical emergency and the development of effective surgical techniques and sterilization practices drastically improved the outcome. Modern appendectomy procedures, performed laparoscopically, minimize incisions, reduce recovery time, and greatly improve patient outcomes.
Evolution of Surgical Methods and Challenges
| Era | Surgical Method | Challenges | Successes |
|---|---|---|---|
| Ancient Egypt | Rudimentary attempts at lens extraction, bone setting | Lack of anesthesia, sterilization, and understanding of anatomy | Limited success, some cases of stabilization |
| Medieval Europe | Bleeding, cauterization, use of crude instruments | High infection rates, lack of understanding of the body’s healing mechanisms | Limited interventions, some success with simple procedures |
| Modern Era | Phacoemulsification, internal fixation, laparoscopy | Minimally invasive techniques, new materials and technologies | High success rates, reduced recovery times, improved patient outcomes |
The table above highlights the progression of surgical methods across different eras, emphasizing the significant challenges and remarkable successes in the evolution of surgical interventions.
Surgical Instruments and Materials
Surgical instruments have undergone a remarkable transformation from crude tools to sophisticated precision instruments. This evolution mirrors the broader advancement of medical knowledge and technological capabilities. The materials used, from simple stone and bone to advanced alloys and polymers, reflect the changing understanding of both surgical procedures and the human body. This evolution significantly impacted surgical safety and effectiveness, making procedures less invasive and more precise.The development of surgical instruments has been intrinsically linked to the overall progress of civilization.
Early societies relied on rudimentary tools for basic surgical interventions. As knowledge and technology advanced, so did the complexity and sophistication of these tools. This continuous refinement has led to the remarkable surgical instruments and techniques available today.
Progression of Surgical Instruments
Early surgical instruments were primarily made from readily available materials like bone, stone, and wood. These early tools were often crude and lacked the precision necessary for complex procedures. The discovery and utilization of metals like bronze and later iron marked a significant advancement, allowing for stronger and more durable instruments. The introduction of steel further improved the quality and functionality of surgical tools.
This progressive development of materials has allowed for more complex and precise surgical interventions.
Materials Used in Surgical Instrument Construction
The materials used in surgical instruments have evolved alongside the understanding of human anatomy and physiology. Stone, bone, and wood were the primary materials in ancient times, while bronze and iron were significant improvements. The introduction of steel, and later, specialized alloys, allowed for greater strength, sharpness, and durability. Today, advanced materials like titanium, stainless steel, and polymers are used to create instruments with specific properties for various surgical procedures.
These materials are chosen based on factors such as biocompatibility, corrosion resistance, and sterilizability.
Specific Surgical Instruments and their Historical Context
The scalpel, a fundamental surgical instrument, has seen significant evolution. Early scalpel blades were often fashioned from flint or bronze, providing limited precision and control. The development of steel allowed for sharper and more refined blades, leading to greater precision and control. Modern scalpel blades are made from high-carbon steel or other specialized materials, with varying blade shapes and sizes tailored to specific surgical procedures.
Other instruments, such as forceps, retractors, and needles, have also evolved from basic designs to intricate tools designed for greater accuracy and precision.
Evolution of Suturing Instruments
| Period | Instrument | Description | Material |
|---|---|---|---|
| Ancient Egypt (circa 3000 BCE) | Needle | Simple, often made from bone or bronze, used for basic wound closure. | Bone/Bronze |
| Medieval Europe (circa 1000 CE) | Needle | Iron or steel needles became more common, with improved sharpness and durability. | Iron/Steel |
| 19th Century | Surgical needle and suture | Development of various suture materials (catgut, silk). Needles became more precise and adapted for different tissues. | Steel, catgut, silk |
| 20th Century | Needle driver, surgical stapler | Advancements in materials and design led to more precise and efficient suturing. Surgical staplers introduced faster methods for wound closure. | Stainless steel, titanium |
| 21st Century | Microneedles, robotic assisted suturing | Miniaturization and precision tools for microsurgery. Robotic systems enhance precision and dexterity. | Titanium, specialized alloys, polymers |
Impact of Material Advancements on Surgical Safety and Effectiveness
The progression of surgical materials has dramatically improved surgical safety and effectiveness. The development of stainless steel and other biocompatible materials has reduced the risk of infection. The introduction of more durable and precise instruments allows for less invasive procedures, leading to faster recovery times and reduced complications. The rise of specialized alloys and polymers has resulted in instruments that are easier to sterilize and maintain, further enhancing safety.
Materials that resist corrosion and maintain their sharpness for longer periods have led to more efficient procedures.
Concluding Remarks
In conclusion, the history of surgery timeline reveals a remarkable journey of human ingenuity and resilience. From rudimentary techniques in ancient times to the sophisticated procedures of today, surgery has continuously evolved, reflecting societal advancements and scientific progress. The dedication of countless surgeons and the tireless pursuit of knowledge have transformed surgery from a perilous art to a precise and life-saving science.
This journey through time underscores the enduring human desire to heal and the incredible progress that has shaped modern medicine.