What does anger do to your body? This sets the stage for a fascinating exploration of the immediate and long-term effects of anger on our physical well-being. From the initial physiological responses like a racing heart to the potential for long-term health consequences, we’ll delve into the intricate relationship between anger and the human body. Understanding this connection can be crucial for developing healthy coping mechanisms and promoting overall well-being.
This discussion examines the physiological effects of anger, ranging from mild to severe. We’ll look at how anger impacts the cardiovascular system, the nervous system, and various other organ systems. Furthermore, we’ll explore the long-term consequences of chronic anger, including its link to heart disease and other health problems. Finally, practical strategies for managing anger and promoting emotional well-being will be presented, offering valuable tools for personal growth and improved health.
Physiological Effects of Anger
Anger, a common human emotion, triggers a cascade of physiological responses within the body. Understanding these responses is crucial for managing anger effectively and preventing potential health consequences. These reactions, while often automatic, are significant and can impact various bodily systems.The immediate physiological responses to anger are a complex interplay of hormonal and nervous system activity. These responses are not merely a matter of feeling; they manifest as tangible changes in the body, from increased heart rate to heightened muscle tension.
Immediate Physiological Responses
The initial stages of anger involve a rapid activation of the sympathetic nervous system, the body’s “fight-or-flight” response. This system triggers a series of changes designed to prepare the body for physical action. A surge of adrenaline and other stress hormones is released into the bloodstream, increasing heart rate and blood pressure. Simultaneously, blood is diverted away from non-essential organs like the digestive system and towards the muscles, enhancing strength and speed.
This rapid mobilization of resources is vital for responding to perceived threats, but prolonged or frequent episodes of anger can have detrimental effects.
Hormonal Changes During Anger
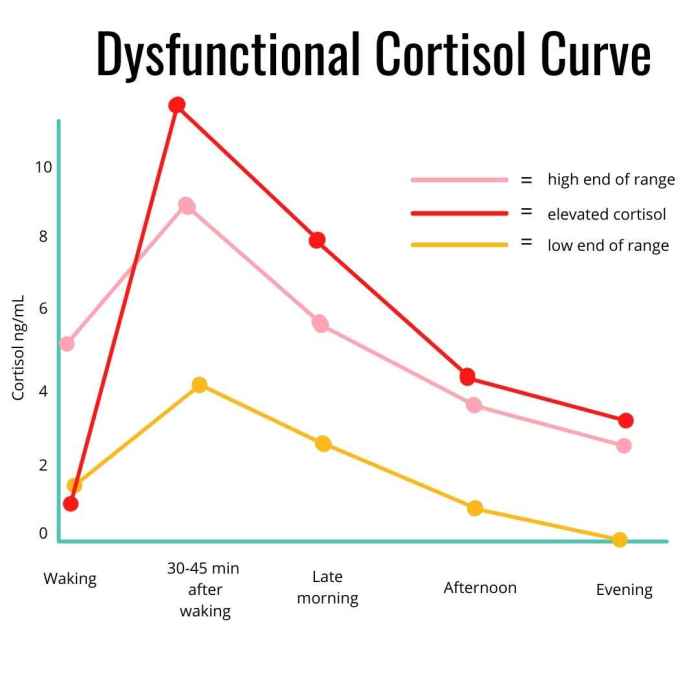
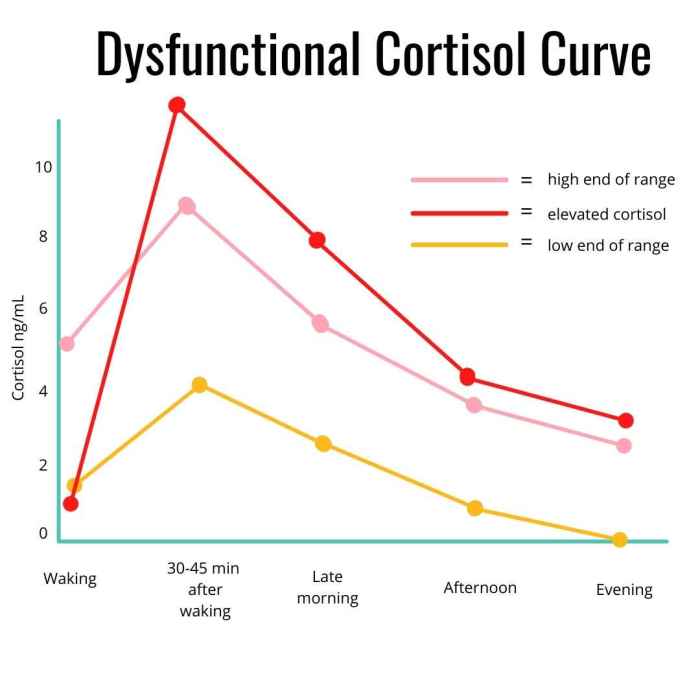
A critical aspect of the physiological response to anger is the release of specific hormones. Adrenaline, also known as epinephrine, plays a central role, increasing heart rate, blood pressure, and breathing rate. Cortisol, another stress hormone, is also released, further contributing to the body’s heightened state of alertness. The release of these hormones is a natural response, but chronic anger can lead to elevated levels, potentially impacting long-term health.
Impact on the Cardiovascular System
Anger significantly affects the cardiovascular system. Increased heart rate and blood pressure are direct consequences of the sympathetic nervous system’s activation. The heightened blood pressure can strain the heart and blood vessels, potentially contributing to cardiovascular problems like hypertension or heart disease. Sustained anger can lead to prolonged periods of elevated blood pressure, increasing the risk of serious cardiovascular complications.
The impact on blood flow is also noteworthy, as blood is diverted from non-essential organs to the muscles, potentially compromising organ function if the anger is prolonged.
Role of the Nervous System
The nervous system is the central orchestrator of the physiological responses to anger. The sympathetic nervous system, part of the autonomic nervous system, is responsible for the immediate “fight-or-flight” response. It stimulates the release of hormones, increases heart rate, and diverts blood flow to muscles. The parasympathetic nervous system, responsible for the “rest-and-digest” response, counteracts the effects of the sympathetic system, promoting relaxation and recovery.
The imbalance in these systems resulting from prolonged anger can disrupt overall bodily function.
Comparison of Physiological Effects Across Anger Levels
| Anger Level | Heart Rate | Blood Pressure | Muscle Tension |
|---|---|---|---|
| Mild | Slightly elevated | Slightly elevated | Minor increase |
| Moderate | Significantly elevated | Substantial increase | Increased tension |
| Severe | Extremely elevated | High | Extreme tension |
The table above illustrates the progressive nature of physiological changes as anger escalates. Mild anger may only produce subtle responses, but severe anger can lead to significant and potentially harmful physiological effects.
Long-Term Consequences of Anger: What Does Anger Do To Your Body
Anger, a natural human emotion, can become detrimental when it’s chronic and uncontrolled. While short-term expressions of anger might be manageable, persistent anger can significantly impact physical and mental well-being over time. Understanding these long-term consequences is crucial for developing healthy coping mechanisms and seeking support when needed.Chronic anger takes a toll on the body and mind, often manifesting in various physical and mental health problems.
This prolonged state of heightened emotional arousal can lead to a cascade of negative effects, impacting various organ systems and increasing the risk of serious illnesses.
Health Implications of Chronic Anger
Uncontrolled anger can have severe consequences on physical health. The physiological responses triggered by anger, such as increased heart rate and blood pressure, when sustained over extended periods, can damage vital organs.
Cardiovascular Risks
Anger and heart disease are intricately linked. Studies have shown a strong correlation between chronic anger and an increased risk of cardiovascular problems. The constant stress response triggered by anger can damage blood vessels, increase blood pressure, and promote the buildup of plaque in arteries. This can lead to heart attacks, strokes, and other cardiovascular complications. For example, individuals with a history of frequent and intense anger outbursts may be more susceptible to developing coronary artery disease.
Other Health Problems, What does anger do to your body
Chronic anger is also linked to various other health issues. The persistent physiological arousal associated with anger can lead to a heightened risk of developing high blood pressure, headaches, and sleep disturbances. These conditions can further exacerbate the negative effects of anger, creating a vicious cycle. High blood pressure, for instance, is a known risk factor for heart disease, and the stress associated with anger can further elevate blood pressure readings.
Mental Health Issues
Beyond physical health, uncontrolled anger can significantly impact mental well-being. Chronic anger can contribute to anxiety, depression, and other mood disorders. The constant negativity and frustration associated with anger can lead to feelings of isolation and hopelessness. Moreover, anger management issues can strain relationships and create difficulties in navigating social situations.
Impact on Organ Systems
The sustained physiological response to anger can affect multiple organ systems over time. A structured view of this impact can be seen in the following table:
| Organ System | Potential Impacts |
|---|---|
| Cardiovascular | Increased risk of heart disease, high blood pressure, abnormal heart rhythms |
| Endocrine | Hormonal imbalances, increased cortisol levels, impacting metabolism and stress response |
| Gastrointestinal | Increased risk of digestive problems, ulcers, and irritable bowel syndrome |
| Immune | Weakened immune system, increased susceptibility to infections |
| Nervous | Chronic headaches, sleep disturbances, anxiety, and depression |
Prolonged anger can damage multiple organ systems, making it crucial to address anger management strategies and seek professional help if needed.
Management and Coping Mechanisms
Anger, while a natural human emotion, can become detrimental if not managed effectively. Understanding how to channel anger into constructive outlets and employ healthy coping mechanisms is crucial for maintaining mental and physical well-being. Learning these strategies empowers individuals to navigate challenging situations and prevent anger from escalating into harmful behaviors.
Ever wondered what happens inside you when you’re furious? Anger can wreak havoc on your body, triggering a cascade of physical responses. Understanding how anger affects your physical health is crucial, especially when considering the spread of contagious illnesses like the flu. For example, knowing the facts about how the flu spreads, such as through respiratory droplets and contact with contaminated surfaces, is vital for prevention, as outlined in this helpful article on is the flu airborne facts transmission prevention.
Ultimately, managing your anger effectively can significantly improve your overall well-being and reduce your vulnerability to illnesses like the flu.
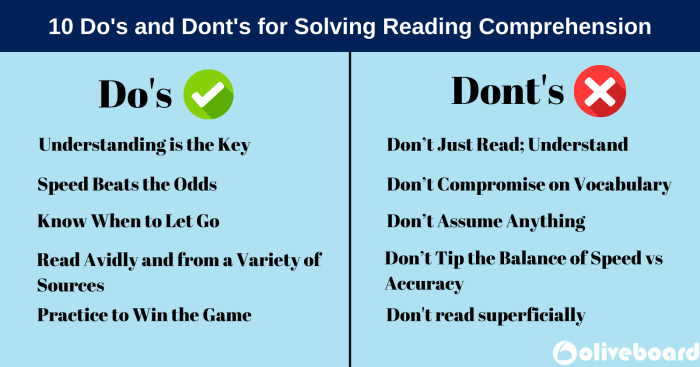
Strategies for Managing Anger Healthily
Effective anger management involves a multi-faceted approach. This includes identifying triggers, recognizing early warning signs of escalating anger, and developing proactive strategies to de-escalate before it becomes overwhelming. These strategies are not a quick fix, but rather a consistent effort to retrain responses and build healthier emotional regulation skills. The key is to practice these techniques regularly to build resilience and improve overall well-being.
Relaxation Techniques for Anger Regulation
Relaxation techniques are powerful tools for calming the body and mind when anger arises. They help lower physiological arousal associated with anger, creating space for rational thought and reducing the intensity of emotional responses. These techniques work by engaging the parasympathetic nervous system, which promotes relaxation and reduces stress hormones.
- Deep Breathing Exercises (High): Deep breathing techniques are highly effective for calming the nervous system. Slow, deep breaths regulate the body’s response to stress, reducing heart rate and blood pressure, which are physiological indicators of anger. These exercises can be practiced anywhere, anytime, making them highly accessible and readily available methods for anger management.
- Progressive Muscle Relaxation (Medium): This technique involves systematically tensing and releasing different muscle groups in the body. By focusing on physical sensations, individuals can become more aware of tension and learn to release it. Regular practice can help reduce physical symptoms of anger and promote relaxation. The effectiveness is somewhat dependent on the individual’s ability to focus on physical sensations.
- Mindfulness Meditation (High): Mindfulness meditation cultivates present-moment awareness, allowing individuals to observe their thoughts and feelings without judgment. By recognizing anger as a transient emotion, mindfulness reduces its power and promotes emotional regulation. Consistent practice can significantly enhance self-awareness and emotional intelligence, leading to better anger management.
Constructive Methods for Expressing Anger
Expressing anger constructively is crucial for maintaining healthy relationships and preventing the buildup of resentment. Instead of suppressing or exploding, individuals can use assertive communication to address concerns and needs directly. This involves clearly articulating feelings and needs without resorting to aggression or blame.
- Assertive Communication: This involves expressing feelings and needs directly and respectfully, without resorting to aggression or blame. Assertive communication is a valuable skill that promotes healthy conflict resolution and fosters understanding. It helps ensure that needs are addressed while maintaining respectful interactions.
- Journaling: Writing down feelings and thoughts related to anger can provide a safe space for processing emotions. This can help identify patterns and triggers, allowing for a deeper understanding of anger’s root causes.
- Physical Activity: Engaging in physical activity, such as exercise or sports, can be a healthy outlet for pent-up anger. Physical exertion releases endorphins, which have mood-boosting effects and can help shift focus away from negative emotions.
Therapeutic Approaches for Anger Management
Various forms of therapy can help individuals manage anger effectively. These therapies focus on identifying the root causes of anger, developing coping mechanisms, and changing negative thought patterns. These therapies also focus on teaching healthy emotional regulation skills and address any underlying mental health conditions that may contribute to anger.
- Cognitive Behavioral Therapy (CBT): CBT is a highly effective therapy for anger management. CBT helps individuals identify and challenge negative thought patterns that contribute to anger. By changing these patterns, individuals can develop healthier responses to triggering situations.
- Dialectical Behavior Therapy (DBT): DBT focuses on emotional regulation, interpersonal effectiveness, and distress tolerance. It helps individuals develop skills to manage intense emotions, including anger, and improve relationships. This can help individuals identify and address the underlying causes of anger.
Coping Mechanism Effectiveness
| Coping Mechanism | Effectiveness Level | Description |
|---|---|---|
| Deep Breathing Exercises | High | Regulates the nervous system, reduces physiological arousal. |
| Progressive Muscle Relaxation | Medium | Reduces physical tension associated with anger. |
| Mindfulness Meditation | High | Promotes present moment awareness, reducing judgment of emotions. |
| Cognitive Behavioral Therapy | High | Challenges negative thought patterns, promotes healthier responses. |
| Physical Activity | Medium | Releases endorphins, shifts focus away from negative emotions. |
Impact on Specific Body Systems
Anger, a powerful emotion, isn’t just a feeling; it has a tangible impact on our physical well-being. Understanding how anger affects different body systems is crucial for developing healthy coping mechanisms and managing this often-overlooked aspect of our health. It’s important to recognize that these effects are interconnected and often exacerbate each other, highlighting the importance of a holistic approach to anger management.The physiological responses triggered by anger can have a ripple effect throughout the body, influencing various systems and potentially leading to long-term health consequences.
Chronic anger can contribute to various health problems, making understanding its impact on specific systems critical for preventative care.
Digestive System Effects
Anger significantly impacts the digestive system. The stress response triggered by anger can disrupt normal digestive processes, leading to a variety of issues. This includes reduced blood flow to the digestive tract, which can hinder nutrient absorption and lead to feelings of nausea, indigestion, or abdominal pain. Furthermore, the release of stress hormones during anger can cause increased muscle tension in the digestive system, contributing to cramping and discomfort.
The body’s resources are redirected away from the digestive system, leading to compromised function during periods of high stress and anger.
Immune System Impact
Anger’s impact on the immune system is substantial. Chronic anger and the accompanying stress response can suppress the immune system’s ability to fight off infections. This can make individuals more susceptible to illnesses and slow down the healing process. Studies have shown a correlation between prolonged stress and suppressed immune function, leading to an increased risk of catching common colds, flu, and other viral infections.
Sleep Pattern Disturbances
Anger can significantly disrupt sleep patterns. The heightened physiological arousal associated with anger can interfere with the body’s natural sleep-wake cycle. Elevated heart rate, muscle tension, and racing thoughts can make it difficult to fall asleep or stay asleep. The resulting sleep deprivation can further exacerbate anger and stress, creating a vicious cycle. Individuals experiencing chronic anger often report difficulties with both the quantity and quality of sleep, leading to fatigue and reduced cognitive function.
Role in Triggering Headaches
Anger is often a significant trigger for headaches. The tension and constriction in blood vessels caused by the stress response associated with anger can lead to tension headaches. The release of stress hormones, such as adrenaline and cortisol, can further constrict blood vessels, increasing pain and pressure in the head. The cycle of anger, stress, and headache can become quite persistent, making it crucial to address the underlying anger issues to manage headaches effectively.
Impact on Skin Conditions
Anger can affect skin conditions by increasing the production of stress hormones, which can contribute to inflammation and exacerbate existing skin conditions. The inflammatory response associated with anger can lead to flare-ups of conditions like acne, eczema, and psoriasis. Furthermore, the stress associated with anger can negatively impact the body’s ability to repair skin damage, making it more susceptible to irritation and dryness.
This highlights the link between mental health and skin health, demonstrating how emotional well-being plays a critical role in overall physical health.
Illustrative Examples
Anger, a powerful emotion, manifests in diverse ways across individuals and cultures. Understanding these expressions is crucial for recognizing and managing anger effectively. This section provides examples of how anger manifests, the scenarios that trigger it, and the impact of cultural perspectives on its expression.Different individuals react to anger differently, often based on personal experiences, learned behaviors, and their emotional makeup.
Some may exhibit outward aggression, while others might internalize their feelings, leading to simmering resentment or passive-aggressive behaviors. These variations highlight the complexity of anger management and the need for tailored strategies.
Anger Manifestations in Different Individuals
Various factors contribute to how individuals express anger. Personality traits, past experiences, and learned coping mechanisms significantly influence the outward display of anger. Some individuals might yell, throw things, or engage in physical altercations, while others might withdraw, become silent, or exhibit sullen behavior. These differences underscore the need for individualized approaches to anger management.
Anger can wreak havoc on your physical well-being, triggering a cascade of stress hormones that impact everything from your heart rate to your digestion. It’s a powerful emotion, and often, people turn to unhealthy coping mechanisms like those explored in Rachel Charlton Dailey’s powerful story, ” rachel charlton dailey my journey with alcoholism “. Understanding how anger affects our bodies is key to finding healthier ways to manage it and move forward, whether that’s through therapy, exercise, or other coping strategies.
Anger-Eliciting Scenarios
Anger is frequently triggered by perceived injustices, threats to personal well-being, or unmet expectations. These situations can vary widely, from minor inconveniences like traffic jams to major life events like job loss or relationship conflicts. The intensity of the anger response is often proportional to the perceived threat or significance of the event.
Cultural Perspectives on Anger Expression
Cultural norms play a significant role in how individuals are expected to express anger. Some cultures prioritize direct confrontation and verbal outbursts, while others value emotional restraint and indirect communication. These differing expectations shape the expression and management of anger within a society.
Impact of Anger in Different Age Groups
The manifestation and management of anger vary across different age groups. Children may express anger through tantrums or defiance, while adolescents might exhibit irritability or withdrawal. Adults typically employ more nuanced methods of expressing and managing anger, though individual differences persist.
Anger can wreak havoc on your body, causing everything from a racing heart to muscle tension. Understanding the physical symptoms is crucial, but sometimes, those symptoms can mimic other conditions. A crucial step in properly diagnosing the source of your discomfort is a differential diagnosis confirming your diagnosis, which helps rule out other potential issues. This process is essential in identifying the root cause, ensuring you’re receiving the correct treatment for your specific needs.
Ultimately, understanding how anger affects your body, through thorough examination and differential diagnosis, is key to managing its impact on your well-being. differential diagnosis confirming your diagnosis
Table Summarizing Anger Expressions Across Cultures
Culture Typical Anger Expression Social Norms Western Verbal outbursts, aggressive body language, direct confrontation Direct confrontation often accepted as a means of resolving conflict. Eastern Indirect communication, avoidance, emotional restraint Emotional restraint and maintaining harmony valued above direct confrontation. Latin American Strong emotional displays, physical expressions of frustration, and open expression of emotions. Open expression of emotions is common and often seen as a natural response to situations. Indigenous Cultures (e.g., Native American) Vary widely depending on specific tribe/nation; often emphasize respect, mediation, and indirect communication Cultural practices often emphasize spiritual and communal well-being, influencing anger expression.
Understanding the diverse expressions of anger across cultures is vital for fostering empathy and effective communication. Cultural sensitivity plays a critical role in managing interpersonal conflicts.
Brain Chemistry and Anger
Anger, a powerful human emotion, is more than just a feeling; it’s a complex physiological response involving intricate interactions within the brain. Understanding the neurochemicals and brain regions involved in anger processing is crucial for developing effective anger management strategies. This intricate interplay dictates how we experience and react to anger, influencing both immediate and long-term consequences.
Neurochemicals Involved in Anger Responses
The experience of anger is intricately linked to a cascade of neurochemicals. These chemical messengers influence our emotional state and behavioral responses. Key neurochemicals associated with anger include norepinephrine, dopamine, and serotonin. Norepinephrine, often called the “fight-or-flight” hormone, increases heart rate and alertness, preparing the body for action. Dopamine, associated with reward and motivation, can intensify feelings of anger, particularly when coupled with perceived injustice or frustration.
Serotonin, a mood-regulating neurotransmitter, can play a role in modulating anger; imbalances in serotonin levels can contribute to heightened irritability and emotional dysregulation.
The Role of the Amygdala in Processing Anger
The amygdala, a small almond-shaped structure deep within the brain, acts as a crucial hub for processing emotions, including anger. It rapidly assesses situations for potential threat and triggers a cascade of physiological responses. The amygdala’s rapid response system is often referred to as the “emotional brain,” and its immediate evaluation of a situation can lead to an angry reaction before the prefrontal cortex (the “thinking brain”) has a chance to intervene.
This rapid assessment mechanism can sometimes result in impulsive reactions and hinder rational problem-solving.
Impact of Stress Hormones on Anger Reactions
Stress hormones, such as cortisol and adrenaline, significantly influence anger reactions. These hormones prepare the body for immediate action, increasing heart rate, blood pressure, and alertness. Chronic stress can lead to elevated cortisol levels, potentially making individuals more susceptible to experiencing anger more frequently and intensely. In individuals already predisposed to anger issues, chronic stress can further exacerbate existing tendencies.
Brain Activity Changes During Anger
Brain activity undergoes measurable changes during episodes of anger. Areas associated with emotional processing, like the amygdala, show increased activity, while areas responsible for rational thought and control, such as the prefrontal cortex, demonstrate decreased activity. This imbalance can explain the impulsive and less-controlled nature of anger responses. For example, a study found that individuals experiencing anger showed heightened activity in the amygdala and reduced activity in the prefrontal cortex.
How Different Brain Regions Interact to Produce an Anger Response
An anger response isn’t solely generated by one brain region. Several regions interact in a complex interplay to produce the full response. The amygdala, as previously discussed, rapidly assesses potential threats, while the prefrontal cortex attempts to regulate the emotional response. The hippocampus plays a role in memory and context, influencing how the amygdala perceives a situation. The hypothalamus, responsible for autonomic functions, triggers the physiological changes associated with anger.
These regions work together, with the prefrontal cortex’s role in regulating the response being crucial for modulating the intensity and duration of the angry reaction. This intricate interplay highlights the complexity of the anger response and the need for comprehensive strategies to manage it effectively.
Closing Notes
In conclusion, anger’s impact on the body is multifaceted and profound. Understanding the physiological responses, long-term effects, and available coping mechanisms is essential for navigating anger effectively. By recognizing the ways anger affects our physical and mental health, we can develop healthier responses and strategies for managing our emotions. This knowledge empowers us to prioritize our well-being and live more fulfilling lives.