The cortisol weight loss controversy rages on. Is cortisol truly the villain in our weight struggles, or is there more to the story? This deep dive explores the complex relationship between cortisol, stress, and weight management, examining the science behind the claims and dissecting the differing perspectives on this often-misunderstood hormone.
From the physiological mechanisms of cortisol action to the impact of stress on our bodies, we’ll unravel the complexities of this hormone’s influence on our weight. We’ll also examine the role of lifestyle factors, current research, and practical implications for those seeking to understand and manage their weight effectively.
Defining the Controversy
The cortisol weight loss controversy centers on the complex relationship between the stress hormone cortisol and body weight. While cortisol is crucial for various bodily functions, its role in regulating metabolism and fat storage is debated. Proponents of a strong link between cortisol and weight gain argue that chronic stress elevates cortisol levels, leading to detrimental effects on weight management.
Conversely, some argue that cortisol’s influence on weight is overstated and that other factors play a more significant role. This debate involves a wide range of perspectives, from those who view cortisol as a primary driver of weight gain to those who see it as a secondary factor influenced by a multitude of other variables.This discussion is important because understanding the true impact of cortisol on weight management can inform effective strategies for weight loss and weight maintenance.
Misinterpretations can lead to ineffective or potentially harmful interventions. Addressing the conflicting perspectives and evidence is crucial to forming a balanced understanding of this complex interaction.
Core Arguments and Perspectives
The controversy surrounding cortisol’s role in weight management revolves around several key arguments and differing perspectives. Different schools of thought exist on how cortisol affects weight regulation. A nuanced understanding requires examining these varying viewpoints.
| Perspective | Argument | Evidence/Supporting Points |
|---|---|---|
| Elevated Cortisol = Weight Gain | Chronic stress and elevated cortisol levels disrupt metabolic processes, leading to increased fat storage, particularly in the abdominal region. This is often linked to decreased insulin sensitivity and altered energy expenditure. | Studies have shown correlations between high cortisol levels and abdominal obesity in some individuals. Animal models have demonstrated cortisol’s impact on fat deposition. Clinical observations in individuals experiencing chronic stress often show weight gain. |
| Cortisol’s Influence is Secondary | While cortisol plays a role in the body’s response to stress, its effect on weight is largely mediated by other factors such as diet, exercise, and sleep. Other hormones, such as insulin and growth hormone, have a more significant impact on weight regulation. | Studies demonstrating that other lifestyle factors, such as diet and exercise, have a more significant impact on weight management. Some studies highlight that individuals with high cortisol levels but healthy lifestyles do not exhibit the same degree of weight gain. The complex interplay of various hormonal systems and metabolic pathways makes attributing weight gain solely to cortisol challenging. |
| Cortisol’s Role is Contextual | Cortisol’s impact on weight is not uniform and depends on various factors like individual metabolic profiles, genetics, and the intensity and duration of stress. | Studies have shown that the relationship between cortisol and weight gain is not consistent across all individuals. Variations in genetic predispositions, metabolic rates, and lifestyle choices can modify the impact of cortisol on weight. |
Historical Context of the Discussion
The discussion on cortisol and weight loss has evolved over time, influenced by advancements in scientific research and changing societal views on stress and well-being. Early studies focused primarily on the physiological effects of cortisol, laying the groundwork for understanding its role in metabolism and stress responses. More recent research has emphasized the complex interplay of various factors in weight regulation, recognizing the limitations of attributing weight gain solely to cortisol levels.
This evolution has led to a more nuanced understanding of cortisol’s influence.
The cortisol weight loss controversy is fascinating, but it’s important to remember that the body’s stress response is complex. While some claim cortisol can lead to weight gain, understanding the prognosis for conditions like metastatic prostate cancer ( metastatic prostate cancer prognosis ) reveals how critical hormone balance is in overall health. Ultimately, a holistic approach, considering factors beyond cortisol alone, is key to understanding weight management.
Mechanisms of Cortisol Action
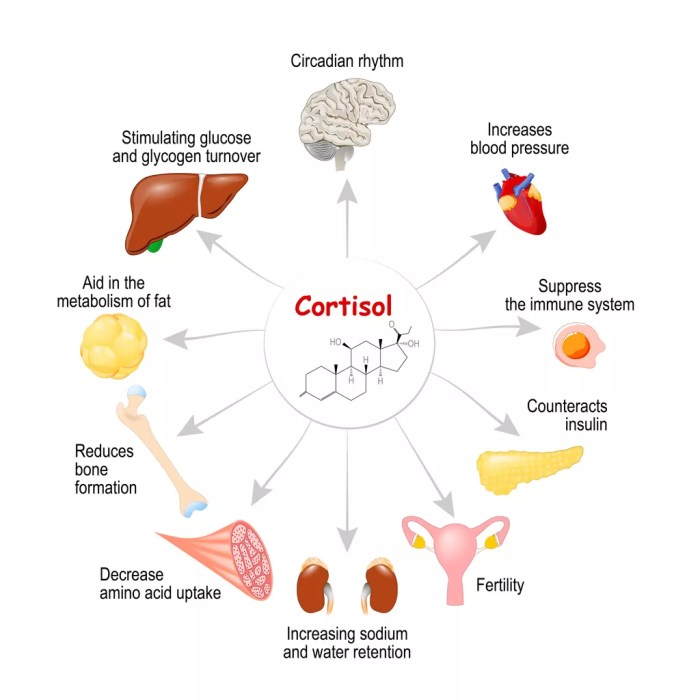
Cortisol, a crucial hormone produced by the adrenal glands, plays a multifaceted role in the body’s physiological processes. While often associated with stress responses, cortisol’s impact extends far beyond that, influencing metabolism, immune function, and, importantly, weight management. Understanding the intricate mechanisms by which cortisol affects weight is essential to addressing the controversy surrounding its role in weight gain.Cortisol’s influence on weight is not a simple case of “good” or “bad”.
Its effects are complex and often depend on factors like the duration and intensity of stress, individual genetic predispositions, and overall health. This intricate interplay leads to diverse outcomes, which we will explore in more detail.
Cortisol and Metabolism
Cortisol’s effects on metabolism are profound. It enhances the breakdown of proteins into amino acids, a process crucial for energy production. This increased protein breakdown can have implications for muscle mass, which, in turn, can impact basal metabolic rate (BMR). Furthermore, cortisol stimulates gluconeogenesis, the production of glucose from non-carbohydrate sources. This process is essential for maintaining blood sugar levels but can also contribute to elevated blood glucose, potentially leading to insulin resistance, which is often linked to weight gain.
Cortisol and Fat Storage
Cortisol’s influence on fat storage is particularly complex. While it can promote the breakdown of fat in certain tissues, it also promotes the storage of fat in the abdominal region. This is often referred to as visceral fat, which is associated with a higher risk of health problems. The exact mechanisms behind this preferential storage are not fully understood, but it’s believed to be connected to its impact on insulin sensitivity and the regulation of adipogenesis (fat cell formation).
A chronic stress response, which leads to higher cortisol levels, can thus contribute to visceral fat accumulation.
Cortisol and Appetite Regulation
Cortisol’s role in appetite regulation is a critical aspect of its influence on weight. Studies suggest that cortisol can stimulate appetite, particularly for high-calorie, high-carbohydrate foods. This effect is likely mediated through the hypothalamic-pituitary-adrenal (HPA) axis, a key regulatory system in the body. Elevated cortisol levels can lead to cravings for comfort foods, which often contain high amounts of sugars and fats, further exacerbating weight gain.
Cortisol Effects on Men and Women
The effects of cortisol on men and women differ slightly, primarily due to hormonal variations. Women tend to have a higher baseline cortisol level than men. This difference might contribute to the potential higher susceptibility to weight gain in some women. Furthermore, the distribution of fat storage under the influence of cortisol may differ between sexes.
Cortisol-Mediated Weight Changes: A Flowchart
The following flowchart illustrates the steps involved in cortisol’s influence on weight, highlighting the complex interplay of various physiological pathways.

Note: This is a simplified representation of a complex process. Numerous other factors and interactions influence the outcome.
Cortisol and Stress
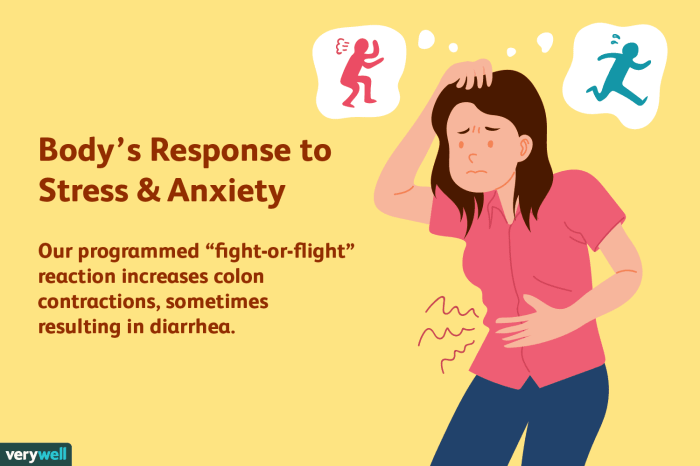
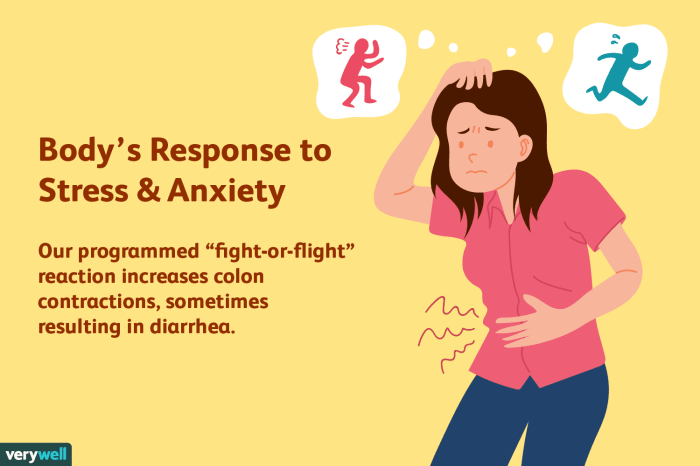
Stress is a ubiquitous part of modern life, and its impact on our bodies, including our hormone levels and weight, is undeniable. Cortisol, the primary stress hormone, plays a crucial role in regulating various bodily functions, but chronic or excessive stress can disrupt its balance, leading to a cascade of effects, including weight gain. Understanding this connection is key to effective stress management and healthy weight management strategies.Cortisol, a steroid hormone produced by the adrenal glands, is vital for maintaining homeostasis.
In response to stress, cortisol is released to provide the body with the energy needed to cope with the perceived threat. However, sustained exposure to stressors leads to chronically elevated cortisol levels, which can disrupt metabolic processes and contribute to weight gain. This disruption of normal physiological functions is a major contributor to the difficulties people face in managing their weight.
The Connection Between Stress, Cortisol, and Weight Gain
The relationship between stress, cortisol, and weight gain is complex and multifaceted. Elevated cortisol levels can lead to increased appetite, particularly for high-calorie, sugary foods, and decreased metabolic rate. This combination can lead to a surplus of calories, which are then stored as fat, contributing to weight gain. Furthermore, chronic stress can disrupt sleep patterns, another crucial factor in weight management, as insufficient sleep is associated with increased cortisol levels and altered metabolism, further hindering weight loss efforts.
The Role of Chronic Stress in Cortisol Dysregulation
Chronic stress, unlike acute stress, is a prolonged exposure to stressors. This persistent elevation of cortisol levels can lead to significant physiological changes. The body’s natural feedback mechanisms that regulate cortisol production become overwhelmed, leading to dysregulation. This dysregulation can have far-reaching effects, impacting not only weight management but also overall health and well-being. Long-term cortisol exposure can weaken the immune system, increasing susceptibility to illness and potentially impacting the body’s ability to process and utilize nutrients efficiently, further contributing to weight gain.
The impact of chronic stress can be profound, as seen in studies that demonstrate a correlation between chronic stress and increased abdominal fat deposition.
Different Types of Stress and Their Impact on Cortisol Levels and Weight Outcomes
Different types of stress elicit varying responses in the body. While acute stress, like a sudden confrontation, can trigger a temporary cortisol spike, chronic stress, stemming from prolonged exposure to demanding situations, can lead to sustained elevated cortisol levels. This sustained elevation can negatively impact metabolic processes, ultimately affecting weight management.
| Stress Type | Effect on Cortisol | Effect on Weight |
|---|---|---|
| Acute Stress (e.g., a sudden argument) | Temporary spike in cortisol levels | Potentially minimal or no significant effect on weight, depending on the individual’s response. |
| Chronic Stress (e.g., demanding job, relationship problems) | Sustained elevated cortisol levels | Increased appetite, decreased metabolic rate, potential for abdominal fat accumulation, and difficulty in weight management. |
| Psychological Stress (e.g., anxiety, depression) | Increased cortisol levels, often chronic in nature | Increased appetite for comfort foods, disrupted sleep, potentially impacting metabolic function and leading to weight gain. |
| Financial Stress | Elevated cortisol levels | Increased consumption of inexpensive, high-calorie foods, and reduced access to healthy options, potentially leading to weight gain. |
| Social Stress (e.g., bullying, social isolation) | Increased cortisol levels, potentially chronic | Increased cravings, potentially impacting sleep, impacting metabolic function, and contributing to weight gain. |
Factors Influencing Cortisol Levels
Understanding cortisol levels is crucial for comprehending its impact on weight management. Cortisol, the body’s primary stress hormone, is a complex player in various bodily functions, and its production is not static. A multitude of factors can influence its levels, ranging from genetic predispositions to everyday lifestyle choices. This section delves into these influential factors, highlighting the intricate interplay between genetics, diet, lifestyle, and cortisol regulation.
Genetic Predisposition
Individual genetic makeup plays a significant role in determining an individual’s cortisol response. Variations in genes responsible for cortisol synthesis, metabolism, and receptor sensitivity can affect how the body produces and utilizes cortisol. Some individuals might naturally have a higher baseline cortisol level or a greater tendency to experience heightened cortisol responses to stress compared to others. This inherent predisposition can impact the effectiveness of certain weight management strategies.
The cortisol weight loss controversy is fascinating, but often misunderstood. While some claim cortisol can directly lead to weight gain, the truth is much more nuanced. Sometimes, changes in your hormone levels, like those related to missing your period, can play a significant role in the cortisol response and subsequent weight fluctuations. If you’re curious about the various reasons why your period might be delayed, check out this helpful guide on reasons you missed your period.
Ultimately, the cortisol weight loss debate is complex and requires a holistic understanding of your overall health and lifestyle.
Dietary Influences
Diet significantly affects cortisol levels. A diet rich in processed foods, sugar, and unhealthy fats can contribute to increased cortisol production, while a balanced diet emphasizing whole foods, lean proteins, and complex carbohydrates can help maintain healthier cortisol levels. Nutrient deficiencies can also impact cortisol production, as certain vitamins and minerals are crucial for optimal cortisol metabolism.
Lifestyle Choices and Cortisol
Lifestyle choices exert a powerful influence on cortisol levels. Consistent stress, lack of sleep, and inadequate exercise can disrupt the body’s natural cortisol rhythm, leading to elevated levels. Conversely, a balanced lifestyle incorporating sufficient sleep, regular exercise, and stress management techniques can contribute to more stable cortisol levels. Chronic stress, a pervasive aspect of modern life, has a direct correlation with elevated cortisol levels, potentially impacting weight management goals.
Sleep and Cortisol Regulation
Adequate sleep is essential for regulating cortisol levels. During sleep, the body repairs and rejuvenates, and cortisol levels naturally decrease. Chronic sleep deprivation can disrupt this natural rhythm, leading to higher cortisol levels throughout the day. Maintaining a regular sleep schedule and ensuring sufficient sleep duration can contribute to healthier cortisol regulation and overall well-being.
Exercise and Cortisol Dynamics
Regular exercise can help regulate cortisol levels, but the relationship is nuanced. While intense or prolonged exercise can temporarily elevate cortisol, moderate-intensity exercise, like brisk walking or cycling, often results in a subsequent decrease in cortisol levels. This beneficial effect can contribute to better weight management by reducing stress and improving metabolic function.
Impact of Stress on Cortisol
Stress, whether acute or chronic, profoundly impacts cortisol levels. Acute stress triggers a temporary increase in cortisol, but chronic stress can lead to sustained elevated cortisol levels. Managing stress through techniques like mindfulness, meditation, and relaxation exercises can help regulate cortisol production.
Table: Lifestyle Factors and Cortisol Levels
| Lifestyle Factor | Impact on Cortisol | Potential Effect on Weight |
|---|---|---|
| Balanced Diet | Maintains stable levels | Supports healthy weight management |
| Chronic Stress | Elevated levels | Increased risk of weight gain |
| Regular Exercise (moderate) | Decreased levels | Supports weight loss and maintenance |
| Adequate Sleep | Natural fluctuations | Contributes to healthy weight management |
| Inadequate Sleep | Elevated levels | Increased risk of weight gain |
| Genetic Predisposition | Varying baseline levels | Potential impact on weight management |
Current Research and Studies
The relationship between cortisol and weight loss remains a complex and debated topic. While a clear causal link between chronic stress-induced cortisol elevation and weight gain is often implied, the scientific evidence is not always straightforward. Understanding the nuances of cortisol’s impact on metabolism and body composition requires careful examination of the current research landscape.
Animal Studies on Cortisol and Weight Gain
Animal studies have played a significant role in exploring the mechanisms behind cortisol’s influence on weight. These studies often involve controlled environments and specific manipulations of cortisol levels, allowing researchers to isolate the effects of cortisol. However, extrapolating findings directly to humans requires caution due to differences in physiology and lifestyle factors.
The cortisol weight loss controversy is definitely a confusing one, isn’t it? While some swear by reducing cortisol levels to shed pounds, the science is still murky. A handful of walnuts every day for health, packed with healthy fats and antioxidants, might actually help in managing stress hormones, and therefore potentially influence weight loss efforts. Check out this article for more on the benefits of incorporating walnuts into your daily routine: handful of walnuts every day for health.
Ultimately, a balanced diet and lifestyle, including stress management techniques, might be more effective than focusing solely on cortisol reduction for weight loss.
- Chronic stress exposure in animal models, typically induced through various methods, frequently leads to increased abdominal fat deposition. This suggests a correlation between elevated cortisol and adiposity. For example, studies on rats subjected to chronic restraint stress have shown significant increases in body weight and fat mass, correlating with elevated circulating cortisol levels.
- Certain animal studies demonstrate that cortisol can alter metabolic pathways, impacting glucose metabolism and insulin sensitivity. These changes can, in turn, contribute to fat storage. For instance, experiments involving genetically modified mice with altered cortisol responses have highlighted the crucial role of cortisol in regulating fat accumulation in specific tissues.
Human Trials Investigating Cortisol and Weight Loss, The cortisol weight loss controversy
Human trials, while more complex than animal studies, offer valuable insights into the impact of cortisol on weight in real-world settings. These studies face challenges related to controlling various lifestyle factors and individual differences in cortisol response.
- Studies examining the correlation between perceived stress levels and body weight in humans have often yielded mixed results. While some studies suggest a positive association between chronic stress and weight gain, others find no significant correlation. This discrepancy highlights the multifaceted nature of the relationship between stress, cortisol, and weight.
- Research investigating the impact of specific interventions aimed at reducing cortisol levels, such as mindfulness-based stress reduction programs, on weight loss has produced inconsistent findings. The efficacy of such interventions in promoting weight loss seems to vary significantly between individuals, potentially due to the complex interplay of psychological and physiological factors.
Limitations of Current Research
Current research on cortisol and weight loss faces several limitations. These limitations affect the interpretation and generalizability of the findings.
- The complexity of human physiology and lifestyle factors is a significant hurdle. Individual responses to stress and cortisol vary widely, making it difficult to establish a universal correlation between cortisol levels and weight gain.
- Measurement challenges associated with assessing cortisol levels accurately over time contribute to inconsistencies in the findings. The variability in cortisol secretion patterns, influenced by factors like time of day and stress exposure, makes it difficult to obtain a representative measure.
Conclusion:
The existing research on cortisol and weight loss suggests a complex interplay between stress, cortisol levels, and weight gain. While some animal and human studies show a correlation, the results are not conclusive and often inconsistent. Further research is needed to elucidate the specific mechanisms and identify the individual factors that influence this relationship.
Practical Implications and Recommendations: The Cortisol Weight Loss Controversy
Understanding the complex relationship between cortisol, stress, and weight loss is crucial for developing effective strategies. While cortisol isn’t inherently “bad,” chronic stress and elevated cortisol levels can significantly impact weight management, often leading to unwanted fat storage, particularly around the abdominal area. This section provides practical advice and actionable steps for individuals concerned about cortisol’s influence on their weight.This section delves into practical implications, offering actionable strategies for managing stress, regulating cortisol levels, and making lifestyle modifications for better weight management.
The key lies in finding a balance that supports overall well-being and reduces the negative impact of cortisol on weight.
Stress Management Techniques
Chronic stress triggers a sustained release of cortisol, which can lead to increased appetite and fat storage. Effective stress management is therefore a cornerstone of weight management when cortisol is a concern. Various techniques can help regulate cortisol levels and reduce the impact of stress on the body.
- Mindfulness and Meditation: Practicing mindfulness and meditation can help calm the mind and reduce the body’s stress response. Regular practice can lower cortisol levels and promote a sense of well-being. Studies have shown a correlation between mindfulness practices and decreased cortisol levels.
- Physical Activity: Exercise is a powerful stress reliever. Regular physical activity, whether it’s a brisk walk, a yoga class, or a gym workout, helps the body release endorphins, which have mood-boosting effects and help reduce cortisol levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Sleep Hygiene: Adequate sleep is essential for hormone regulation, including cortisol. Establish a consistent sleep schedule, create a relaxing bedtime routine, and ensure a conducive sleep environment. Aim for 7-9 hours of quality sleep per night.
- Time Management: Effective time management helps reduce feelings of overwhelm and stress. Prioritize tasks, break down large projects into smaller steps, and learn to say “no” to commitments that exceed your capacity.
Dietary Strategies
Diet plays a significant role in regulating cortisol levels and supporting weight management. A balanced diet that includes adequate protein, healthy fats, and complex carbohydrates can help maintain stable blood sugar levels, reducing fluctuations in cortisol.
- Prioritize Protein: Protein is crucial for satiety and muscle maintenance. Incorporating lean protein sources like chicken, fish, beans, and lentils into your diet can help you feel fuller for longer and support healthy metabolism.
- Healthy Fats: Include healthy fats like avocados, nuts, and seeds in your diet. These fats support hormone production and can help regulate cortisol levels.
- Complex Carbohydrates: Choose complex carbohydrates like whole grains, fruits, and vegetables over simple sugars. Complex carbohydrates release energy more slowly, helping to stabilize blood sugar and reduce cortisol spikes.
- Limit Processed Foods and Sugars: Processed foods and sugary drinks can lead to blood sugar imbalances and contribute to cortisol fluctuations. Reducing intake of these foods can help regulate cortisol levels and improve overall health.
Lifestyle Modifications
Certain lifestyle choices can significantly impact cortisol levels and weight management.
- Hydration: Staying adequately hydrated is essential for overall health and can positively influence cortisol levels. Drink plenty of water throughout the day.
- Sunlight Exposure: Sunlight exposure helps regulate the body’s natural circadian rhythm and can positively influence cortisol levels. Aim for regular outdoor time, even during the winter months.
- Social Connection: Strong social connections and supportive relationships can buffer against stress and contribute to overall well-being. Prioritize meaningful interactions with loved ones.
Resources for Further Exploration
- National Institute of Mental Health (NIMH)
- Mayo Clinic
- Harvard Health Publishing
- American Psychological Association (APA)
Illustrative Examples
Understanding how cortisol dysregulation affects weight gain requires looking at real-world scenarios. These examples highlight the complex interplay between stress, cortisol levels, and dietary choices. They demonstrate how addressing cortisol imbalances can significantly improve weight management strategies.Cortisol, while crucial for various bodily functions, can become a detrimental factor when chronically elevated. This often leads to a cascade of negative consequences, including increased appetite, altered metabolism, and ultimately, weight gain.
The following examples showcase different facets of this complex relationship.
A Case Study of Cortisol Dysregulation and Weight Gain
Sarah, a 35-year-old marketing executive, experienced consistent stress due to demanding deadlines and high-pressure work environments. She reported increased cravings for sugary and fatty foods, particularly in the evening. Her cortisol levels, consistently elevated, contributed to insulin resistance, leading to weight gain around her midsection. Sleep disturbances were also observed, further compounding the issue. Her weight gain pattern wasn’t simply about overeating; it was a direct result of her body’s physiological response to chronic stress, affecting her metabolism and appetite regulation.
Sarah’s case underscores how stress-induced cortisol imbalances can impact weight management strategies.
A Hypothetical Scenario for Weight Management Improvement
Imagine Mark, a 40-year-old software developer, struggling with stubborn belly fat despite a healthy diet and exercise routine. Recognizing the potential role of cortisol, he implemented stress-reduction techniques like meditation and yoga into his daily schedule. He also made adjustments to his diet, focusing on foods that support cortisol regulation, such as lean proteins and complex carbohydrates. By addressing his cortisol levels, Mark noticed a significant shift in his weight management journey.
He not only experienced improved sleep quality but also a reduction in cravings, leading to sustainable weight loss. This scenario exemplifies how incorporating cortisol-regulating strategies into a comprehensive weight management plan can yield positive results.
A Fictional Story Illustrating the Impact of Stress and Cortisol on Health and Weight
Amelia, a young artist, found her creative energy dwindling amidst the pressures of a demanding art school. Constant deadlines and critical feedback triggered a surge in cortisol. She found herself constantly reaching for comfort foods like pastries and chocolate, exacerbating the weight gain she was experiencing. Her sleep was interrupted, her energy levels were low, and her overall well-being deteriorated.
As her stress levels persisted, so did the weight gain. Amelia’s story demonstrates how prolonged stress, fueled by elevated cortisol, can negatively impact not only weight but also mental and physical well-being.
A Real-World Situation Where a Weight Management Plan Failed Due to Cortisol Issues
Emily, a 28-year-old nurse, followed a strict low-calorie diet and intense exercise regimen for weight loss. Despite her dedication, progress was slow and eventually stalled. Underlying cortisol issues, stemming from the demanding nature of her job, were impacting her body’s ability to effectively utilize nutrients and burn calories. She experienced frequent cravings, particularly for high-carbohydrate foods, and her body struggled to maintain a healthy metabolism.
Her weight loss plan failed not because of a lack of effort but because a key factor—cortisol dysregulation—had been overlooked. This illustrates the importance of considering the role of stress and cortisol in weight management plans.
Epilogue
In conclusion, the cortisol weight loss controversy highlights the intricate interplay between hormones, stress, and lifestyle choices. While cortisol plays a crucial role in our bodies, its impact on weight is far more nuanced than a simple cause-and-effect relationship. Understanding the nuances of this complex issue can lead to more effective and sustainable weight management strategies. The key is to find balance and to manage stress, which ultimately affects cortisol levels and our overall well-being.