Spending the first night using CPAP sets the stage for a transformative journey toward better sleep. This experience, while potentially daunting, can be smoother than you imagine with the right preparation. We’ll explore everything from essential equipment and setup to troubleshooting common issues, and ultimately, how your first night with CPAP affects your overall sleep quality.
From selecting the perfect mask to understanding CPAP settings, this guide provides a detailed, step-by-step approach to make your initial CPAP experience as comfortable and effective as possible. We’ll cover potential discomfort, common adjustments, and how to address any problems that may arise during your first night. You’ll also discover practical strategies for achieving a positive and successful transition into CPAP therapy.
Initial Setup and Preparation
Embarking on your CPAP journey begins with careful preparation. Understanding the equipment, mastering the setup process, and choosing the right mask are crucial for a comfortable and effective first night. This section details the essential steps to ensure a smooth transition into CPAP therapy.
Essential Equipment
Your CPAP journey necessitates a specific set of equipment. The core components include the CPAP machine itself, a mask, tubing, and an optional humidifier. The machine provides the pressurized air, the mask delivers the air to your airways, the tubing connects them, and the humidifier, if used, adds moisture to the air, often important for preventing dryness.
Setting Up the CPAP Machine and Mask
A proper setup is paramount to a comfortable CPAP experience. Following these steps will ensure you’re using your CPAP machine correctly from the start.
- Unpack all components and familiarize yourself with the CPAP machine, mask, and tubing.
- Connect the CPAP machine to a power source.
- Attach the tubing to the CPAP machine and the mask.
- Adjust the mask to your face and ensure a proper seal. Experiment with different positions to optimize fit.
- Turn on the CPAP machine and monitor the pressure settings as displayed on the machine’s control panel.
- Check for leaks by listening to the machine’s air flow. Leaks often cause a hissing sound.
- If using a humidifier, add water to the reservoir according to the manufacturer’s instructions.
Mask Types and Facial Structures
The choice of mask significantly impacts the comfort and effectiveness of CPAP therapy. Different mask types cater to diverse facial structures, and proper selection is key to a successful treatment.
- Full Face Masks: These masks cover the entire nose and mouth, providing a complete seal. Suitable for individuals with significant facial issues that affect a good nasal or oral seal, or for those who experience difficulty breathing through their nose. They can offer a more stable and consistent air delivery.
- Nasal Masks: These masks cover only the nose, often with a cushioned nasal bridge and straps. They are frequently favored for their ease of use and potential for a more discreet appearance. Nasal masks might be more suitable for individuals who breathe primarily through their nose.
- Nasal Pillow Masks: These masks use small, flexible cushions that rest on the nasal passages. They are known for their light weight and potentially better comfort for individuals with sensitive or narrow noses.
- Full Face Masks: These masks cover the entire nose and mouth, providing a complete seal. They are often preferred for individuals with significant facial issues that affect a good nasal or oral seal.
Potential Discomfort and Alleviation Strategies
Initial CPAP use can sometimes lead to discomfort, but strategies exist to mitigate these issues.
- Dry Mouth: Adding a humidifier to the CPAP machine can help alleviate dryness. Ensure proper hydration throughout the day is also crucial.
- Facial Pressure: Experiment with different mask types and sizes to find the best fit. Proper mask adjustment is essential. Adjusting straps can also alleviate pressure points.
- Air Leaks: Ensure a tight seal by adjusting the mask’s position. If leaks persist, consult with a healthcare provider for further assistance.
CPAP Mask Type Comparison
| Mask Type | Material | Features | Potential Issues |
|---|---|---|---|
| Full Face | Silicone, Foam | Complete seal, often adjustable | May cause skin irritation, limited mobility |
| Nasal | Silicone, Foam | Lightweight, less bulky | Potential for nasal discomfort, limited seal for mouth breathers |
| Nasal Pillow | Soft silicone | Lightweight, gentle on the nose | May not provide adequate seal for mouth breathers, potential for air leakage |
First Night Experience: Spending The First Night Using Cpap
My first night using CPAP was a mix of anticipation and apprehension. I’d meticulously prepared the equipment, ensuring everything was set up correctly, and now the real test had begun. I was eager to see if this therapy would help me get the rest I needed, but also nervous about the potential challenges.The experience is often described as a journey of adjustment, and mine was no exception.
It’s important to understand that the first night is frequently marked by a blend of sensations, from the initial feeling of the mask to the subtle pressure adjustments.
Typical Sensations and Emotions
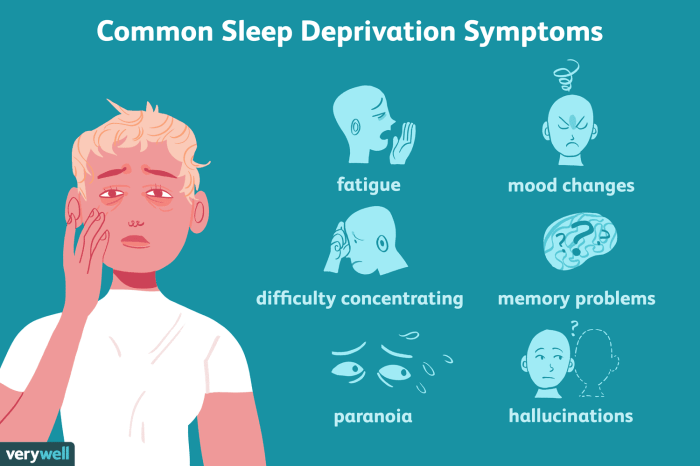
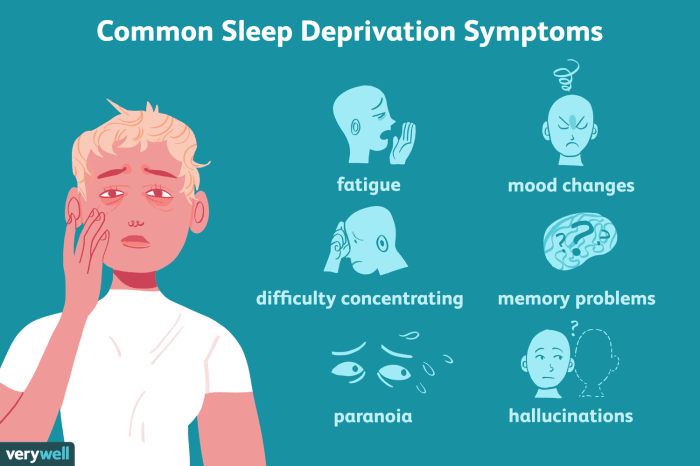
The first night often brings a range of sensations. You might feel pressure on your nose and face from the mask, and the unfamiliar sound of the machine may be disconcerting. Discomfort is quite common, and some individuals experience slight dryness or soreness in their nose or mouth due to the airflow. Emotions can vary from mild frustration to a sense of relief once the body adjusts.
Common Adjustments and Modifications
It’s not uncommon to need to make adjustments to the CPAP settings during the initial night. You may notice that the prescribed pressure isn’t optimal for you, and you might find yourself experimenting with different settings. This could include slightly increasing or decreasing the pressure to find a comfortable and effective level. You might also need to adjust the mask fit, ensuring a proper seal to prevent leaks.
The goal is to minimize discomfort and maximize the effectiveness of the therapy.
Potential Obstacles and Challenges
The first night with CPAP can present several challenges. One common obstacle is mask leaks. A poor mask seal can lead to air escaping and a less effective therapy. Another challenge is the pressure itself. The prescribed pressure might feel uncomfortable, especially if it’s too high or if the patient is not used to it.
Adjusting to the new sensation and the noise of the machine can also be difficult for some individuals. Additionally, the dryness associated with the airflow can become bothersome.
Examples of Common Issues
Mask Leaks
A loose or improperly fitted mask can lead to air escaping, reducing the effectiveness of the therapy and causing discomfort. This can be addressed by adjusting the mask straps, trying a different mask type, or seeking guidance from a healthcare professional.* Pressure Discomfort: A pressure setting that’s too high or too low can lead to discomfort.
Gradually adjusting the pressure according to the recommended guidelines is key. A CPAP machine with a ramp feature can ease this transition by starting with lower pressure and gradually increasing it.* Difficulties Adjusting: The transition to CPAP can be challenging. The unfamiliar sensations, sounds, and adjustments can be overwhelming. Taking your time, seeking support from healthcare professionals, and being patient with yourself are crucial.
Potential Issues and Solutions
| Potential Issue | Possible Solution |
|---|---|
| Mask Leaks | Adjust mask fit, try a different mask type, consult with a healthcare professional. |
| Pressure Discomfort | Gradually adjust pressure according to guidelines, utilize ramp feature on CPAP machine, and consult a healthcare professional. |
| Difficulties Adjusting | Take your time, seek support from healthcare professionals, be patient with yourself. |
Troubleshooting and Adjustments
Navigating the first few nights with CPAP can be tricky. It’s completely normal to experience some discomfort or issues as you adjust to the device. This section Artikels common problems and how to address them, emphasizing the crucial role of your healthcare provider in this process.Successfully adapting to CPAP requires a combination of understanding the device, identifying potential problems, and making appropriate adjustments.
Your healthcare professional is your best resource, offering personalized guidance and support to ensure a comfortable and effective treatment journey.
Common CPAP Issues and Troubleshooting
Understanding potential issues on your first night with CPAP allows for proactive problem-solving. This section details common problems and how to address them.
- Mask Leaks: Mask leaks are a frequent complaint. A poorly fitting mask can lead to air escaping and reduced effectiveness. Ensure the mask seals snugly around your nose and mouth. Adjust the straps for a comfortable, yet secure fit. If the problem persists, consider different mask types, like nasal pillows or full face masks, or consult your healthcare provider to determine if a custom-fit mask is appropriate.
- Airflow Discomfort: Excessive or insufficient airflow can cause discomfort. Adjust the pressure settings as recommended by your healthcare professional. A gradual increase in pressure is often necessary to optimize therapy.
- Dry Mouth/Nose: Dry mouth and nose are common side effects. Using a humidifier with your CPAP machine can significantly reduce this dryness. Adjust the humidifier settings to your comfort level.
- Headaches: Headaches can be a symptom of improper pressure settings or mask fit. Consult your healthcare provider to assess the optimal pressure and mask type for your needs.
- Other Issues: If you experience other problems, such as difficulty breathing or chest discomfort, contact your healthcare provider immediately.
Role of Healthcare Professionals
Your healthcare professional plays a vital role in your CPAP journey. They provide personalized guidance, answer your questions, and monitor your progress.
- Personalized Guidance: Healthcare professionals provide personalized advice tailored to your specific needs and medical history.
- Monitoring Progress: They track your progress and adjust the treatment plan as needed.
- Addressing Concerns: They address your concerns, alleviate discomfort, and provide reassurance.
- Equipment Recommendations: They can recommend suitable mask types and pressure settings to ensure optimal comfort and effectiveness.
Mask Fit and Pressure Settings
Proper mask fit and pressure settings are essential for effective CPAP therapy. Incorrect settings can lead to discomfort, reduced effectiveness, and potential side effects.
- Mask Fit: A well-fitting mask ensures that air is delivered effectively and comfortably. A proper fit is crucial for successful treatment.
- Pressure Settings: Pressure settings should be optimized by your healthcare provider. Starting with lower settings and gradually increasing them is a common approach.
Adjusting CPAP Settings
Adjusting CPAP settings based on your feedback is a critical aspect of optimizing therapy.
- Listening to Feedback: Pay close attention to how your body reacts to different settings. Document any discomfort or improvement in sleep quality.
- Gradual Adjustments: Make gradual adjustments to pressure settings, never exceeding recommended levels without consulting your healthcare provider.
CPAP Settings and Sleep Quality, Spending the first night using cpap
This table illustrates how different CPAP settings can potentially impact sleep quality.
| CPAP Setting | Potential Impact on Sleep Quality |
|---|---|
| Low Pressure | May not be sufficient to maintain airway pressure, potentially reducing effectiveness |
| High Pressure | May cause discomfort, including nasal dryness or pain. It may interfere with sleep and reduce overall comfort |
| Optimal Pressure | Facilitates a consistent airway opening, leading to improved sleep quality and reduced sleep disturbances |
Sleep Quality and Outcomes
My first night with CPAP was a mix of anticipation and trepidation. I’d read countless stories, some positive, some filled with initial struggles. I was curious about how my sleep quality would change, and if the experience would live up to my expectations.The first night on CPAP is often a crucial indicator of how the device will integrate into your overall sleep routine.
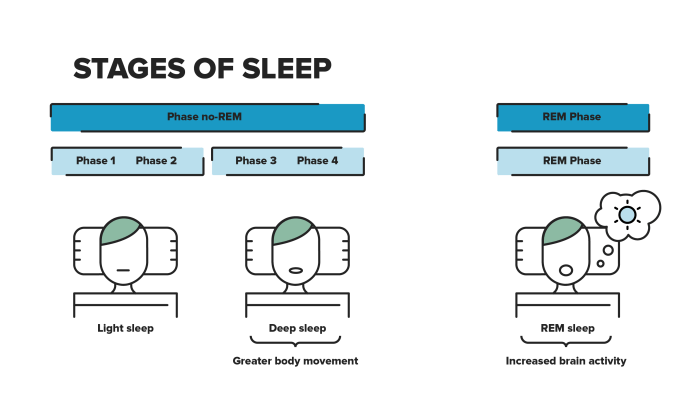
It’s a transition period, where your body adjusts to the pressure and the new sensation of the mask. This adjustment period often directly influences your first night’s sleep quality and is a significant factor in the long-term success of CPAP therapy.
Assessing First Night Sleep Quality
Sleep quality on the first night of CPAP usage is often assessed by subjective reports and objective measurements. Subjective reports, such as self-assessment questionnaires, can gauge overall satisfaction and comfort. Objective measurements, like sleep studies (polysomnography) or CPAP machine data logs, provide quantifiable metrics. These measures offer insight into factors like sleep stages, breathing patterns, and the effectiveness of the CPAP treatment.
My first night with CPAP was surprisingly easy, though a little noisy. Adjusting to the mask took a few minutes, but once I got comfortable, the whole experience was surprisingly peaceful. Trying to figure out how to get dementia patients to eat can be a real challenge, just like the initial discomfort of a new CPAP machine. Luckily, there are helpful resources available, like this guide on how to get dementia patients to eat , that provide tips and tricks.
Overall, the first night wasn’t as bad as I anticipated, and I’m feeling much better now.
Differences from Prior Sleep
The first night of CPAP usage can significantly differ from previous sleep experiences. You may experience a feeling of fullness or pressure in your face, or discomfort from the mask. A change in breathing patterns and reduced snoring are common observations. A feeling of disorientation or difficulty adjusting to the device is also typical. The introduction of the mask and the unfamiliar pressure may initially interrupt your usual sleep cycle.
Comparing First Night to Expectations
Often, the first night’s sleep quality doesn’t meet expectations. The unfamiliar sensations and the need to adjust to the mask can lead to a restless night. However, many users report that the first night’s discomfort is often superseded by improved sleep quality in subsequent nights. This improvement is usually related to the body’s adjustment to the CPAP machine.
Individual experiences can vary, with some individuals experiencing minimal disruption.
Tracking Sleep Quality After the First Night
Regular tracking of sleep quality after the first night is essential for monitoring progress and making adjustments to the CPAP settings. This process allows you to see how your sleep quality evolves over time. Tracking also allows you to identify any problems or areas that require further adjustments.
My first night using CPAP was surprisingly manageable. I was a bit nervous, of course, but the machine wasn’t as loud as I’d imagined. It was definitely an adjustment, but the relief from sleep apnea symptoms was worth it. Learning about the potential link between sleep apnea and respiratory conditions like pneumonia vs lung cancer really made me appreciate the importance of getting treatment.
Pneumonia vs lung cancer are both serious, and understanding the differences is crucial. Overall, despite the initial adjustment period, the first night went much better than expected and I’m already feeling the benefits.
Sleep Quality Tracking Methods
Consistent tracking of sleep quality after the first night is essential to measure the effectiveness of CPAP therapy. This involves both subjective and objective methods.
| Method | Description | Pros | Cons |
|---|---|---|---|
| Self-Assessment | Keeping a sleep diary, noting sleep duration, quality, and any discomfort. | Easy to implement, provides insights into subjective experience. | Subjectivity can introduce bias, doesn’t offer detailed physiological data. |
| CPAP Machine Logs | Reviewing the CPAP machine’s data, including hours of use, pressure settings, and leaks. | Provides objective data, tracks adherence. | Requires technical understanding of the machine’s output, data may be complex to interpret. |
| Sleep Tracking Apps | Using wearable devices or smartphone apps to monitor sleep patterns. | Offers comprehensive data on sleep stages, heart rate, and other parameters. | Accuracy can be affected by the quality of the device, requires consistent use. |
| Sleep Studies (Polysomnography) | Formal sleep studies conducted by a sleep specialist, using various sensors. | Provides the most comprehensive data on sleep quality, identifies specific sleep disorders. | Expensive, may require travel to a specialized facility, takes time to schedule. |
Patient Education and Support
Navigating the initial stages of CPAP therapy can be challenging. Understanding the importance of proper patient education and support systems is crucial for successful long-term adherence and positive outcomes. A well-informed patient is more likely to successfully integrate CPAP into their daily routine and experience the therapeutic benefits. This section will Artikel the critical role of education, support resources, and maintaining motivation throughout the CPAP journey.
My first night using CPAP was definitely an adjustment. I’d read about how important it is for managing breathlessness, a common side effect of many lung conditions, including lung cancer treatments. Breathlessness with lung cancer treatments can be particularly challenging, and I found the initial CPAP pressure a little overwhelming. However, once I got used to it, the difference in my breathing was noticeable, and I slept much better than I had in a long time.
It really made a difference.
Importance of Patient Education
Patient education during the first night of CPAP use is vital. Clear and concise instructions regarding CPAP machine operation, mask fitting, and potential side effects are essential. This empowers patients to actively participate in their therapy and address any concerns promptly. Proper education helps patients understand the rationale behind CPAP therapy, reducing anxiety and increasing their likelihood of successful adaptation.
Resources for Supporting Patients
Numerous resources are available to support patients during their initial CPAP adaptation. These resources provide guidance and practical assistance to help patients adjust to the therapy.
- Healthcare Professionals: Physicians, respiratory therapists, and sleep specialists are crucial resources. They can provide personalized guidance, address specific concerns, and adjust the CPAP settings as needed. Regular follow-up appointments are essential to monitor progress and make necessary adjustments to the therapy.
- Patient Handbooks and Online Materials: Detailed information about CPAP machines, mask types, and potential side effects can be found in patient handbooks and online resources. These resources provide a comprehensive overview of the therapy and empower patients with the knowledge they need.
- Support Groups: Connecting with other CPAP users can provide invaluable support and encouragement. Support groups offer a platform for sharing experiences, asking questions, and learning coping strategies from those who have already navigated similar challenges.
Role of Support Groups
Support groups play a significant role in helping patients overcome the challenges associated with CPAP therapy. The shared experiences and encouragement within these groups can foster a sense of community and belonging. Members can offer practical advice, share coping strategies, and provide emotional support. This sense of camaraderie can help patients feel less isolated and more motivated to continue their therapy.
For example, a support group might share tips for dealing with mask discomfort or offer encouragement to patients who are struggling with sleep quality improvements.
Maintaining a Positive Mindset and Motivation
Maintaining a positive mindset and motivation is crucial for ongoing CPAP therapy. Patients should focus on the long-term benefits of CPAP therapy, such as improved sleep quality, reduced daytime sleepiness, and overall health improvement. It is important to celebrate small victories and acknowledge the progress made.
- Setting Realistic Expectations: It is important to set realistic expectations for the initial adaptation phase. Adjustments to CPAP therapy may take time, and setbacks are common. Understanding that the journey may not be seamless can help to manage expectations.
- Seeking Support from Loved Ones: Involving loved ones in the journey can provide emotional support and encouragement. Communicating the challenges and successes with family and friends can create a supportive network.
- Rewarding Progress: Recognizing and rewarding progress can reinforce positive behavior and maintain motivation. This could include celebrating milestones like consistently using CPAP for a week or experiencing improved sleep quality.
Summary of Resources for Patients and Caregivers
| Category | Resources |
|---|---|
| Healthcare Professionals | Physicians, respiratory therapists, sleep specialists |
| Patient Information | Patient handbooks, online resources, support groups |
| Support Networks | Family, friends, support groups |
Illustrative Examples

Embarking on CPAP therapy can be a journey with both exhilarating successes and initial hurdles. Understanding different experiences, from smooth transitions to those requiring troubleshooting, can help ease anxieties and build confidence in the process. This section provides concrete examples to illustrate the diverse possibilities of your CPAP journey.
A Positive First-Night Experience
A typical positive first-night experience involves a gradual adjustment to the unfamiliar sensation of the mask and the gentle airflow. Sarah, a patient new to CPAP, reported feeling a slight pressure initially but quickly found comfort. She meticulously followed the instructions for mask sizing and placement, ensuring a snug yet comfortable fit. The gentle hum of the machine and the steady airflow soon became background noise, allowing her to drift off to sleep without interruption.
Waking up felt refreshing, with a clear head and an overall sense of well-being.
Challenges and Successful Troubleshooting
Not every first night is a breeze. Mark, a new CPAP user, experienced some initial discomfort with the mask and occasional leaks. He meticulously reviewed the mask fitting instructions and adjusted the straps to achieve a more secure fit. He also experimented with different mask types to find the most comfortable option. A consultation with his sleep specialist helped him determine that the leak was due to a minor issue with the mask seal.
A simple adjustment resolved the issue, and Mark reported a significantly improved sleep experience on subsequent nights.
Patience and Persistence in Overcoming Initial Difficulties
Adjusting to CPAP therapy often requires patience and persistence. Initial discomfort, such as dryness, pressure, or leaks, is common and often temporary. Successful adaptation often depends on proactive troubleshooting, communication with healthcare professionals, and a commitment to consistent use. Many patients report that the initial difficulties gradually diminish as they become accustomed to the device. The benefits of consistent use far outweigh the temporary challenges.
Long-Term Benefits of CPAP Therapy
The long-term benefits of CPAP therapy are substantial. Studies have shown that CPAP therapy can significantly improve daytime alertness, reduce snoring, and enhance overall quality of life. By improving sleep quality, CPAP therapy can lead to increased productivity, reduced irritability, and improved emotional well-being. Individuals with sleep apnea often experience improved cardiovascular health, reduced risk of stroke, and an overall improvement in physical health.
A Well-Fitted CPAP Mask Illustration
Imagine a CPAP mask snugly fitting the face, conforming to the contours without causing pressure points or discomfort. The mask’s edges are firmly sealed to the face, creating a complete air-tight seal. The straps are adjusted to a comfortable tension, evenly distributing pressure and preventing any slippage. The mask’s design allows for ample airflow while maintaining a secure fit, allowing for a restful sleep experience.
This illustration represents a well-fitted CPAP mask, which is crucial for effective treatment.
Final Summary

Successfully navigating the first night using CPAP is a crucial step towards a healthier sleep routine. Remember, patience and persistence are key. While initial adjustments might seem challenging, the long-term benefits of consistent CPAP therapy far outweigh the short-term hurdles. This experience is highly personal, and your healthcare professional is your best resource for support and guidance throughout this journey.
The insights and tools shared here empower you to confidently embrace CPAP and experience the transformative impact on your overall well-being.