What causes sleep related hallucinations – What causes sleep-related hallucinations? This fascinating topic delves into the mysterious world of hypnagogic and hypnopompic experiences, exploring the neurological, psychological, and environmental factors that can trigger them. We’ll uncover the science behind these vivid dreamscapes, from the role of sleep deprivation to the influence of medications and underlying medical conditions. Get ready for an in-depth journey into the captivating realm of sleep-related hallucinations.
Sleep-related hallucinations, often vivid and unsettling, can range from fleeting glimpses to full-blown, disturbing experiences. These episodes can occur at the onset or during the end of sleep, impacting sleep quality and overall well-being. Understanding the underlying causes is crucial for effective management and prevention strategies.
Defining Sleep-Related Hallucinations
Sleep-related hallucinations are vivid sensory experiences that occur during specific stages of sleep. These experiences can range from unsettling to frightening, impacting both the individual’s sleep quality and overall well-being. Understanding the different types and characteristics of these hallucinations is crucial for recognizing and addressing potential underlying issues. They are distinct from other sleep disorders, often presenting with unique symptom patterns.Sleep-related hallucinations are not a single disorder but rather a group of experiences that arise during specific transitions in sleep.
These hallucinations are generally harmless but can cause distress and disruption. The ability to distinguish these from other sleep disorders is important for appropriate intervention.
Types of Sleep-Related Hallucinations
Sleep-related hallucinations encompass a spectrum of experiences, primarily occurring during the transition between wakefulness and sleep. Hypnagogic and hypnopompic hallucinations are the most common types.
Hypnagogic Hallucinations
These sensory experiences occur as one is falling asleep. The individual is usually in a state of drowsiness, often just before sleep onset. Common characteristics include visual hallucinations, which can be vivid and detailed. Auditory hallucinations, such as voices or sounds, are also possible. Other sensations, such as feeling a presence or physical sensations, can also accompany the visual and auditory components.
These hallucinations typically last for a few seconds to a few minutes.
Hypnopompic Hallucinations
These hallucinations occur as one is waking up. The individual is often still in a state of drowsiness, with a sense of disorientation. Hypnopompic hallucinations often share similar characteristics with hypnagogic hallucinations, including visual and auditory components. The individual might experience a feeling of being attacked or chased, which can heighten the fear and distress associated with these experiences.
These hallucinations are often shorter in duration than hypnagogic hallucinations.
Sleep-related hallucinations can stem from various factors, like sleep deprivation or certain medical conditions. However, seasonal changes can also play a role, particularly with Seasonal Affective Disorder (SAD). If you’re struggling with SAD, exploring strategies like light therapy, maintaining a regular sleep schedule, and adjusting your diet could be helpful. 4 ways to tackle seasonal affective disorder might offer some valuable insights.
Ultimately, understanding these contributing factors is key to effectively managing sleep-related hallucinations.
Comparison with Other Sleep Disorders, What causes sleep related hallucinations
Sleep-related hallucinations are distinct from other sleep disorders, although overlapping symptoms can occur. Distinguishing features include the sensory nature of the experience and the specific timing associated with transitions between wakefulness and sleep. For example, nightmares are often more narrative-based and occur during REM sleep, a deeper stage of sleep. Sleep paralysis is characterized by the inability to move or speak while falling asleep or waking up.
The lack of clear sensory imagery distinguishes it from sleep-related hallucinations.
Age and Prevalence
Sleep-related hallucinations are relatively common, with a range of prevalence across different age groups. These experiences are typically reported in children, adolescents, and adults. They are frequently encountered in clinical practice, especially among younger adults.
| Type | Description | Symptoms | Prevalence |
|---|---|---|---|
| Hypnagogic | Hallucinations occurring as one is falling asleep | Visual, auditory, or other sensory experiences. Commonly vivid and detailed visual imagery. | Reported in a significant percentage of the population, particularly in young adults. |
| Hypnopompic | Hallucinations occurring as one is waking up | Similar sensory experiences as hypnagogic hallucinations, often accompanied by feelings of being attacked or chased. | Reported frequency comparable to hypnagogic hallucinations, potentially slightly lower in some studies. |
Underlying Causes of Sleep-Related Hallucinations

Sleep-related hallucinations, vivid sensory experiences during sleep transitions, can be unsettling but often have identifiable underlying causes. Understanding these factors can help individuals address these experiences and improve their sleep quality. While some cases are benign, others may indicate an underlying medical issue.Understanding the potential causes of sleep-related hallucinations is crucial for effective management and treatment. These experiences can range from unsettling to frightening, and identifying the root cause is often the first step towards alleviating them.
Medical Conditions Linked to Sleep-Related Hallucinations
Certain medical conditions can disrupt the brain’s normal sleep-wake cycle, leading to sleep-related hallucinations. These conditions may affect brain function or neurochemical balance, making them a significant factor in the development of these experiences. For example, conditions like narcolepsy, which involve excessive daytime sleepiness and cataplexy (sudden muscle weakness), often accompany sleep paralysis and hypnagogic hallucinations.
Sleep Deprivation and Poor Sleep Hygiene
Chronic sleep deprivation and poor sleep hygiene significantly contribute to sleep-related hallucinations. Consistent lack of adequate sleep disrupts the natural sleep cycles, leading to fragmented sleep and increased vulnerability to these types of experiences. Poor sleep hygiene practices, such as irregular sleep schedules, excessive screen time before bed, and an uncomfortable sleep environment, also disrupt the body’s natural sleep-wake rhythm.
These factors can increase the likelihood of experiencing sleep-related hallucinations.
Substance Use and Sleep-Related Hallucinations
Substance use, both recreational and prescription, can induce sleep-related hallucinations. Certain substances, such as alcohol, certain medications, and illicit drugs, can interfere with normal brain function during sleep. Alcohol use, for instance, can disrupt sleep cycles and increase the likelihood of vivid dreams or hallucinations. It’s essential to note that the impact varies greatly based on the specific substance, dose, and individual factors.
Impact of Medications and Potential Side Effects
Medications, including certain prescription drugs, can have side effects that contribute to sleep-related hallucinations. Some medications can disrupt neurotransmitter balance, impacting the brain’s sleep-wake cycle and increasing the risk of hallucinations. This can be especially concerning for individuals with pre-existing sleep disorders or neurological conditions.
Comparison of Causes of Sleep-Related Hallucinations
| Category | Cause | Description | Examples |
|---|---|---|---|
| Medical Conditions | Narcolepsy, Alzheimer’s disease, Parkinson’s disease | Conditions that affect brain function or neurochemical balance | These conditions may cause disruptions in the sleep-wake cycle. |
| Sleep Deprivation and Poor Sleep Hygiene | Insufficient sleep, irregular sleep schedules | Disruption of natural sleep cycles | Consistent sleep deprivation can lead to fragmented sleep and heightened susceptibility to hallucinations. |
| Substance Use | Alcohol, illicit drugs, certain medications | Interference with normal brain function during sleep | Alcohol can disrupt sleep cycles and increase the risk of hallucinations. Specific medications may have sleep-disrupting side effects. |
| Medication Side Effects | Certain prescription drugs | Disruption of neurotransmitter balance | Some medications can disrupt the brain’s sleep-wake cycle. |
Neurological Mechanisms
Sleep-related hallucinations aren’t just bizarre dreams; they’re a disruption in the normal neurological processes of sleep. Understanding the intricate interplay of brain activity during sleep and how it can go awry is key to comprehending these experiences. This involves delving into the normal sleep cycle, the regions of the brain involved, and the potential neurochemical imbalances that contribute to these unusual events.The neurological underpinnings of sleep-related hallucinations are multifaceted, drawing from the complex interplay of brain regions and neurochemicals during various stages of sleep.
Sleep itself isn’t a passive state; rather, it’s a dynamic process with distinct stages characterized by varying levels of brain activity. Understanding these stages is crucial to understanding why hallucinations might arise.
Normal Sleep and Dreaming
The brain cycles through different sleep stages, each with its unique characteristics in terms of brain wave patterns and physiological activity. These stages include Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. NREM sleep is further divided into stages 1 through 3, progressively characterized by slower brain waves. REM sleep is associated with vivid dreaming and increased brain activity, resembling wakefulness in many aspects.
During REM sleep, the brain’s activity is characterized by rapid, low-voltage brain waves, increased eye movements, and muscle paralysis. These characteristics play a critical role in the generation of dreams.
Disruptions in Normal Sleep Processes
Sleep-related hallucinations often arise when the normal sleep processes are disrupted. This can occur due to various factors, from underlying medical conditions to medication side effects. For instance, certain neurological disorders, like dementia or Parkinson’s disease, are frequently associated with sleep disturbances and hallucinations. The disruption can involve various stages, particularly the transition between sleep stages. A person might experience a vivid dreamlike experience during NREM sleep, or the normal muscle paralysis that accompanies REM sleep may be incomplete or absent, allowing the individual to act out their dreams.
Brain Regions in Hallucination Generation
Several brain regions are implicated in the generation of sleep-related hallucinations. The temporal lobe, particularly the hippocampus, plays a crucial role in memory consolidation and dream formation. Disruptions in this area can lead to fragmented or distorted memories, contributing to the hallucinatory experience. The prefrontal cortex, responsible for higher-level cognitive functions, may also be involved in the filtering and interpretation of sensory information during sleep, and its dysfunction can lead to misinterpretations of internal stimuli.
The amygdala, involved in emotional processing, can also contribute to the intensity and emotional content of the hallucinations.
Neurochemical Imbalances
Neurochemical imbalances are another potential contributor to sleep-related hallucinations. Acetylcholine, a neurotransmitter associated with attention and arousal, may be involved in the heightened sensory experiences during hallucinations. Serotonin and dopamine, neurochemicals associated with mood regulation, also play a role in sleep-wake cycles. Imbalances in these neurochemicals can affect the regulation of sleep stages and potentially lead to the formation of hallucinations.
For example, anticholinergic medications, which block acetylcholine, are known to be associated with hallucinations.
Visual Representation of Brain Activity
Imagine a dynamic brain map, representing brain activity during sleep. During normal REM sleep, specific regions light up in a complex pattern, signifying increased neuronal activity, corresponding to the dream state. Regions associated with memory, emotion, and sensory processing show heightened activity, but the prefrontal cortex, which normally helps filter and interpret information, shows relatively lower activity. In contrast, during sleep-related hallucinations, the pattern becomes irregular, showing abnormal activity in some areas.
The activity in the prefrontal cortex might be very low, and the activity in regions associated with sensory processing, like the visual cortex, might be abnormally high. This heightened activity in sensory regions could lead to the misinterpretation of internal stimuli as external realities. The entire map is distorted in places, with areas showing both high and low activity, not in a well-regulated manner.
Psychological Factors
Sleep-related hallucinations aren’t solely a neurological phenomenon. Psychological factors play a significant role in their occurrence and intensity. Anxiety, stress, and mental health conditions can create a fertile ground for these vivid, unsettling experiences. Understanding these psychological underpinnings is crucial for developing comprehensive treatment strategies.Psychological factors can influence the likelihood and severity of sleep-related hallucinations by impacting the brain’s state during sleep.
Stress and anxiety, for instance, can disrupt normal sleep patterns, leading to fragmented sleep and increased alertness. This heightened state of arousal can make individuals more susceptible to hallucinatory experiences. Furthermore, personality traits, coping mechanisms, and pre-existing mental health conditions can all contribute to the individual’s vulnerability.
Anxiety and Stress
Anxiety and chronic stress can significantly impact sleep quality and increase the likelihood of sleep-related hallucinations. The physiological effects of stress, such as elevated cortisol levels, can disrupt the normal sleep cycle, making individuals more prone to hallucinations. Furthermore, anxiety often involves intrusive thoughts and worries, which can seep into the dream state and contribute to the hallucinatory experience.
Individuals experiencing high levels of stress may also report more vivid and disturbing hallucinations.
Sleep-related hallucinations can stem from various factors, like stress, certain medications, or even underlying medical conditions. Interestingly, some studies suggest a potential link between sleep disturbances and antibiotic use, like those for urinary tract infections, antibiotics for urinary tract infections. This is a fascinating area of research, and further investigation is needed to fully understand the interplay between medication and these unusual sleep experiences.
Ultimately, more research is crucial to pinpoint the exact causes of these sleep-related hallucinations.
Mental Health Conditions
Mental health conditions, including depression, post-traumatic stress disorder (PTSD), and schizophrenia, have been linked to a higher incidence of sleep-related hallucinations. The underlying neurobiological and psychological processes associated with these conditions can disrupt the brain’s normal sleep mechanisms, leading to increased susceptibility. For example, individuals with PTSD may experience vivid nightmares and hallucinations that are related to traumatic events.
Personality Traits and Coping Mechanisms
Personality traits can also influence the experience of sleep-related hallucinations. Individuals with certain personality traits, such as neuroticism or high levels of anxiety, may be more susceptible to these experiences. Similarly, coping mechanisms employed by individuals to manage stress and anxiety can also play a role. For instance, some individuals may engage in maladaptive coping mechanisms, such as substance abuse, which can further exacerbate sleep disturbances and increase the likelihood of hallucinations.
Table: Psychological Factors and Sleep-Related Hallucinations
| Psychological Factor | Effect on Sleep-Related Hallucinations |
|---|---|
| Anxiety | Disrupts sleep patterns, increases arousal, allows intrusive thoughts to influence dream state, leading to more vivid and disturbing hallucinations. |
| Stress | Elevates cortisol levels, disrupts sleep cycle, increases susceptibility to hallucinations. |
| Mental Health Conditions (e.g., PTSD, Depression) | Disrupts normal sleep mechanisms, linked to increased incidence of sleep-related hallucinations, often related to underlying trauma or emotional distress. |
| Personality Traits (e.g., Neuroticism) | Increased susceptibility to sleep-related hallucinations due to heightened emotional reactivity and vulnerability. |
| Coping Mechanisms (e.g., Substance Abuse) | Can exacerbate sleep disturbances and increase the likelihood of hallucinations. |
Environmental Factors
Our sleep environment plays a surprisingly significant role in our overall sleep quality, and consequently, our susceptibility to sleep-related hallucinations. Factors like noise, light, and temperature can disrupt the delicate balance of our sleep cycles, making us more vulnerable to experiencing these vivid, often unsettling dream-like events. Understanding these environmental influences is crucial for managing and potentially preventing sleep-related hallucinations.
Impact of Noise on Sleep and Hallucinations
Noise, whether constant or intermittent, can significantly disrupt sleep. Sudden loud noises can jolt individuals out of sleep, disrupting the restorative processes vital for healthy sleep. Chronic exposure to even moderate levels of noise can lead to fragmented sleep, reducing the amount of deep sleep, which is associated with a higher risk of hallucinations. This lack of restorative sleep can negatively affect the brain’s ability to regulate dream activity, potentially contributing to sleep-related hallucinations.
Influence of Light on Sleep and Hallucinations
Light exposure, especially in the hours leading up to bedtime, can interfere with the body’s natural sleep-wake cycle. Exposure to bright light suppresses the production of melatonin, a hormone crucial for initiating and maintaining sleep. This disruption can result in difficulties falling asleep and staying asleep, increasing the likelihood of experiencing sleep-related hallucinations. Artificial light from electronic devices is a particularly significant factor, as the blue light emitted from these screens can be especially disruptive to melatonin production.
Impact of Temperature on Sleep and Hallucinations
Temperature fluctuations can significantly affect sleep quality. A bedroom that is either too hot or too cold can make it difficult to fall asleep and stay asleep. An uncomfortable temperature can lead to restless sleep, potentially increasing the likelihood of experiencing hallucinations. Optimizing the bedroom temperature to a comfortable range, ideally around 65-67°F (18-19°C), can improve sleep quality and reduce the risk of hallucinations.
Role of Sleep Environment in Hallucinations
The overall sleep environment profoundly impacts sleep quality. A chaotic or cluttered bedroom can create a sense of anxiety and stress, making it harder to relax and fall asleep. This stress can contribute to the occurrence of sleep-related hallucinations. Conversely, a calm, dark, and quiet bedroom environment promotes relaxation and enhances the likelihood of a restful night’s sleep, minimizing the risk of hallucinations.
Examples of Environmental Conditions Triggering Hallucinations
Environmental factors can act in concert to trigger sleep-related hallucinations. For example, a person sleeping in a dimly lit room with a ticking clock or nearby traffic noise may experience more vivid hallucinations. Similarly, a person sleeping in a hot, crowded room might have increased likelihood of sleep-related hallucinations compared to someone sleeping in a cool, quiet, and well-ventilated space.
Influence of Sleep Position and Sleep Environment
Sleep position and sleep environment are intertwined in their effect on sleep quality and the potential for hallucinations. Sleeping in an uncomfortable or unfamiliar position can disrupt sleep and increase the risk of sleep-related hallucinations. Furthermore, a sleep environment that is poorly organized or cluttered can increase stress and anxiety, leading to fragmented sleep and potentially inducing hallucinations.
A well-organized, comfortable, and familiar sleep environment can promote relaxation and improve sleep quality, reducing the risk of sleep-related hallucinations.
Diagnostic Considerations
Pinpointing the specific cause of sleep-related hallucinations is crucial for effective management. Accurate diagnosis hinges on a meticulous evaluation that considers various factors, from a comprehensive medical history to specialized sleep studies. This process allows clinicians to differentiate sleep-related hallucinations from other conditions with overlapping symptoms, ultimately guiding the most appropriate treatment plan.
Sleep-related hallucinations can stem from various factors, like stress or sleep deprivation. Interestingly, similar issues with sensory overload can arise from excessive earwax buildup in children, which can impact hearing and overall well-being. Learning how to prevent and treat excessive pediatric earwax can be beneficial for kids’ sleep and general health. For more on this topic, check out this helpful resource on how to prevent and treat excessive pediatric earwax.
Ultimately, understanding the root causes of sleep-related hallucinations is key to better sleep hygiene.
Methods Used to Diagnose Sleep-Related Hallucinations
A multi-faceted approach is employed to diagnose sleep-related hallucinations. This involves a thorough investigation of the patient’s medical history, a physical examination, and potentially, sleep studies. The combination of these methods provides a more comprehensive understanding of the individual’s condition, helping distinguish sleep-related hallucinations from other potential neurological or psychological issues.
Role of Sleep Studies in Evaluation
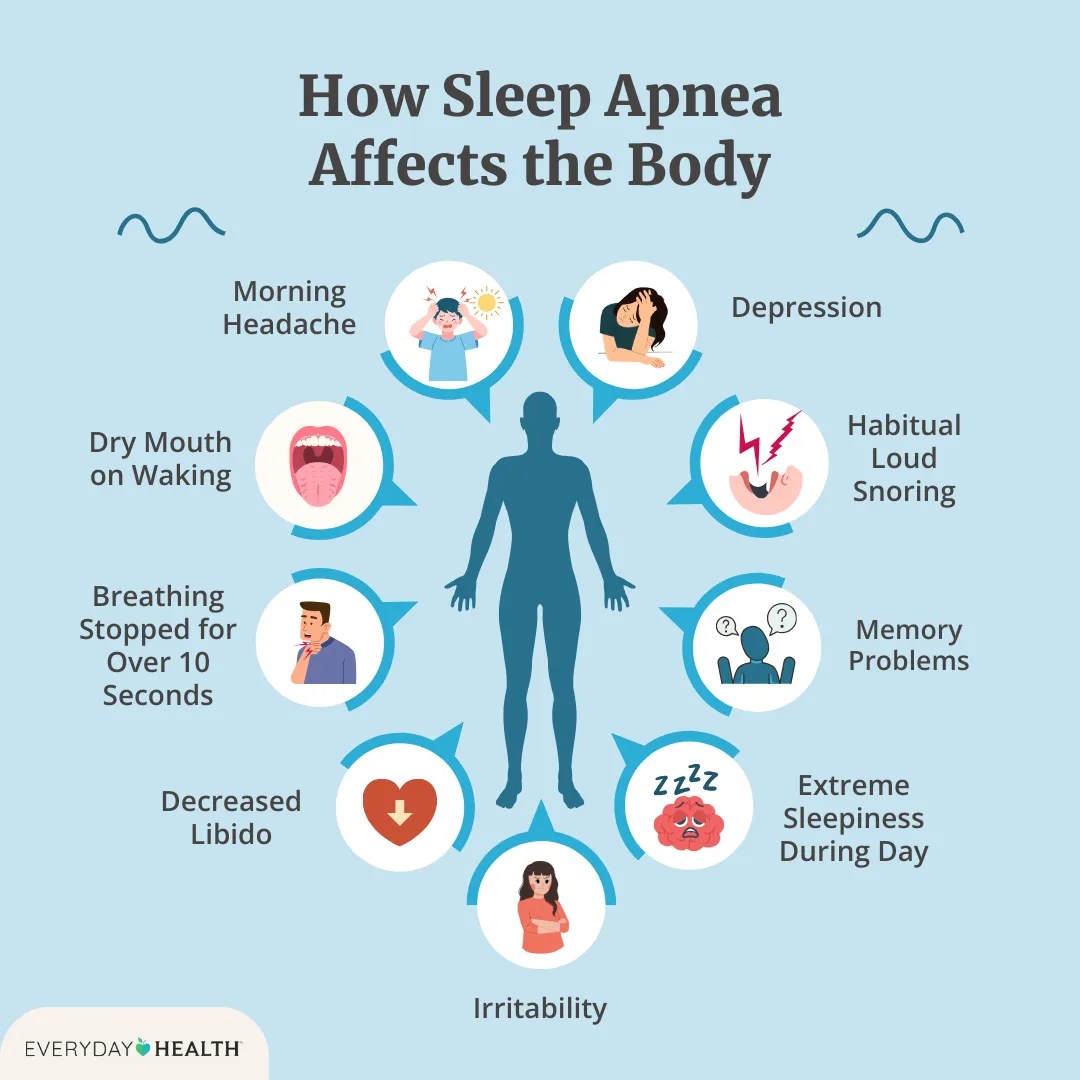
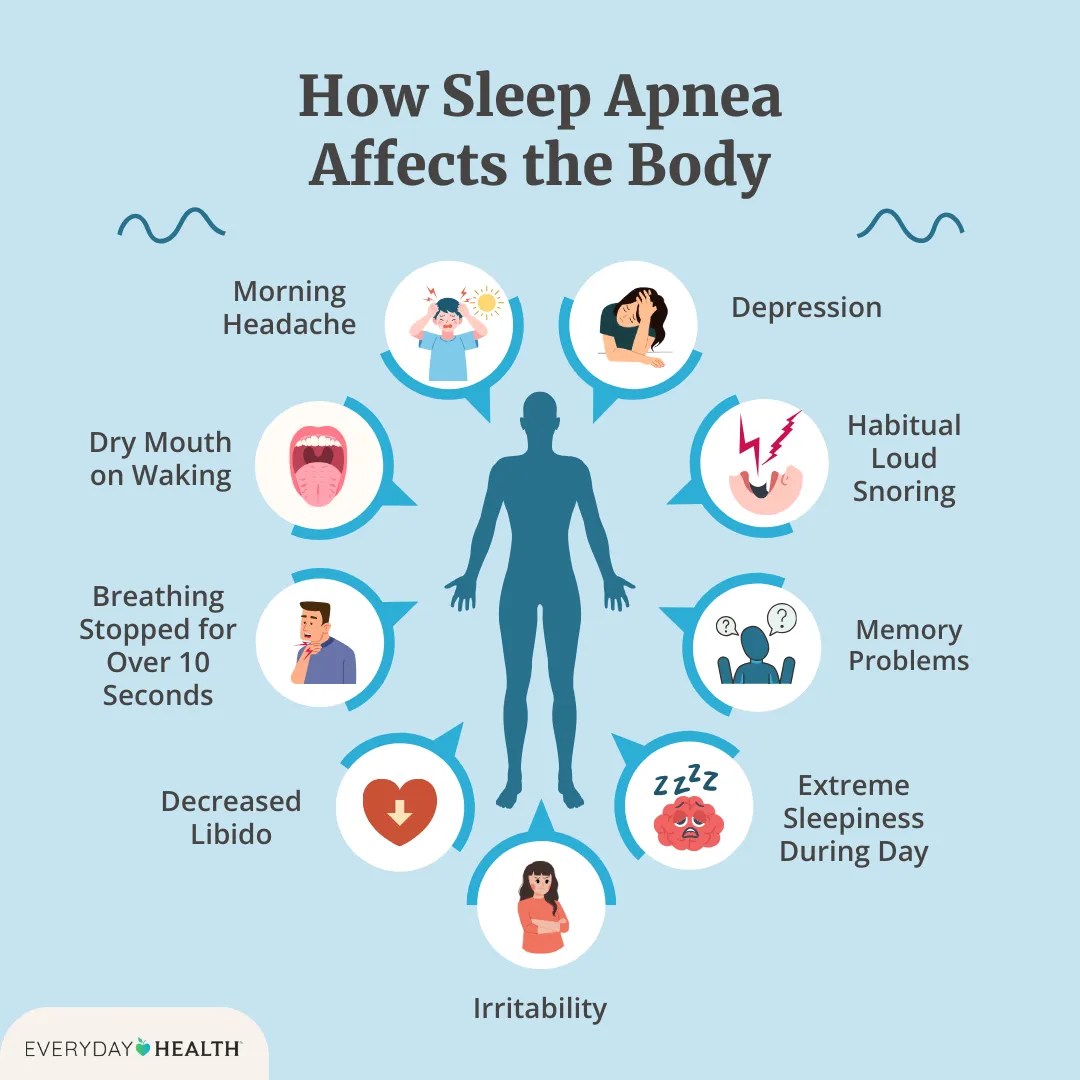
Polysomnography (PSG) plays a pivotal role in diagnosing sleep-related hallucinations. PSG is a comprehensive sleep study that monitors various physiological parameters during sleep. These parameters include brain waves, eye movements, muscle activity, heart rate, and breathing patterns. This comprehensive recording offers invaluable insights into the patient’s sleep architecture and can reveal any underlying sleep disorders, such as sleep apnea or narcolepsy, that might be contributing to the hallucinations.
By identifying abnormalities in sleep stages, clinicians can better understand the context of the hallucinations.
Significance of Comprehensive Medical History and Physical Examination
A thorough medical history is essential for identifying potential contributing factors. This includes inquiries about any pre-existing medical conditions, medications, substance use, and family history of neurological or psychiatric disorders. A physical examination provides objective data, helping rule out other conditions with similar symptoms. For example, a neurological examination can help assess the patient’s cognitive function and identify any signs of neurological dysfunction.
Flowchart of the Diagnostic Process
The following flowchart Artikels the general diagnostic process for sleep-related hallucinations:
| Step | Action | Possible Outcomes |
|---|---|---|
| 1 | Obtain detailed medical history, including sleep habits, medications, substance use, and family history. | Identification of potential contributing factors. |
| 2 | Conduct a comprehensive physical and neurological examination. | Rule out other neurological or medical conditions, identify potential physical issues. |
| 3 | Perform a polysomnography (PSG) sleep study. | Identification of sleep disorders, abnormal sleep patterns, and correlations with hallucinations. |
| 4 | Review all data and consider potential contributing factors. | Possible diagnosis of sleep-related hallucinations or identification of alternative diagnosis. |
| 5 | If indicated, consider additional testing, such as psychological evaluation, or specialized sleep studies. | Refine diagnosis, identify psychological or environmental triggers. |
Management and Treatment Strategies
Sleep-related hallucinations, while often unsettling, are manageable. Effective treatment hinges on understanding the underlying causes and employing a multifaceted approach. This often involves addressing both the immediate symptoms and the root causes to achieve lasting relief. Lifestyle modifications, behavioral therapies, and sometimes medications can play crucial roles in alleviating the discomfort and improving sleep quality.
Common Treatments for Sleep-Related Hallucinations
A range of treatments are available for sleep-related hallucinations, with the best approach varying depending on the individual’s specific circumstances. These treatments often focus on reducing the frequency and intensity of the hallucinations and improving the overall quality of sleep. Some treatments may involve a combination of approaches.
- Lifestyle Modifications: A healthy sleep hygiene routine is paramount. This includes establishing a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a conducive sleep environment. Regular exercise, a balanced diet, and stress management techniques, such as meditation or deep breathing exercises, can also significantly improve sleep quality and reduce the likelihood of hallucinations. Consistent sleep schedules and predictable sleep environments are crucial for regulating the body’s natural sleep-wake cycle, thereby minimizing the occurrence of sleep-related disturbances.
- Behavioral Therapies: Cognitive behavioral therapy for insomnia (CBT-I) is frequently used to address sleep-related issues. CBT-I helps patients identify and modify negative thoughts and behaviors that contribute to sleep problems. Relaxation techniques, such as progressive muscle relaxation or guided imagery, can also be helpful in reducing anxiety and promoting relaxation before sleep. These techniques equip individuals with coping mechanisms to manage stress and anxiety, which are often linked to heightened sleep disturbances.
Sleep restriction therapy, a component of CBT-I, can also be employed to regulate sleep patterns, promoting more efficient sleep.
- Medications: In some cases, medications may be necessary to manage sleep-related hallucinations, particularly if they are severe or persistent. Selective serotonin reuptake inhibitors (SSRIs) and other antidepressants may be prescribed to address underlying anxiety or mood disorders that contribute to the hallucinations. However, medications should only be considered after other interventions have been explored. The use of medications should be guided by a healthcare professional and carefully monitored.
- Managing Underlying Medical Conditions: Addressing any underlying medical conditions is critical in managing sleep-related hallucinations. For example, if sleep apnea is identified as a contributing factor, treatment for apnea is essential. Conditions like restless legs syndrome, Parkinson’s disease, or other neurological disorders may also trigger hallucinations. Thorough medical evaluation and treatment of any concurrent medical conditions are paramount in optimizing the management of sleep-related hallucinations.
Comparing Treatment Approaches
Different treatment strategies have varying degrees of effectiveness and potential side effects. CBT-I, for example, often yields long-term improvements in sleep quality without the need for medication. Lifestyle changes, such as regular exercise and stress reduction, are often recommended as foundational elements of any treatment plan.
Effectiveness of Treatments
The effectiveness of treatments for sleep-related hallucinations is variable. The outcome depends on several factors, including the underlying cause, the individual’s response to treatment, and the consistency of the treatment plan. While some individuals may experience significant improvement with lifestyle changes and behavioral therapies, others may require medication. Monitoring and adjusting treatment strategies as needed is key to achieving optimal outcomes.
Prevention Strategies: What Causes Sleep Related Hallucinations
Sleep-related hallucinations can be a disruptive and unsettling experience, but proactive measures can significantly reduce their occurrence. Understanding the factors contributing to these hallucinations allows us to implement strategies for better sleep hygiene, stress management, and overall well-being. By cultivating a conducive sleep environment and prioritizing sleep quality, individuals can significantly minimize the risk of experiencing these episodes.Effective prevention strategies often involve addressing the underlying causes of the hallucinations.
This approach emphasizes creating a supportive environment conducive to healthy sleep and reducing potential triggers. By consistently practicing these strategies, individuals can create a positive feedback loop, enhancing their sleep quality and reducing the likelihood of sleep-related hallucinations.
Establishing Good Sleep Hygiene Practices
Maintaining a consistent sleep schedule is crucial for regulating the body’s natural sleep-wake cycle. This regularity helps synchronize the internal clock with the external environment, promoting deeper and more restorative sleep. Going to bed and waking up around the same time each day, even on weekends, is key to this process. Creating a relaxing bedtime routine can also signal to the body that it’s time to wind down.
This might involve taking a warm bath, reading a book, or practicing gentle stretching exercises.
Reducing Stress and Anxiety
Chronic stress and anxiety can significantly impact sleep quality and increase the likelihood of sleep-related hallucinations. Stress-reducing techniques, such as meditation, deep breathing exercises, or yoga, can help manage stress levels and promote relaxation before bedtime. Regular exercise, while promoting overall health, also contributes to better sleep. Finding healthy ways to cope with stress is essential for reducing the risk of sleep-related hallucinations.
Creating a Conducive Sleep Environment
A comfortable and dark sleep environment is critical for optimal sleep. Maintaining a cool, quiet, and dark bedroom can significantly improve sleep quality. Using blackout curtains or an eye mask can block out light, while white noise machines or earplugs can minimize disruptive sounds. A comfortable mattress and pillows tailored to individual needs also contribute to a more restful sleep experience.
Ensuring a quiet and dark environment will minimize potential disturbances.
Improving Sleep Quality and Quantity
Adequate sleep duration is crucial for cognitive function and overall well-being. The recommended amount of sleep varies by individual, but most adults require 7-9 hours of quality sleep per night. Prioritizing sleep and establishing a routine conducive to quality sleep will lead to more restorative sleep, reducing the risk of sleep-related hallucinations. Regular physical activity, while promoting overall health, also contributes to better sleep quality.
Conclusion
In conclusion, sleep-related hallucinations stem from a complex interplay of factors, including neurological processes, psychological states, and environmental influences. From medical conditions to sleep hygiene, substance use to stress levels, various elements contribute to the occurrence of these experiences. Ultimately, a comprehensive understanding of these causes, coupled with appropriate diagnostic measures and management strategies, is vital for improving sleep quality and overall well-being.