Papule definition of an acne papule delves into the specifics of this skin condition. Understanding what constitutes an acne papule is key to effective management and treatment. This in-depth exploration covers everything from defining the papule itself to examining its causes, symptoms, and available treatments.
Acne papules are small, solid bumps on the skin. They’re often inflamed and reddish, and their formation is intricately linked to clogged pores, bacteria, and hormonal changes. This guide will explore the characteristics of papules, their connection to other acne types, and the importance of proper skincare and medical advice for effective management.
Definition and Characteristics
Acne papules are a common skin condition characterized by inflamed, raised bumps. These lesions are typically a result of blocked hair follicles and the subsequent inflammatory response within the skin. Understanding their characteristics is crucial for proper diagnosis and treatment.Understanding the differences between various types of acne lesions is essential for effective management. Different types of acne lesions, like papules, pustules, and nodules, have unique appearances and causes, influencing the treatment approach.
Differentiating these lesions helps determine the severity and appropriate course of action.
Papule Definition
A papule is a small, solid, raised skin lesion that doesn’t contain pus. It arises from inflammation beneath the skin’s surface. The defining feature of a papule is its solid, non-pustular nature.
Key Characteristics Distinguishing Papules
Papules are distinguished from other skin lesions by their specific characteristics. These characteristics include a firm, raised texture, and a limited depth. These characteristics help differentiate them from other skin conditions. For example, they differ from flat spots or lesions filled with pus.
Typical Appearance of a Papule
Papules typically present as small, round or slightly irregular bumps. They range in size from a few millimeters to about 1 centimeter in diameter. The color of a papule can vary from pinkish-red to reddish-brown, depending on the severity of inflammation. The appearance reflects the underlying inflammatory process.
Comparing Papules with Pustules and Nodules
Papules, pustules, and nodules are all types of acne lesions, but they differ in appearance and cause. Understanding these differences aids in effective treatment. The key distinctions lie in the presence or absence of pus and the depth of the lesion.
Table: Key Differences between Papules, Pustules, and Nodules
| Characteristic | Papule | Pustule | Nodule |
|---|---|---|---|
| Appearance | Small, solid, raised bump; pinkish-red to reddish-brown | Small, pus-filled bump; white or yellow | Large, solid, deep, often painful bump; reddish-pink or purplish |
| Size | Usually a few millimeters to 1 centimeter | Usually a few millimeters to 1 centimeter | Often larger than 1 centimeter; can extend deep into the skin |
| Texture | Firm, often slightly tender | Soft, pus-filled, often tender | Firm, deep, often painful |
| Cause | Blocked hair follicles and inflammation | Blocked hair follicles, inflammation, and pus formation | Blocked hair follicles, inflammation, and deep tissue involvement |
Causes of Acne Papules

Acne papules, those pesky little bumps that often plague our skin, aren’t just a matter of bad luck. They develop due to a complex interplay of factors, and understanding these causes is key to effective management. This deeper dive will explore the critical roles of bacteria, inflammation, clogged pores, hormonal fluctuations, and sebum production in the formation of these skin imperfections.The formation of acne papules is a multifaceted process involving the interaction of several factors.
From the microscopic level of bacterial activity to the broader impact of hormonal changes, each element plays a crucial role in the development of these skin lesions. Understanding these factors is essential for developing personalized strategies to combat acne and promote healthier skin.
Role of Bacteria
Acne papules are often associated with the presence ofP. acnes*, a bacterium naturally found on the skin. When pores become clogged, this bacterium multiplies rapidly, leading to inflammation and the formation of papules. The inflammatory response triggered by the bacteria further contributes to the swelling and redness characteristic of acne. This is a critical link in the chain of events that causes acne, highlighting the importance of maintaining skin hygiene to prevent bacterial overgrowth.
So, you’re trying to understand acne papules? A papule is basically a small, raised bump on the skin. It’s often a sign of inflammation, like a pimple, but learning about these skin conditions can be a good starting point for understanding your body. Sometimes, understanding your body’s signals can help you focus on your overall health and well-being, like when you’re trying to get pregnant fast.
How to get pregnant fast can be a complex topic, and you’ll want to talk to your doctor for personalized advice. No matter what, understanding your body is key, and acne papules are just one small piece of that puzzle.
Role of Inflammation
Inflammation is a natural response to injury or infection, playing a significant role in the development of papules. When clogged pores become infected with bacteria, the immune system triggers an inflammatory response, leading to redness, swelling, and pain. This inflammatory reaction is the key to the visible characteristics of the papule, highlighting the importance of managing inflammation to reduce discomfort and prevent scarring.
Role of Clogged Pores
Clogged pores are the foundation of acne development. When dead skin cells, sebum, and bacteria accumulate in the pore, it creates a breeding ground forP. acnes*. This blockage leads to increased pressure within the follicle, contributing to inflammation and the development of papules. Effective skincare routines that focus on exfoliation and pore cleansing can help prevent clogged pores and thus reduce the risk of acne.
Influence of Hormonal Changes
Hormonal fluctuations, particularly during puberty and menstruation, significantly impact sebum production, a key factor in acne development. Increased androgen levels, for example, stimulate sebaceous glands to produce more sebum. This heightened sebum production, combined with other factors like bacterial activity and clogged pores, can lead to the formation of acne papules. Understanding these hormonal influences is crucial for tailoring acne management strategies to individual hormonal cycles.
So, you’ve got a pesky acne papule? A papule, basically, is a small, raised, inflamed bump on the skin. While figuring out your sleeping position might not directly cure your acne, it could reveal some interesting things about your personality. For example, did you know that certain sleeping positions could reflect your personality traits? Check out this fascinating article on what your sleeping position says about you to see if your nighttime posture aligns with your known characteristics.
Regardless of your sleeping style, understanding the papule definition is key to effective acne management.
Sebum Production
Sebum, an oily substance produced by sebaceous glands, is essential for skin health. However, excessive sebum production can lead to clogged pores and subsequent inflammation. When sebum production is elevated, it can mix with dead skin cells and bacteria, creating a perfect environment forP. acnes* proliferation. This process is critical in the formation of acne papules.
Maintaining a balance in sebum production is vital for preventing acne.
Potential Triggers
Various factors can trigger or exacerbate acne papules. These include:
- Stress: Stress can disrupt hormonal balance, leading to increased sebum production and a higher risk of acne development. For example, students experiencing exam stress might see a rise in acne breakouts.
- Diet: Certain foods, such as high-glycemic index carbohydrates, may influence hormone levels and sebum production, potentially increasing acne risk. A diet high in processed foods, for example, could be a trigger.
- Certain Medications: Some medications, such as corticosteroids or certain birth control pills, can affect sebum production and increase the likelihood of acne development.
- Cosmetics: Certain cosmetics, particularly those with pore-clogging ingredients, can contribute to acne development. Heavy makeup, for instance, can trap sebum and exacerbate the problem.
Symptoms and Associated Conditions
Acne papules, while often a cosmetic concern, can sometimes present with additional symptoms that extend beyond the visible lesion. Understanding these associated symptoms is crucial for proper management and recognizing potential complications. This section will delve into the broader picture of papules, exploring their relationship with other acne types and potential complications.Beyond the noticeable bump, acne papules can present with various accompanying symptoms.
These range from mild tenderness and slight swelling to more significant discomfort and inflammation. The intensity of these symptoms can fluctuate depending on the individual and the severity of the acne.
Common Symptoms Associated with Acne Papules
Acne papules, though often small, can trigger a localized inflammatory response. This leads to symptoms like redness, warmth, and tenderness to the touch. In some cases, the affected area may feel slightly swollen, and the papule may become slightly elevated. Sometimes, there’s also a slight tingling or burning sensation. The severity of these symptoms varies, and not all individuals will experience them all.
Relationship Between Papules and Other Acne Lesions
Acne papules are often closely linked to other types of acne lesions. Comedones, for example, can progress to papules if the trapped sebum and dead skin cells become inflamed. This inflammatory response is a key factor in the development of papules from comedones. The progression from comedones to papules is a common stage in acne development.
So, you’re looking for the definition of an acne papule? It’s basically a small, red, solid bump on the skin. Knowing the best time to check your blood sugar can be crucial for managing health conditions, and understanding the details of papules is important for identifying and treating skin issues. For a deeper dive into optimal blood sugar testing times, check out this helpful resource: best time to check blood sugar.
Ultimately, understanding papules is key to properly diagnosing and treating acne.
Potential Associated Conditions or Complications
While generally not life-threatening, acne papules can lead to potential complications. Scarring is a significant concern, particularly with persistent or severe inflammation. Scarring can range from mild, barely noticeable marks to deep, noticeable pits. In rare cases, acne can lead to psychological distress, impacting self-esteem and confidence.
Importance of Hygiene and Skincare Practices
Maintaining good hygiene and implementing proper skincare routines are essential for managing acne papules. Regular cleansing with a gentle, non-comedogenic cleanser helps remove excess oil and debris. Gentle exfoliation can also help prevent the accumulation of dead skin cells that can exacerbate inflammation. Avoiding harsh scrubbing, however, is crucial to prevent irritation. Choosing products specifically formulated for acne-prone skin can significantly aid in managing symptoms.
Importance of Seeking Medical Advice
Persistent or severe acne papules, particularly those that don’t respond to at-home remedies, require professional medical attention. A dermatologist can accurately diagnose the condition, recommend appropriate treatment options, and potentially identify underlying causes. Early intervention and proper treatment are key to preventing further complications, such as scarring. A dermatologist can also advise on the best skincare practices tailored to individual needs.
Diagnosis and Treatment Options: Papule Definition Of An Acne Papule
Pinpointing the cause and severity of acne papules is crucial for effective treatment. A dermatologist can accurately diagnose acne papules through a visual examination and a detailed patient history. This assessment helps determine the type and extent of the acne, enabling the development of a personalized treatment plan.Understanding the underlying factors contributing to acne papules is vital for choosing the right treatment strategy.
Factors like hormonal fluctuations, genetics, and lifestyle choices play a significant role in the development and progression of acne.
Diagnostic Process
A dermatologist meticulously examines the affected skin area, looking for characteristics like the size, shape, and distribution of papules. They will also inquire about the patient’s medical history, including any previous acne treatments, medications, and lifestyle habits. This detailed evaluation allows the dermatologist to rule out other skin conditions with similar appearances.
Common Treatment Methods, Papule definition of an acne papule
Various methods are employed to treat acne papules, ranging from topical applications to oral medications. The chosen treatment depends on the severity and extent of the acne.
Topical Treatments
Topical treatments directly target the affected skin, providing localized relief and addressing the acne at its source. These treatments often contain active ingredients like benzoyl peroxide, salicylic acid, or retinoids. Benzoyl peroxide works by killing bacteria and reducing inflammation, while salicylic acid exfoliates the skin and unclogs pores. Retinoids stimulate cell turnover, preventing future breakouts.
- Benzoyl peroxide: This common ingredient is often a first-line treatment for acne papules due to its effectiveness in reducing inflammation and killing bacteria. It can be quite effective for mild to moderate cases, but can sometimes cause skin irritation, redness, and dryness in some individuals.
- Salicylic acid: Salicylic acid is another effective topical treatment for acne. It has keratolytic properties, meaning it helps to exfoliate the skin and unclog pores. This can be particularly beneficial for those with comedonal acne (blackheads and whiteheads) that often accompany papules.
- Retinoids: Prescription retinoids, like tretinoin, are potent topical treatments that work by regulating skin cell turnover. This helps prevent future breakouts and reduces the appearance of existing acne scars. Retinoids can take several weeks to show significant results, and some individuals may experience mild skin irritation initially.
Oral Medications
Oral medications are often reserved for more severe or persistent cases of acne papules. These medications address the underlying hormonal imbalances or inflammatory processes that contribute to the condition.
- Antibiotics: Oral antibiotics, such as tetracycline or erythromycin, can help control bacterial overgrowth that plays a significant role in acne development. They are often prescribed in conjunction with topical treatments to maximize effectiveness.
- Hormonal Contraceptives: In some cases, particularly for women experiencing hormonal acne, oral contraceptives can help regulate hormone levels, reducing the frequency and severity of breakouts. This is a common treatment for hormonal imbalances and acne.
- Isotretinoin: Isotretinoin, an oral retinoid, is a powerful medication often used for severe cases of acne that don’t respond to other treatments. However, it carries significant side effects and is only prescribed by dermatologists in specific cases, due to potential serious side effects.
Effectiveness Comparison
The effectiveness of different treatment approaches varies depending on individual factors. For example, benzoyl peroxide is often effective for mild to moderate acne, while retinoids are more suitable for persistent cases. Oral antibiotics can be helpful in controlling bacterial overgrowth, while isotretinoin is reserved for the most severe cases.
Prevention Strategies
Preventing acne papules requires a multi-pronged approach targeting lifestyle factors, diet, skincare routines, and stress management. A proactive approach to these elements can significantly reduce the likelihood of breakouts and improve overall skin health. This is crucial for maintaining a clear complexion and boosting self-esteem.A holistic approach to preventing acne papules goes beyond simply treating existing breakouts. By understanding the contributing factors and implementing preventative measures, individuals can actively manage their skin health and minimize the occurrence of blemishes.
Lifestyle Changes for Acne Prevention
Maintaining a healthy lifestyle plays a vital role in controlling acne. Regular habits contribute to overall well-being, which in turn positively impacts skin health. Incorporating these changes into your routine can significantly reduce the risk of developing acne papules.
- Regular Exercise: Physical activity boosts blood circulation, which helps deliver essential nutrients to the skin cells and remove toxins. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. For instance, a brisk walk, jogging, or swimming can improve circulation and overall skin health. Exercise also helps regulate hormones, which can influence acne development.
- Adequate Sleep: Sufficient sleep allows the body to repair and regenerate cells, including skin cells. Aim for 7-9 hours of quality sleep per night to promote optimal skin health. Lack of sleep can disrupt hormone balance, contributing to acne breakouts.
- Stress Management: Chronic stress can trigger hormonal imbalances that lead to acne. Incorporating stress-reducing activities, such as meditation, yoga, or deep breathing exercises, can significantly help manage stress and reduce acne risk. Identifying and managing stress triggers is also an important component.
Dietary Recommendations for Acne Management
A balanced diet rich in fruits, vegetables, and lean proteins is essential for overall health and can contribute to clearer skin. Nutrients like vitamins, minerals, and antioxidants play a crucial role in maintaining healthy skin function. Conversely, certain foods and drinks can exacerbate acne.
- Balanced Diet: Prioritize a diet rich in fruits, vegetables, and whole grains. These foods provide essential vitamins, minerals, and antioxidants that support healthy skin function. Limit processed foods, sugary drinks, and excessive consumption of dairy products, which may trigger acne in some individuals.
- Hydration: Drinking plenty of water is crucial for overall health and supports skin hydration. Dehydration can lead to dry skin, which can contribute to acne breakouts. Ensure you drink sufficient water throughout the day.
Effective Skincare Routines for Papule Prevention
Consistent and appropriate skincare practices are crucial in maintaining healthy skin and preventing acne papules. A personalized routine adapted to your skin type is essential for preventing breakouts.
- Gentle Cleansing: Use a gentle, non-comedogenic cleanser twice daily to remove dirt, oil, and makeup. Avoid harsh scrubbing, as this can irritate the skin and worsen acne. Opt for a cleanser suitable for your skin type.
- Exfoliation: Regular, gentle exfoliation can help remove dead skin cells and prevent clogged pores. Choose a mild exfoliant, such as a chemical exfoliant, and avoid over-exfoliating, which can damage the skin barrier.
- Moisturization: Moisturizing is crucial, even for oily skin. Using a non-comedogenic moisturizer can hydrate the skin without clogging pores. This helps maintain the skin’s natural barrier.
Stress Management Techniques for Acne Reduction
Stress can significantly impact hormone levels and contribute to acne breakouts. By incorporating stress-reducing techniques, individuals can positively influence their skin health.
- Mindfulness Practices: Mindfulness techniques, such as meditation and deep breathing exercises, can help manage stress levels and reduce its impact on acne. Consistent practice can significantly lower stress and improve skin health.
- Physical Activity: Regular exercise can help alleviate stress and improve overall well-being, which can positively affect acne. Physical activity promotes relaxation and releases endorphins, further reducing stress.
- Adequate Sleep: Sufficient sleep is crucial for the body’s ability to manage stress and maintain overall health, which also positively impacts acne. A consistent sleep schedule is essential for stress reduction and improved skin health.
Illustrations and Visual Aids
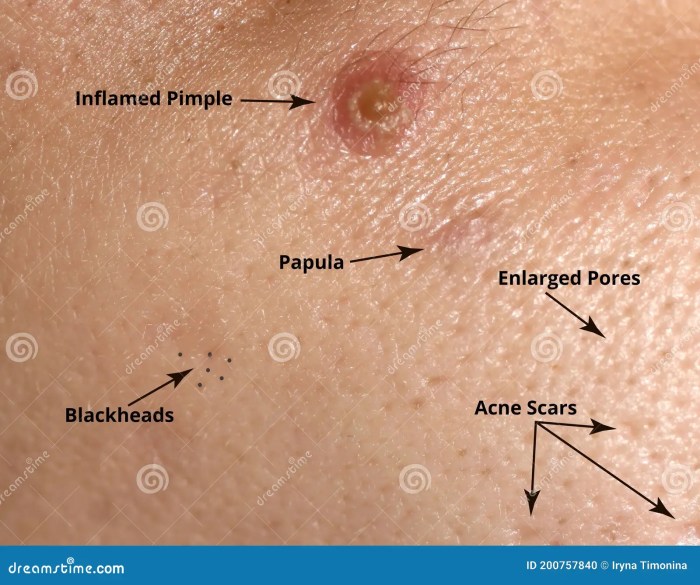
Visual aids are crucial for understanding complex concepts like acne papules. Illustrations and diagrams help visualize the characteristics, development, and relationship of papules to other acne lesions and skin structures. This section provides detailed descriptions of various visual representations that can aid in comprehension.
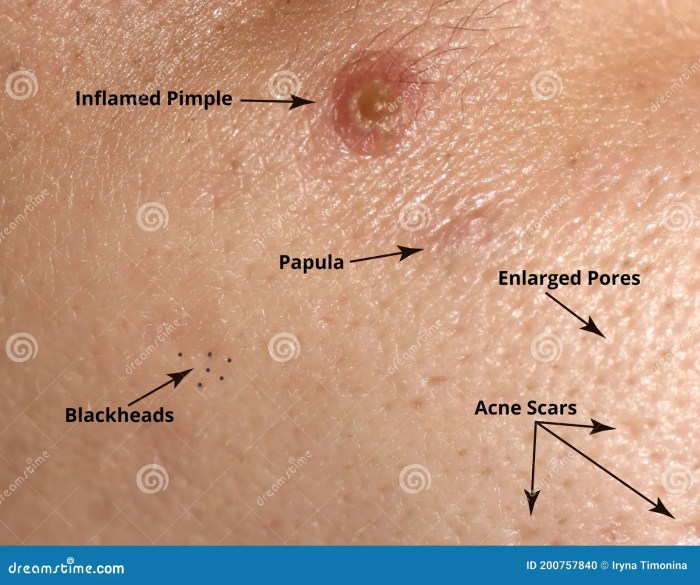
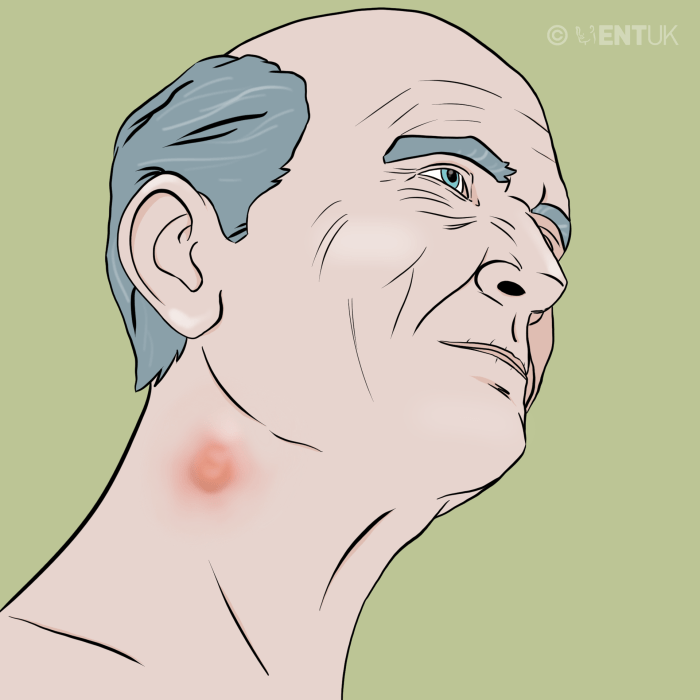
Papule Visual Representation
A papule is a small, solid, raised skin lesion. A visual representation would depict a slightly elevated area on the skin, typically round or oval, with a well-defined border. Its color might vary, from skin-toned to reddish or pinkish, depending on the inflammation level. The size would typically be less than 1 centimeter in diameter. The illustration should clearly distinguish the papule from surrounding skin.
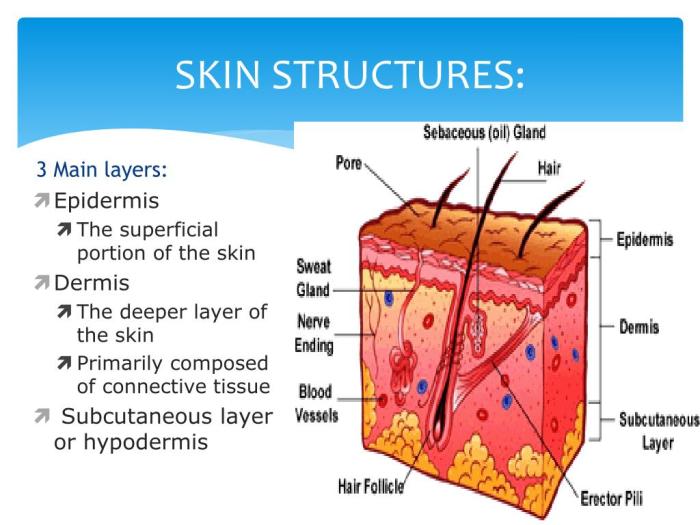
Diagram of a Typical Papule Anatomy
A diagram illustrating a typical papule’s anatomy should show a cross-section of the skin. The diagram should highlight the key elements: the epidermis, dermis, and the papule itself. The papule should be depicted as an elevated area within the dermis, potentially indicating inflammation or a buildup of material. The diagram should clearly show the boundary between the papule and the surrounding skin.
It would also potentially illustrate the inflammatory cells that might be present in the dermis around the papule.
Comparison of Acne Lesions
A visual aid comparing and contrasting different acne lesions, including papules, should use a table format. This table would categorize various acne lesions (e.g., papules, pustules, nodules, cysts) and illustrate them using simple shapes. Each lesion would be clearly labeled. Important characteristics, such as size, color, and texture, would be noted for each lesion type. For example, a papule would be shown as a small, solid elevation, while a pustule would be a similar elevation containing pus.
This visual aid would help differentiate between different types of acne lesions.
| Lesion Type | Description | Appearance |
|---|---|---|
| Papule | Small, solid elevation | Small, round or oval, slightly raised area, skin-colored to reddish |
| Pustule | Papule containing pus | Small, pus-filled elevation, white or yellow |
| Nodule | Deep, solid lesion | Larger, firm, and painful, often inflamed |
| Cyst | Deep, pus-filled lesion | Larger, inflamed, painful, pus-filled, and often tender |
Cross-section of a Skin Pore with a Papule
A labeled illustration of a cross-section of a skin pore with a papule should clearly show the pore structure. The pore should be shown as a canal in the epidermis and dermis. A papule should be shown as an accumulation of material, possibly sebum, within or adjacent to the pore, leading to inflammation and swelling. The illustration should highlight the relationship between the pore, the papule, and the surrounding skin tissue.
Labels should indicate the epidermis, dermis, hair follicle, sebaceous gland, and the location of the papule.
Stages of Acne Papule Development
A graphic representation of the stages of acne papule development would use a series of sequential images. The first image could depict a normal skin pore. Subsequent images would show the buildup of sebum and/or bacteria, progressing to inflammation and finally to the formation of a papule. This visual aid should clearly illustrate the progression of events, highlighting the contributing factors at each stage.
It would effectively show how a simple buildup can lead to an acne papule.
Final Review
In conclusion, understanding acne papules, from their definition to their management, empowers individuals to take control of their skin health. This comprehensive guide provides a thorough understanding of this common skin condition. By recognizing the causes, symptoms, and treatment options, individuals can proactively address acne papules and work towards clearer, healthier skin.