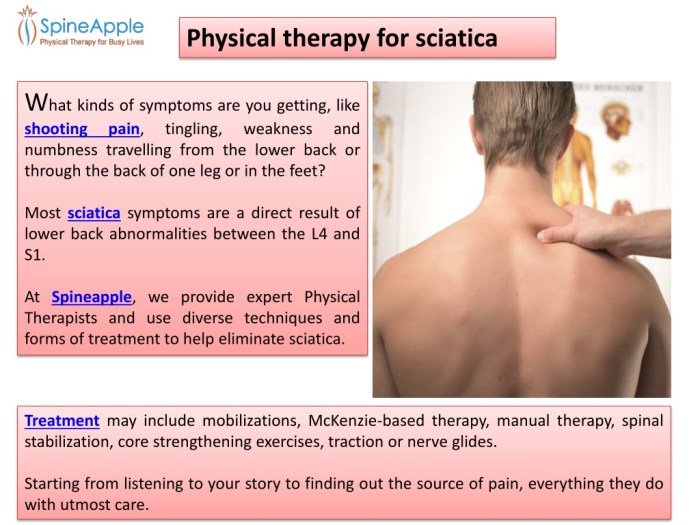
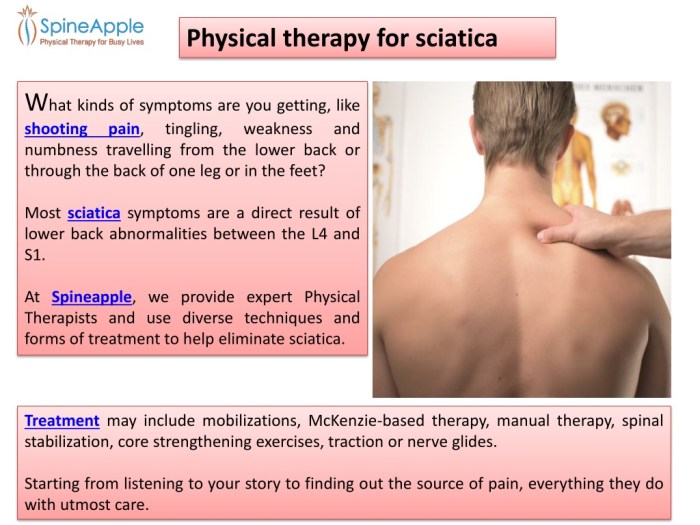
Physical therapy for sciatica offers a powerful approach to managing and relieving this debilitating condition. It delves into understanding the root causes, identifying effective treatments, and empowering patients with self-management strategies. This guide will explore the various techniques and exercises used in physical therapy to alleviate sciatica pain, improve posture, and enhance overall well-being.
This comprehensive guide explores the multifaceted nature of sciatica, providing a detailed overview of its causes, symptoms, and effective physical therapy approaches. We will delve into the role of assessments, personalized treatment plans, and crucial home exercises to help you navigate this condition effectively.
Introduction to Sciatica
Sciatica is a common condition characterized by pain that radiates along the sciatic nerve, which runs from the lower back down each leg. It’s often described as a sharp, burning, or shooting pain, but the specific sensation can vary. Understanding the causes, symptoms, and types of sciatica pain is crucial for effective diagnosis and treatment.The sciatic nerve is the largest nerve in the body, originating from the lower back and extending down through the buttocks and legs.
Irritation or compression of this nerve can lead to a range of symptoms, often affecting daily activities. Common causes include herniated discs, spinal stenosis, piriformis syndrome, and other musculoskeletal issues. Identifying the specific cause helps guide appropriate treatment strategies.
Common Causes of Sciatica
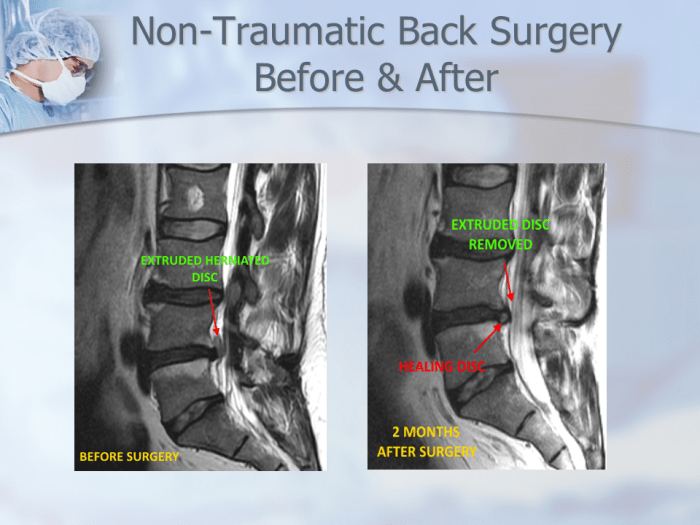
Various factors can contribute to sciatica. A herniated disc, where the soft inner material of a spinal disc bulges out, can press on the sciatic nerve. Spinal stenosis, a narrowing of the spinal canal, can also compress the nerve. Muscle imbalances, such as those associated with piriformis syndrome (where the piriformis muscle irritates the sciatic nerve), can contribute to the condition.
Other contributing factors include osteoarthritis, pregnancy, and rarely, tumors.
Typical Symptoms of Sciatica
Sciatica pain is typically characterized by a sharp, shooting, or burning sensation radiating down one leg. The pain can range in intensity from mild discomfort to severe agony. It often worsens with certain movements, such as bending, twisting, or sitting for extended periods. Other symptoms may include numbness, tingling, or weakness in the affected leg. The pain may also be accompanied by muscle spasms or stiffness in the lower back.
Physical therapy for sciatica can be a game-changer, helping you manage pain and regain movement. Sometimes, dealing with sciatica pain can lead to feeling disconnected or spaced out, almost like you’re not fully present. Understanding what exactly “spacing out” entails can be helpful in pinpointing the underlying causes and finding effective coping mechanisms. For a deeper dive into the concept of “spacing out,” check out this article: what is spacing out.
Ultimately, physical therapy provides targeted exercises and techniques to alleviate sciatica symptoms, helping you feel grounded and back in control.
Types of Sciatica Pain
| Type of Pain | Description | Example |
|---|---|---|
| Sharp Pain | A sudden, intense, stabbing sensation. | Imagine a sudden, intense poke with a needle. |
| Burning Pain | A continuous, uncomfortable, fiery sensation. | A feeling like a hot object is touching the affected area. |
| Shooting Pain | A quick, intense, and often localized pain that travels along the nerve path. | Imagine an electric shock that travels down the leg. |
This table illustrates the different sensations associated with sciatica pain. Each individual’s experience can vary significantly, and the type of pain may also depend on the underlying cause of the condition.
Physical Therapy Approaches for Sciatica
Physical therapy plays a crucial role in managing sciatica pain and restoring function. A tailored physical therapy program can help alleviate pain, improve mobility, and prevent future episodes. It often involves a combination of exercises, manual therapies, and education.Physical therapists employ various techniques to address the root cause of sciatica and its associated symptoms. These techniques aim to reduce inflammation, improve flexibility, strengthen core muscles, and correct postural imbalances.
A personalized approach is essential for optimal results, considering individual needs and limitations.
Common Physical Therapy Techniques for Sciatica
Various physical therapy techniques are employed to address the underlying causes of sciatica and alleviate symptoms. These include manual therapy, such as spinal manipulation and mobilization, to address restrictions in spinal movement. Soft tissue mobilization, like massage and myofascial release, targets tight muscles and improves tissue flexibility. Exercise therapy is fundamental, focusing on strengthening core muscles and improving flexibility of the surrounding muscles.
Patient education plays a vital role in empowering individuals to manage their condition effectively and prevent future episodes.
Exercises for Sciatica Pain Relief
Specific exercises are designed to strengthen the core muscles, improve flexibility, and reduce pain. These exercises are tailored to individual needs and abilities.
- Core Strengthening Exercises: Exercises like planks, bridges, and pelvic tilts strengthen the abdominal and back muscles, providing support to the spine and reducing pressure on the sciatic nerve. Modifications for individuals with limited mobility or strength include starting with shorter holds and progressively increasing duration and difficulty. For instance, a beginner could perform a modified plank by resting their forearms on the floor, instead of their hands.
- Stretching Exercises: Stretching the hamstrings, hip flexors, and piriformis muscles can alleviate tightness that can contribute to sciatica pain. Gentle, sustained stretches are crucial, avoiding any sudden or forceful movements. An example of a hamstring stretch involves lying on the back with one leg extended and the other bent, gently pulling on the extended leg to feel the stretch.
Modifications for individuals with reduced flexibility include starting with shorter stretches and gradually increasing the duration and intensity.
- Strengthening Exercises: Strengthening exercises for the glutes and surrounding muscles help support the lower back and improve posture. Examples include glute bridges, hip abductions, and clam shells. Modifications for beginners might involve using resistance bands or lighter weights, and gradually increasing the resistance and repetitions.
Improving Posture and Core Strength
Maintaining good posture and a strong core are essential for preventing sciatica. Proper posture reduces stress on the spine and surrounding structures, while a strong core provides support and stability.
- Postural Awareness: Practicing mindful posture throughout the day, whether sitting, standing, or walking, is vital. Individuals should focus on keeping their spine straight, shoulders relaxed, and core engaged. This includes sitting with good back support and avoiding slouching.
- Core Engagement Exercises: Incorporating core engagement exercises into daily routines can significantly enhance spinal support. Examples include engaging the core muscles while performing everyday activities like lifting objects and standing up from a chair.
Physical Therapy Modalities
Various physical therapy modalities are used to manage sciatica symptoms. These modalities aim to reduce inflammation, improve blood flow, and alleviate pain.
- Heat Therapy: Heat therapy can help relax muscles and increase blood flow to the affected area, potentially reducing pain and stiffness. Hot packs, heating pads, or warm baths are common methods.
- Ice Therapy: Ice therapy is effective in reducing inflammation and swelling, which can alleviate pain in the acute phase of sciatica. Ice packs or cold compresses are typically used.
- Ultrasound Therapy: Ultrasound therapy uses high-frequency sound waves to increase blood flow and reduce pain. It can also help promote tissue healing.
Exercises for Sciatica
This table provides a structured overview of exercises for sciatica, including descriptions and illustrations of proper form.
| Exercise | Description | Illustration |
|---|---|---|
| Pelvic Tilt | Lie on your back with knees bent, feet flat on the floor. Tighten your abdominal muscles and gently tilt your pelvis upward. Hold for a few seconds, then release. | (Imagine a picture showing the correct posture, with the pelvis tilted slightly upward, while the rest of the body remains relaxed.) |
| Glute Bridge | Lie on your back with knees bent and feet flat on the floor, hip-width apart. Lift your hips off the floor, squeezing your glutes at the top. Lower back down slowly. | (Imagine a picture showing the correct posture, with the hips lifted off the floor, and the spine in a straight line.) |
| Standing Hamstring Stretch | Stand with one leg slightly behind the other. Bend forward at the hips, keeping your back straight. Reach toward your toes. | (Imagine a picture showing the correct posture, with the back straight and the reach towards the toes.) |
Assessment and Diagnosis
Physical therapists play a crucial role in evaluating sciatica, moving beyond simply treating symptoms to pinpoint the underlying cause. Accurate assessment is essential for developing a personalized treatment plan and ensuring optimal recovery. A thorough evaluation helps distinguish sciatica from other potential back pain conditions, leading to more effective interventions.Physical therapists employ a multifaceted approach to assess sciatica, combining a patient’s medical history with a physical examination.
This detailed evaluation not only identifies the source of the pain but also determines the patient’s functional limitations and potential contributing factors.
Physical Therapist Evaluation Process
The physical therapist’s evaluation process for sciatica typically begins with a detailed history taking session. This involves questioning the patient about the onset, location, duration, and intensity of the pain, as well as any associated symptoms like numbness, tingling, or weakness. The therapist also inquires about the patient’s lifestyle, occupation, and any prior injuries or medical conditions. This crucial initial step provides valuable insight into the patient’s individual circumstances.
Following this, a physical examination is conducted.
Physical Examination
A comprehensive physical examination for sciatica is crucial. It includes checking posture, range of motion, muscle strength, and reflexes in the affected area. The therapist assesses spinal mobility, looking for any limitations or restrictions. Neurological testing, such as checking reflexes and sensation in the legs, is also performed to identify potential nerve involvement. Specific tests, like the straight leg raise test, are used to evaluate the sciatic nerve.
This hands-on assessment allows the physical therapist to identify the affected areas and the nature of the issue.
Diagnostic Tools
Several diagnostic tools are commonly employed by physical therapists to aid in the assessment of sciatica. These tools may include:
- Visual Observation: Observing the patient’s posture and gait can reveal clues about potential causes of the pain.
- Palpation: Feeling for tenderness, muscle spasms, or other abnormalities in the spine and surrounding tissues helps identify areas of concern.
- Range of Motion (ROM) Tests: Measuring the extent of movement in the spine and extremities assists in determining limitations and restrictions that might be contributing to the pain.
- Neurological Tests: These tests evaluate reflexes, sensation, and muscle strength in the legs and feet to pinpoint nerve involvement. The straight leg raise test, for instance, helps assess sciatic nerve irritation.
- Special Tests: Specific tests, like the Slump test, are utilized to evaluate nerve impingement.
Diagnostic Tests for Sciatica vs. Other Back Pain Conditions
| Diagnostic Test | Sciatica | Other Back Pain Conditions |
|---|---|---|
| Straight Leg Raise Test | Positive test (pain radiating down the leg) suggests sciatic nerve involvement. | May be positive, but pain may not radiate, or could be related to other musculoskeletal issues. |
| Slump Test | Positive test (pain radiating down the leg) suggests nerve root impingement. | May produce pain, but not necessarily indicative of nerve root involvement. |
| Neurological Examination | Assessment of reflexes, sensation, and strength in the lower extremities to identify nerve root compression. | Focus on assessing the spine, muscles, and joints for other musculoskeletal issues. |
| Imaging (X-rays, MRI) | May be recommended to rule out structural abnormalities or disc herniations contributing to the sciatica. | Essential for identifying fractures, tumors, or other serious conditions. |
Patient Education and Management
Empowering sciatica patients with knowledge and practical strategies is crucial for effective management. Beyond physical therapy interventions, understanding the condition and adopting self-management techniques are key to long-term recovery and pain reduction. This section delves into the importance of patient education, strategies for self-management, lifestyle modifications, and the creation of personalized treatment plans.
Importance of Patient Education
Patient education is fundamental to successful sciatica management. Educated patients are better equipped to understand their condition, actively participate in their care, and make informed decisions about their treatment. This knowledge empowers them to manage their symptoms effectively and prevent future recurrences. It fosters a collaborative relationship between the patient and the physical therapist, ultimately leading to improved outcomes.
Strategies for Patient Education on Self-Management Techniques
Effective patient education involves providing clear and concise information about sciatica, its causes, and its potential triggers. This includes explaining the rationale behind specific exercises and stretches, and demonstrating correct posture and body mechanics. Active participation is key; patients should be encouraged to actively practice the techniques learned in therapy sessions and to understand the importance of consistency in their self-management approach.
Physical therapy for sciatica is often a great way to manage pain and improve mobility. However, sometimes those nagging nighttime leg cramps and feelings of being trapped in bed could be linked to sleep paralysis, a condition where you’re conscious but unable to move. Understanding the causes of sleep paralysis, like those explored in this helpful resource on what causes sleep paralysis , can help you better address the underlying issues and improve your sleep quality, which in turn can impact the effectiveness of your physical therapy for sciatica.
A patient-centered approach, where the patient’s individual needs and preferences are considered, is crucial for successful self-management strategies.
Lifestyle Modifications for Sciatica Management
Lifestyle modifications play a significant role in managing sciatica. Addressing potential risk factors such as poor posture, prolonged sitting, and insufficient physical activity can significantly impact pain levels. Recommendations for ergonomic adjustments in the workplace and at home, incorporating regular physical activity tailored to individual capabilities, and maintaining a healthy weight can contribute to pain relief and prevent future flare-ups.
Furthermore, stress management techniques can be beneficial in managing pain and improving overall well-being.
Examples of Patient Education Materials
Patient education materials should be clear, concise, and visually appealing. These materials can include brochures, pamphlets, videos, and online resources. Brochures could Artikel common causes of sciatica, potential triggers, and self-management strategies. Videos could demonstrate proper posture, stretching techniques, and exercises. Online resources could provide interactive quizzes, symptom trackers, and links to reputable health information.
Consider using illustrations and diagrams to enhance understanding and engagement.
Creating a Personalized Treatment Plan
Developing a personalized treatment plan is essential for optimal sciatica management. This involves assessing the patient’s specific needs, medical history, and lifestyle factors. The plan should integrate physical therapy exercises, lifestyle modifications, and patient education components. Regular follow-up appointments are critical for monitoring progress, adjusting the plan as needed, and addressing any concerns or challenges. For instance, a patient with a sedentary job might benefit from ergonomic recommendations and regular stretching breaks, whereas a patient with a physically demanding job might require specific exercises to strengthen core muscles and improve posture.
The personalized approach ensures that the plan is tailored to the individual’s circumstances, maximizing its effectiveness.
Specific Treatment Considerations: Physical Therapy For Sciatica

Sciatica, characterized by pain radiating down the leg, often requires a multifaceted approach beyond basic pain management. Effective treatment considers the underlying causes, including nerve impingement, muscle imbalances, and inflammation, and integrates various therapeutic modalities. This section delves into specific treatment approaches, highlighting the role of manual therapy, taping techniques, and strategies for addressing contributing factors.
Manual Therapy in Sciatica
Manual therapy plays a crucial role in addressing sciatica by restoring proper biomechanics and reducing nerve compression. Techniques focus on improving joint mobility, releasing muscle tension, and restoring normal spinal function. These techniques are often integrated with other therapies like exercise and education.
Manual Mobilization Techniques for Sciatica Pain
Manual mobilization techniques are used to address restrictions in spinal and/or hip joints that may contribute to sciatica pain. These techniques include spinal manipulations, mobilizations, and soft tissue massage. Specific techniques, like spinal adjustments, can address spinal segmental restrictions, while soft tissue techniques can address trigger points and muscle spasms that often accompany sciatica. Properly performed, these techniques can improve joint mechanics and reduce pain.
Examples include: spinal glides, articulation techniques, and muscle energy techniques.
Taping Techniques for Sciatica
Taping techniques provide support and reduce pain and inflammation associated with sciatica. These techniques can aid in maintaining proper posture, stabilizing joints, and supporting weakened muscles. Neurodynamic mobilization taping techniques, for example, can help reduce nerve tension. Proper taping techniques, applied by trained professionals, can provide temporary support, allowing the patient to perform daily activities with reduced pain and improved function.
Examples of Manual Therapy Techniques for Sciatica
| Technique | Description | Effectiveness |
|---|---|---|
| Spinal Manipulation (e.g., HVLA) | High-velocity, low-amplitude thrusts to restore joint mobility. | Can provide short-term pain relief, but effectiveness varies depending on the patient and the specific condition. |
| Spinal Mobilization (e.g., sustained mobilization) | Gentle, controlled movements to improve joint mobility. | Often effective for reducing pain and improving range of motion. |
| Myofascial Release | Soft tissue techniques to release muscle tension and adhesions. | Can help alleviate muscle pain and improve soft tissue extensibility. |
| Muscle Energy Techniques | Utilizing the patient’s own muscle contractions to restore joint mobility. | Effective in addressing muscle imbalances and improving joint function. |
Addressing Pain, Inflammation, and Muscle Imbalances
Addressing pain, inflammation, and muscle imbalances is crucial for managing sciatica effectively. Pain management strategies include medication (as prescribed by a physician), heat/ice therapy, and transcutaneous electrical nerve stimulation (TENS). Inflammation reduction can be addressed through anti-inflammatory medications and physical modalities. Addressing muscle imbalances involves targeted strengthening and stretching exercises, aimed at restoring proper muscle function and reducing strain on the affected nerves.
Examples of muscle imbalances could include tightness in the hamstrings or gluteal muscles, leading to compensatory movements and further pain. Proper assessment and targeted interventions are essential.
Home Exercises and Self-Care
Taking proactive steps at home is crucial for managing sciatica effectively. Consistent home exercises and self-care strategies can significantly reduce pain, improve flexibility, and enhance overall well-being. By incorporating these practices into your daily routine, you can actively participate in your recovery and prevent future flare-ups.
Effective Home Exercises for Sciatica
Home exercises play a vital role in managing sciatica pain and restoring function. These exercises, when performed correctly and consistently, can strengthen core muscles, improve flexibility, and reduce pressure on the sciatic nerve. Regular practice helps maintain proper posture, which is essential in preventing further irritation.
- Gentle Walking: Start with short, slow walks, gradually increasing duration and pace as tolerated. Walking helps improve circulation, strengthens leg muscles, and reduces stiffness.
- Pelvic Tilts: Lie on your back with knees bent and feet flat on the floor. Gently tilt your pelvis upward, engaging your abdominal muscles. Hold for a few seconds and release. Repeat several times. This exercise strengthens core muscles, supporting the lower back and reducing pressure on the sciatic nerve.
- Knee-to-Chest Stretches: Lie on your back with knees bent. Gently pull one knee towards your chest, holding for a few seconds. Repeat with the other knee. This stretch targets the hip flexors and hamstrings, relieving tension and improving flexibility.
- Hamstring Stretches: Sit on the floor with one leg extended straight in front of you. Gently reach for your toes, keeping your back straight. Hold for a few seconds and repeat with the other leg. Stretching the hamstrings helps maintain flexibility and reduce tension in the lower back, which can contribute to sciatica pain.
Importance of Warm-up and Cool-down Routines
Proper warm-up and cool-down routines are essential components of any exercise program, including those for sciatica. Warming up prepares the muscles for activity, reducing the risk of injury, and increasing blood flow to the area. Cool-down helps the body gradually return to a resting state, reducing muscle soreness and stiffness.
- Warm-up: Begin with 5-10 minutes of light cardio, such as brisk walking or arm circles, to increase blood flow to the muscles. Dynamic stretches, like leg swings and torso twists, further prepare the body for more strenuous exercises. This preparation reduces the chance of injury and enhances the effectiveness of the exercise routine.
- Cool-down: After completing the exercises, engage in 5-10 minutes of static stretches, holding each stretch for 15-30 seconds. This helps muscles recover and prevents stiffness. Examples include hamstring stretches, quad stretches, and lower back stretches. This crucial step aids in recovery and reduces the risk of muscle soreness.
Specific Stretches and Exercises
This table Artikels specific stretches and exercises, categorized by body part, to address common sciatica pain points. Regularly performing these exercises can improve flexibility, strength, and overall well-being.
| Body Part | Stretch/Exercise | Description |
|---|---|---|
| Lower Back | Cat-Cow Pose | On all fours, alternate between arching and rounding your back. This improves spinal mobility and flexibility. |
| Hips | Pigeon Pose | A seated stretch targeting hip flexors and glutes. This helps relieve tension and improve flexibility in the hips, which are often affected by sciatica. |
| Hamstrings | Standing Hamstring Stretch | Stand with one leg extended behind you, slightly bent, and gently lean forward, keeping your back straight. This targets the hamstring muscles, crucial for lower back support. |
| Glutes | Glute Bridges | Lie on your back with knees bent and feet flat on the floor. Lift your hips off the floor, squeezing your glutes. This strengthens the glutes, a vital muscle group for spinal support. |
Demonstrating a Safe and Effective Home Exercise Program
A safe and effective home exercise program for sciatica involves gradual progression and listening to your body. Start with a manageable routine, gradually increasing the duration and intensity of exercises as tolerated. If any exercise causes increased pain, stop immediately and consult your healthcare provider.
Consistency is key for successful outcomes. Regular practice of the exercises will bring about significant improvements in managing sciatica.
Tips for Preventing Sciatica Flare-ups
Preventing sciatica flare-ups involves maintaining good posture, staying active, and addressing underlying causes.
- Maintain Good Posture: Pay attention to your posture while sitting, standing, and lifting objects. Good posture reduces strain on the lower back.
- Stay Active: Regular physical activity, including walking, swimming, or yoga, can help maintain flexibility and strength. This helps prevent stiffness and muscle imbalances that can contribute to flare-ups.
- Address Underlying Causes: If possible, identify and address any underlying conditions that may contribute to sciatica, such as poor posture, obesity, or repetitive strain injuries.
Long-Term Management and Prevention
Sciatica, while often treatable, requires a proactive approach for long-term well-being. Understanding the factors contributing to its recurrence is crucial for preventing future episodes and improving overall quality of life. This proactive strategy focuses on lifestyle modifications and preventative measures.Effective long-term management involves a multifaceted strategy that goes beyond just treating the immediate pain. It’s about building resilience and preventing the condition from returning by addressing the underlying contributing factors.
Physical therapy for sciatica can be incredibly helpful, targeting the root cause of your pain. A great way to build strength and stability in your core, which often plays a significant role in sciatica relief, is through exercises like the one-legged balance challenge for backache. This challenge, detailed in a helpful guide on Valley Ridge Health’s website one legged balance challenge for backache , can significantly improve your overall posture and core strength.
Incorporating these types of exercises into a physical therapy program can be a game-changer in managing sciatica.
This proactive approach includes regular exercise, proper body mechanics, maintaining a healthy weight, and making informed dietary choices.
Importance of Regular Exercise and Physical Activity
Regular physical activity plays a significant role in maintaining spinal health and preventing sciatica. Exercise strengthens core muscles, which support the spine and reduce stress on the sciatic nerve. A balanced exercise routine that incorporates both aerobic and strengthening exercises is vital. This helps maintain flexibility, promotes healthy blood circulation, and reduces the risk of muscle imbalances. For example, swimming, walking, or cycling can improve cardiovascular health and overall body conditioning, reducing the risk of sciatica.
Role of Proper Body Mechanics
Proper body mechanics are essential for preventing sciatica. Maintaining good posture during daily activities, including lifting, sitting, and standing, is critical. Lifting heavy objects with proper form, avoiding prolonged periods of sitting without breaks, and using ergonomic furniture are all crucial steps in preventing strain on the lower back. Practicing correct posture, especially when lifting, is key to avoiding strain on the spine.
Significance of Maintaining a Healthy Weight and Diet
Maintaining a healthy weight significantly reduces the strain on the spine. Excess weight puts added pressure on the lower back, increasing the risk of sciatica. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for maintaining bone health and muscle strength. A healthy diet, coupled with regular exercise, contributes to a healthy weight and reduces the risk of inflammation.
For instance, individuals who maintain a healthy weight are less likely to experience sciatica recurrences.
Examples of Lifestyle Changes to Help Prevent Sciatica Recurrence
Lifestyle changes are pivotal in preventing sciatica recurrence. These changes can include regular exercise routines, proper posture and body mechanics during daily activities, maintaining a healthy weight, and consuming a balanced diet. Quitting smoking, managing stress, and ensuring sufficient sleep are also important components of long-term management. For instance, incorporating regular stretching and yoga into the daily routine can improve flexibility and reduce the risk of future episodes.
Additionally, a structured sleep routine, coupled with a healthy diet, will help in maintaining overall health and reducing inflammation, a factor linked to sciatica.
Illustrations and Visual Aids
Understanding sciatica often requires visualizing the affected structures. Detailed illustrations and diagrams can greatly enhance comprehension, making complex anatomical relationships more accessible. Visual aids allow patients to connect abstract concepts with their own bodies, fostering a deeper understanding of their condition and its potential solutions.
Spine Anatomy and Sciatica, Physical therapy for sciatica
The spine is a complex structure composed of vertebrae, intervertebral discs, and various ligaments and muscles. Proper visualization of these components is crucial for understanding sciatica. The vertebrae stack to form the spinal column, providing support and protection for the spinal cord. Intervertebral discs act as shock absorbers, enabling flexibility and movement. Ligaments stabilize the spine, while muscles provide support and control movement.
Misalignments, injuries, or degeneration in these structures can put pressure on the spinal nerves, leading to sciatica pain. A diagram showing the different parts of the spine and their interrelationship would be extremely helpful. Illustrate the potential for disc herniation, spinal stenosis, or facet joint issues to cause nerve impingement.
Sciatic Nerve Anatomy
The sciatic nerve is the largest nerve in the human body, originating from the lower back and extending down the buttock and leg. Visualizing its course through the pelvis, buttocks, and leg is essential. The sciatic nerve is composed of multiple smaller nerves that branch out to various muscle groups and sensory areas. An illustration showing the sciatic nerve’s path from its origin in the spine to its branching points in the lower limb, clearly highlighting potential points of impingement (such as piriformis syndrome or spinal stenosis), would greatly assist in understanding how pressure on this nerve can cause sciatica.
Illustrate how different structures like the piriformis muscle, the sacroiliac joint, or the sciatic notch can contribute to compression.
Spinal Postures and Sciatica
Different spinal postures can impact the likelihood of experiencing sciatica pain. A table comparing and contrasting various postures, such as forward flexion, prolonged sitting, and excessive lumbar lordosis, is useful. The table should correlate each posture with potential mechanical stress on the spine and sciatic nerve. For example, prolonged sitting often leads to lumbar flexion, which can compress the nerve roots.
Illustrate each posture and its effect on the spine and surrounding structures.
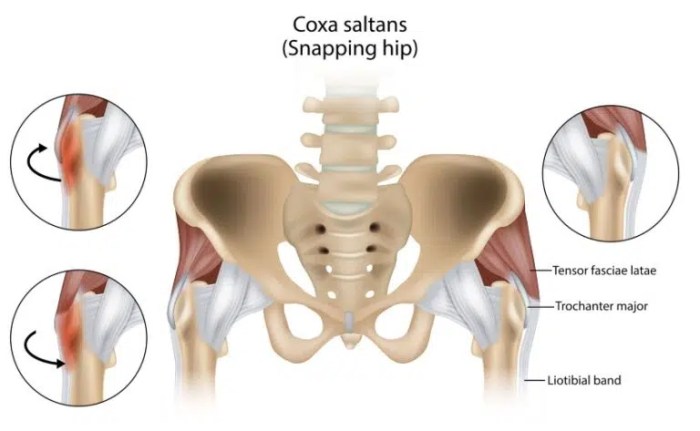
Muscle Imbalances and Sciatica
Muscle imbalances around the spine and hips can contribute to sciatica. Visual aids, such as anatomical diagrams, are helpful in identifying these imbalances. Muscle imbalances can cause altered biomechanics, leading to increased stress on the spine and sciatic nerve. For instance, tight hip flexors can pull on the pelvis, altering spinal alignment and potentially compressing the sciatic nerve.
Illustrations showing the relevant muscles, including the piriformis, gluteus maximus, and hamstrings, and their potential imbalances, should be included. Examples of how imbalances can affect posture and lead to pain would enhance understanding.
Last Recap
In conclusion, physical therapy for sciatica is a valuable resource for managing this common condition. By understanding the causes, symptoms, and treatment options, you can take an active role in your recovery and long-term well-being. This guide provides a comprehensive overview, equipping you with the knowledge and tools to effectively manage sciatica through physical therapy. Remember, consistency and a proactive approach are key to successful outcomes.