Surgery for tennis elbow is a significant decision, and this guide provides a comprehensive overview of the procedure. It explores the causes and symptoms of tennis elbow, differentiating between types and highlighting the typical patient profile. We’ll also dispel common misconceptions and compare surgical options to conservative treatments. Understanding the pre- and post-operative care, recovery process, and potential complications is crucial for informed decision-making.
This in-depth look at tennis elbow surgery covers surgical techniques, recovery timelines, alternative treatments, success rates, costs, and patient experiences. It’s designed to equip you with the knowledge necessary to navigate this potentially complex medical journey.
Introduction to Tennis Elbow Surgery: Surgery For Tennis Elbow

Tennis elbow, also known as lateral epicondylitis, is a common overuse injury affecting the tendons on the outside of the elbow. It’s characterized by pain and tenderness in this area, often aggravated by activities that involve gripping, twisting, or extending the wrist. This pain can range from mild discomfort to severe limitations in daily activities.Understanding the specific type of tennis elbow is crucial for determining the most appropriate treatment approach, including surgical intervention.
Various factors, including the duration and intensity of symptoms, and the patient’s overall health, influence the decision-making process.
Causes of Tennis Elbow
Tennis elbow arises from repetitive strain on the tendons that attach the forearm muscles to the outside of the elbow. This strain can be caused by various activities, including but not limited to: playing tennis (though not exclusively), using tools, gardening, and certain types of computer work. Overuse and improper technique are often cited as key contributing factors.
Types of Tennis Elbow
The condition is not always uniform. There are variations in the nature and severity of the injury. Differentiating these types is crucial for appropriate treatment. The distinction between types often lies in the extent of tendon damage. Some individuals might experience mild inflammation, while others may have significant tendon tears.
The varying degrees of tendon damage will affect the suitability of surgical intervention.
Patient Profile for Tennis Elbow Surgery
Surgical intervention for tennis elbow is typically considered for patients who have not responded to conservative treatments, such as physical therapy, rest, and pain medication. These individuals often experience significant pain and functional limitations that impair their daily activities. The patient profile typically includes individuals who have tried various non-surgical methods without substantial improvement. In addition, patients with severe or chronic tendon damage are more likely to be surgical candidates.
Common Misconceptions About Tennis Elbow Surgery
A common misconception is that tennis elbow surgery is a quick fix for everyone. In reality, recovery time can vary significantly, and successful outcomes depend on factors beyond the surgical procedure itself, such as patient compliance with rehabilitation and lifestyle adjustments. Another misconception is that all cases of tennis elbow will necessitate surgery. Conservative treatments often effectively manage the condition.
Finally, some believe that tennis elbow surgery is always successful. While surgery can be beneficial, it’s not guaranteed to eliminate pain entirely in every case.
Conservative vs. Surgical Treatments, Surgery for tennis elbow
| Characteristic | Conservative Treatment | Surgical Treatment | Description |
|---|---|---|---|
| Initial Treatment Approach | Non-invasive, typically first-line treatment | Reserved for cases that don’t respond to conservative measures | Conservative methods are often attempted before surgery. |
| Treatment Duration | Can take several weeks to months | Recovery can take several months | Recovery times vary depending on the individual. |
| Success Rate | High success rate for many individuals | High success rate for appropriate cases | Both treatments can yield positive results in appropriate situations. |
| Potential Risks | Minimal risks | Potential risks, including infection and nerve damage | Surgical interventions carry risks that conservative methods generally avoid. |
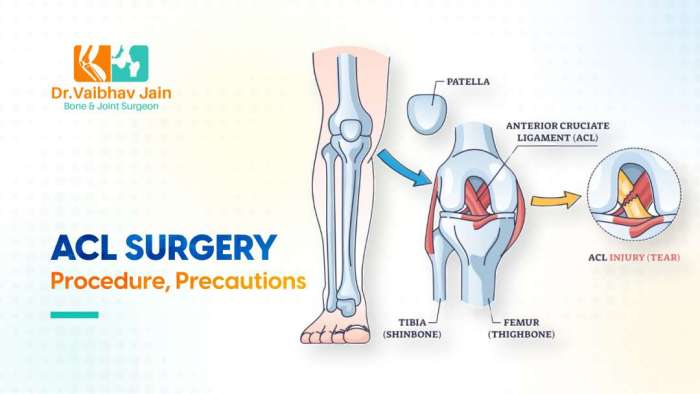
Surgical Procedures for Tennis Elbow

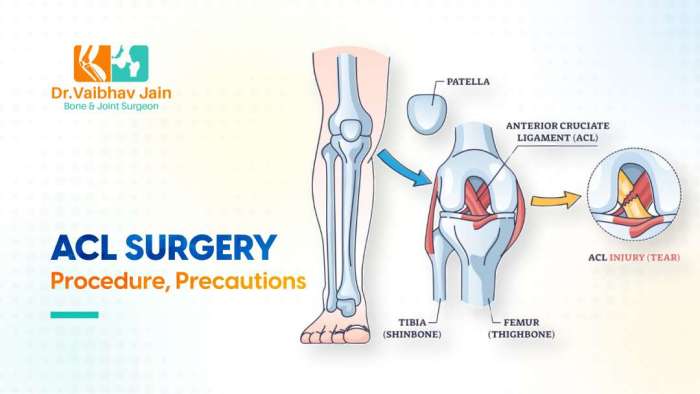
Surgical intervention for tennis elbow, also known as lateral epicondylitis, is often considered when conservative treatments fail to alleviate pain and restore function. Various surgical techniques exist, each with its own advantages and disadvantages. Choosing the right procedure depends on factors like the severity of the condition, the patient’s overall health, and the surgeon’s expertise.Different surgical approaches target the inflamed or damaged tissues around the lateral epicondyle, aiming to reduce pain, improve mobility, and restore normal function.
The specific procedure chosen will influence the recovery process and potential outcomes. This section will explore the common surgical techniques used for tennis elbow repair, their detailed steps, instruments, and comparative effectiveness.
Surgical Techniques for Tennis Elbow Repair
Different surgical approaches are available for tennis elbow, each with its own characteristics. These techniques address the underlying cause of the condition, aiming for optimal results. Surgical techniques generally involve either releasing the tight tissues around the lateral epicondyle or repairing the damaged tendons.
Open Release Surgery
This procedure involves a small incision over the affected area. The surgeon exposes the tendons and surrounding tissues, identifying and releasing any tight or inflamed structures. This allows for better visualization and direct access to the affected region. This procedure is often performed under general anesthesia.The surgical steps typically involve:
- Making a small incision over the lateral epicondyle of the humerus.
- Identifying the extensor tendons and the surrounding tissues.
- Using surgical instruments to release any constricting bands or inflamed tissue around the tendons.
- Examining the tendons for any tears or damage.
- Closing the incision with sutures and dressings.
Surgical instruments used in open release surgery include scalpels, surgical scissors, retractors, and needle holders. Sutures and absorbable materials are employed for closing the incision.
Arthroscopic Surgery
This minimally invasive technique uses small incisions and specialized instruments, known as arthroscopes, to visualize and treat the affected area. Arthroscopy offers several benefits, including smaller scars, reduced pain, and a quicker recovery time compared to open surgery. The surgeon inserts the arthroscope through small incisions, allowing for visualization of the tendon and surrounding tissues.The procedure involves:
- Creating small incisions around the affected area.
- Inserting the arthroscope to visualize the tendons and surrounding tissues.
- Using small instruments to release any constricting tissues or repair any tears.
- Checking for any other issues within the joint.
- Closing the incisions with sutures.
Surgical instruments include arthroscopes, small surgical instruments (e.g., shavers, scissors), and specialized anchors or sutures.
Comparison of Surgical Techniques
| Surgical Technique | Pros | Cons | Recovery Time |
|---|---|---|---|
| Open Release | Direct visualization and access to the affected area, good for complex cases. | Larger incision, potentially more scarring, longer recovery period. | 6-8 weeks |
| Arthroscopic | Minimally invasive, smaller incisions, quicker recovery time, less scarring. | Limited visualization in complex cases, potential for instrument-related complications. | 4-6 weeks |
The effectiveness and recovery times of both techniques vary. Open release surgery is often considered more effective for complex cases, while arthroscopic surgery is preferred for simpler cases due to its less invasive nature. Patient-specific factors should be considered to determine the most appropriate surgical approach.
Pre-Operative and Post-Operative Care
Navigating the path to recovery after tennis elbow surgery involves careful pre-operative planning and meticulous post-operative management. Understanding the steps involved, from initial assessments to long-term rehabilitation, empowers patients to actively participate in their journey toward healing and regaining function. This section delves into the critical aspects of pre- and post-operative care, providing insights into the process and expected outcomes.
Pre-Operative Assessments and Evaluations
Thorough pre-operative evaluations are crucial for ensuring the surgery’s success and minimizing potential risks. These evaluations typically include a comprehensive physical examination, focusing on the affected wrist and elbow joint. Diagnostic imaging, such as X-rays or MRIs, may be used to assess the extent of the injury and rule out other conditions. Neurological assessments are also performed to ensure there are no nerve impingements or complications that could be exacerbated by the surgery.
These assessments allow the surgeon to tailor the surgical approach and anticipate potential challenges.
Pre-Operative Instructions
Prior to surgery, patients are provided with detailed instructions encompassing dietary restrictions and medication adjustments. A period of fasting before the surgical procedure is typically required to minimize the risk of complications during anesthesia. Specific dietary guidelines are often Artikeld, with clear instructions on what to avoid consuming before the scheduled surgery. Patients are also instructed on any medications they should discontinue or adjust in the days leading up to the procedure.
This pre-operative preparation aims to optimize patient well-being and reduce surgical risks.
Post-Operative Recovery Process
The post-operative recovery period typically involves a gradual return to normal activities. Pain management is crucial, and patients are provided with pain medications to manage discomfort. The level of pain experienced can vary among individuals, but most patients report a decrease in pain over time as the tissues heal. Early mobilization exercises, often prescribed by physical therapists, are vital for regaining range of motion and strength.
The duration of recovery can differ, depending on the individual’s response to treatment and the severity of the injury.
Common Post-Operative Complications
Potential complications, though infrequent, may arise following tennis elbow surgery. These complications can include infection, nerve damage, or persistent pain. Proper post-operative care, diligent adherence to prescribed treatments, and prompt reporting of any concerning symptoms to the surgeon are essential to minimize the risk of these complications. Patients should be aware of the possibility of complications and know how to contact their healthcare provider if needed.
Potential Risks Associated with Tennis Elbow Surgery
Like any surgical procedure, tennis elbow surgery carries potential risks. These risks include bleeding, infection, and adverse reactions to anesthesia. The possibility of persistent pain, stiffness, or a failure to regain full function also exists. Understanding these potential risks is vital for patients to make informed decisions about their care.
Summary of Pre-operative, Intra-operative, and Post-operative Care
| Category | Description | Example | Importance |
|---|---|---|---|
| Pre-operative | Comprehensive evaluation (physical exam, imaging, etc.), dietary restrictions, medication adjustments | Fasting before surgery, discontinuing blood-thinning medications | Minimizes risks and ensures optimal surgical conditions |
| Intra-operative | Surgical procedure itself, precise repair techniques | Surgical repair of the tendon, use of anchors | Correct diagnosis and successful repair |
| Post-operative | Pain management, physical therapy, gradual return to activity | Follow-up appointments, adherence to rehabilitation program | Facilitates healing and restoration of function |
Recovery and Rehabilitation
Post-operative recovery from tennis elbow surgery is a journey, not a sprint. A well-structured rehabilitation plan is crucial for a successful outcome. This phase involves carefully guided exercises and physical therapy to regain strength, flexibility, and function in the affected arm. It’s vital to understand that individual recovery timelines and needs vary significantly, and strict adherence to the prescribed plan is key to achieving optimal results.
Dealing with surgery for tennis elbow can be tough, but understanding other foot issues can actually help. For example, sometimes the pain radiating from the elbow can be connected to issues like a bunionette or tailor’s bunion, a bony bump on the pinky toe joint. Learning more about this condition could offer a new perspective on managing your elbow pain, which often gets overlooked in discussions about foot problems.
Check out this article for more information: what is a bunionette or tailors bunion on the foot. Ultimately, a thorough understanding of potential causes is key when it comes to effective surgery for tennis elbow.
Typical Recovery Timeline
The recovery timeline for tennis elbow surgery typically ranges from several weeks to several months. Early stages focus on pain management and gentle movement. As healing progresses, the intensity and complexity of exercises increase. Patients can expect gradual improvements in range of motion, strength, and overall function. For instance, a patient might start with simple wrist flexion and extension exercises and progress to more complex movements like gripping and lifting over a period of weeks or months, depending on the individual’s response and the surgical procedure performed.
Post-Operative Exercises and Physical Therapy
Physical therapy plays a pivotal role in the recovery process. A qualified therapist will design a personalized exercise program tailored to the individual’s needs. This program often includes a combination of stretching, strengthening, and range-of-motion exercises. Exercises might include wrist curls, extensions, and rotations, along with exercises focusing on the forearm and shoulder muscles to maintain overall upper body strength.
It’s important to follow the instructions provided by the therapist precisely and avoid pushing the limits too soon, which can lead to complications.
Importance of Adherence to the Rehabilitation Plan
Adherence to the rehabilitation plan is paramount for a successful recovery. Skipping exercises or pushing beyond the prescribed limits can impede healing and increase the risk of re-injury. A dedicated approach to each exercise is essential for proper muscle activation and tissue repair. A patient who consistently follows the plan is more likely to experience a faster and more complete recovery, preventing potential setbacks.
Factors Influencing the Speed of Recovery
Several factors can influence the speed of recovery, including the severity of the initial condition, the surgical technique employed, the patient’s age and overall health, and their commitment to the rehabilitation program. Individuals with pre-existing conditions or those who have a more sedentary lifestyle might experience a slightly slower recovery process. Moreover, the patient’s motivation and ability to adhere to the prescribed exercises significantly affect the recovery timeline.
Exercises for Different Stages of Recovery
A structured approach to exercises is vital throughout the recovery process. Different stages require different types of exercises. This is crucial to ensure progressive overload, allowing muscles to adapt and regain strength gradually.
- Early Stage (Weeks 1-4): Focus on gentle range of motion exercises to prevent stiffness and promote healing. These exercises might include wrist circles, finger extensions, and light hand squeezes. Examples include performing gentle wrist flexion and extension movements, and making fist-and-open hand gestures for a few minutes several times a day.
- Intermediate Stage (Weeks 5-8): As pain subsides and range of motion improves, the exercises become more challenging. Exercises include strengthening exercises targeting the forearm and hand muscles, like wrist curls and extensions with light weights, and exercises to improve grip strength, such as squeezing stress balls or putty. Examples might involve using progressively heavier weights for wrist curls, and increasing the repetitions of hand squeezes.
- Advanced Stage (Weeks 9-12+): The focus shifts to restoring full strength and function. Exercises include more complex movements, like lifting light weights, resistance band exercises, and activities that mimic daily tasks. Examples include progressively lifting weights and incorporating activities that use the wrist and hand, like playing musical instruments or working on a computer.
Alternatives to Surgery
Tennis elbow, a painful condition affecting the tendons in the elbow, often responds well to non-surgical treatments. Surgical intervention is typically reserved for cases where conservative methods fail to provide relief. Understanding the alternatives to surgery is crucial for making informed decisions about your treatment path.Conservative treatments for tennis elbow, like rest, ice, and physical therapy, often represent a more conservative approach to managing the condition.
Surgery for tennis elbow can be a serious consideration, but it’s important to understand the whole picture. A crucial part of any surgical procedure, like this one, involves the dedicated work of the scrub tech, whose vital role is often overlooked. Learning more about what scrub techs do, like prepping the surgical field and handling instruments, can give you a better understanding of the intricate process involved.
scrub tech what they do Ultimately, understanding the roles of everyone involved, from the scrub tech to the surgeon, makes the whole process of surgery for tennis elbow clearer.
These methods focus on reducing inflammation, strengthening supporting muscles, and improving range of motion without the need for invasive procedures. The effectiveness of these methods can vary depending on the individual’s condition and adherence to treatment plans.
Conservative Treatment Options
Conservative treatments are often the first line of defense against tennis elbow pain. They aim to address the underlying causes of the condition, reduce inflammation, and improve the overall function of the elbow joint. These methods typically involve a combination of approaches, tailored to the specific needs of each patient.
- Rest: Avoiding activities that exacerbate pain is crucial in the early stages of treatment. This allows the affected tendons to heal and recover from the stress and strain. This often involves modifying activities that place stress on the forearm and wrist, such as certain types of gripping, lifting, or twisting motions. For example, a carpenter might need to temporarily alter their woodworking tasks or a tennis player might need to reduce their practice sessions to allow their elbow to rest.
- Ice: Applying ice packs to the affected area can help reduce inflammation and pain. Regular application of ice, for example, 15-20 minutes at a time, several times a day, can help manage discomfort. This helps to constrict blood vessels, reducing swelling and promoting healing.
- Physical Therapy: A physical therapist can develop a customized exercise program to strengthen the muscles that support the elbow and forearm. This often involves targeted exercises to improve flexibility, reduce pain, and restore function. For example, exercises like wrist extensions, forearm curls, and stretches can help improve strength and flexibility in the affected area. This can be especially beneficial in the long term, preventing future episodes of tennis elbow.
Effectiveness of Conservative Treatments
The effectiveness of conservative treatments varies greatly from person to person. While many individuals experience significant pain reduction and functional improvement with these methods, some cases may require more aggressive interventions. The time required for noticeable improvement can range from a few weeks to several months. The crucial element is consistency in treatment and adherence to the prescribed plan.
Comparison with Surgical Interventions
Surgical intervention for tennis elbow is a more aggressive approach, reserved for cases where conservative treatments fail to provide adequate relief. The effectiveness of surgery can vary, with potential for long-term benefits but also risks and complications. The decision to pursue surgery should be made in consultation with a medical professional, weighing the potential benefits against the risks and considering the individual’s specific circumstances.
Situations Where Surgery Might Not Be Necessary
In many instances, conservative treatments can effectively address tennis elbow pain. Surgery is not always the best option. Factors like the severity of the condition, the patient’s overall health, and the patient’s willingness to commit to a conservative treatment plan can influence this decision. Individuals who have a strong preference for non-invasive approaches and are willing to engage in a rigorous and sustained program of conservative treatment may find that surgery is unnecessary.
Long-Term Benefits and Drawbacks of Each Approach
Conservative treatments, while potentially less invasive, can sometimes require a significant time commitment for noticeable results. The potential drawbacks might include the need for patience and adherence to a prescribed treatment plan. On the other hand, surgical intervention, while potentially faster, carries risks of complications, including infection, nerve damage, or persistent pain.
Conservative Treatment Comparison Table
| Treatment Method | Typical Duration | Effectiveness (General) | Potential Drawbacks |
|---|---|---|---|
| Rest | Variable (weeks to months) | Reduces pain and inflammation, crucial initial step | Potential for inactivity-related muscle weakness if not coupled with other treatments |
| Ice | Ongoing as needed | Reduces inflammation and pain, can be a key part of initial treatment | Limited effect on underlying cause if not combined with other treatments |
| Physical Therapy | Variable (weeks to months) | Improves strength, flexibility, and range of motion | Requires patient commitment, may not be effective for all cases |
Success Rates and Outcomes
Tennis elbow surgery, while often effective, isn’t a guaranteed cure. Understanding the success rates, potential for complications, and factors influencing outcomes is crucial for patients considering this procedure. This section delves into the statistical data surrounding surgical success, highlighting the importance of patient compliance and factors that contribute to a positive long-term result.
Success Rates of Different Surgical Procedures
Success rates for tennis elbow surgery vary depending on the specific surgical technique employed. Different procedures target different aspects of the condition, leading to varying levels of effectiveness. Data from various studies provides insight into the efficacy of different approaches.
| Surgical Procedure | Success Rate (Approximate Range) | Factors Influencing Success | Potential for Recurrence |
|---|---|---|---|
| Open Release Surgery | 60-80% | Patient factors, surgical technique, and post-operative care | 10-20% |
| Arthroscopic Release Surgery | 70-90% | Patient factors, surgical technique, and post-operative care | 5-15% |
| PRP (Platelet-Rich Plasma) Injection | 40-60% | Patient factors, individual response to PRP | High |
Factors Influencing Long-Term Outcomes
The long-term success of tennis elbow surgery is influenced by a complex interplay of factors. These include the severity of the initial condition, the patient’s overall health, and their adherence to post-operative rehabilitation instructions.
- Patient Compliance: Adherence to prescribed physical therapy exercises, pain management strategies, and activity restrictions significantly impacts the recovery process. Patients who diligently follow their prescribed regimen are more likely to experience a positive outcome.
- Surgical Technique: The skill and experience of the surgeon play a crucial role. A well-executed procedure minimizes the risk of complications and maximizes the chances of a successful recovery.
- Underlying Conditions: Pre-existing medical conditions can affect the healing process and influence the surgical outcome. Chronic conditions or factors like poor blood circulation can increase the likelihood of complications and negatively affect healing.
- Severity of the Condition: The duration and severity of tennis elbow symptoms influence the potential for success. Patients with milder symptoms tend to experience better outcomes compared to those with more severe cases.
Potential for Recurrence
While many patients experience lasting relief after surgery, a potential for recurrence exists. Factors such as inadequate treatment of the underlying cause, improper post-operative care, or a return to strenuous activity too soon can contribute to a relapse.
- Repetitive Stress: Returning to activities that exacerbate the condition, like tennis or similar repetitive movements, can increase the risk of recurrence. Proper guidance and modifications to activities are vital.
- Incomplete Healing: Failure to address all contributing factors to the condition can lead to a recurrence of the problem.
- Poor Patient Compliance: As mentioned before, inadequate adherence to post-operative instructions significantly increases the risk of recurrence.
Factors Contributing to a Successful Outcome
A successful outcome hinges on a combination of factors. Choosing a qualified surgeon, following post-operative instructions diligently, and adopting a proactive approach to rehabilitation all contribute to a positive result.
- Prompt Diagnosis and Treatment: Early diagnosis and intervention can help prevent the condition from worsening and increase the chances of a successful outcome.
- Comprehensive Rehabilitation Program: A well-structured rehabilitation program focusing on strengthening surrounding muscles, improving flexibility, and gradually increasing activity levels is essential.
- Lifestyle Modifications: Adopting strategies to reduce repetitive stress on the affected area can prevent future problems. This might include adjusting work or recreational activities to minimize stress on the elbow.
Cost and Insurance Coverage
Understanding the financial aspects of tennis elbow surgery is crucial for patients. This section details the average costs involved, how insurance typically handles these procedures, and what to expect in terms of potential out-of-pocket expenses. Knowing the financial implications beforehand can help patients make informed decisions about their treatment plan.Navigating the healthcare system can be complex, especially when facing a surgical procedure.
This section aims to demystify the process of covering tennis elbow surgery costs, offering clarity on insurance coverage, pre-authorization requirements, and potential out-of-pocket expenses.
Average Costs
The cost of tennis elbow surgery varies considerably based on factors like the surgeon’s fees, hospital location, and the complexity of the procedure. Hospital fees encompass operating room charges, anesthesia costs, and post-operative care. Surgeon fees depend on their experience, specialty, and the specific surgical technique employed. Post-operative care costs may include physical therapy sessions, medication, and follow-up appointments.
While precise figures cannot be universally stated, a range of costs, including a general estimate, are provided for patients to consider.
Insurance Coverage
Most health insurance policies cover a portion of tennis elbow surgery costs. However, the extent of coverage varies significantly depending on the specific plan and its benefits. A crucial step is to review your policy’s specifics to understand the extent of your coverage.
Examples of Insurance Plans and Coverage
| Insurance Plan Type | Typical Coverage | Potential Out-of-Pocket Expenses |
|---|---|---|
| High-deductible health plan | May cover a substantial portion of the surgery, but patients may have a significant deductible to meet before coverage begins. | Patients may be responsible for a substantial amount of out-of-pocket expenses. |
| PPO (Preferred Provider Organization) | Usually covers a higher percentage of the cost if the surgeon is in the network. | Out-of-network surgeons may result in higher out-of-pocket expenses. |
| HMO (Health Maintenance Organization) | Often has a network of in-network providers. | Out-of-network providers may not be covered, or coverage may be limited. |
Potential Out-of-Pocket Expenses
Out-of-pocket expenses can include deductibles, co-pays, co-insurance, and any charges exceeding the plan’s coverage. Understanding these components is essential for realistic financial planning.
Pre-authorization Process
“Pre-authorization is a process where your insurance company reviews the necessity and appropriateness of a medical procedure.”
Many insurance companies require pre-authorization for tennis elbow surgery. The process typically involves submitting a request to the insurance company, providing necessary medical records, and obtaining approval before the procedure can be performed. The exact documentation requirements and timelines may differ between insurance plans, so it is crucial to contact your insurer directly for clarification.
Patient Testimonials and Experiences
Navigating the path to tennis elbow surgery can be a complex journey, filled with anticipation, anxiety, and a range of emotions. Understanding the experiences of others can provide valuable insight and support during this process. This section explores the diverse spectrum of patient experiences, highlighting both positive and negative outcomes, and emphasizing the importance of communication and emotional well-being throughout the recovery process.Patient experiences with tennis elbow surgery are varied, reflecting the individual nature of the condition and the surgical procedures themselves.
Some patients report significant relief and improved quality of life following surgery, while others face challenges during recovery. These accounts provide a more complete picture of the reality of undergoing this procedure, emphasizing the importance of realistic expectations and open communication with medical professionals.
Positive Experiences
Patients often express relief from chronic pain and discomfort after surgery. Improved mobility and function are frequently reported, allowing patients to resume activities they enjoyed before the condition developed. The ability to return to sports or daily tasks without pain is a common theme among positive testimonials. Many patients highlight the professionalism and care they received from their surgical team, contributing to a positive experience.
Negative Experiences
Some patients experience unexpected complications during or after surgery, leading to prolonged recovery periods or ongoing discomfort. Difficulties with pain management, complications from anesthesia, or unforeseen physical challenges can contribute to negative experiences. Furthermore, some patients report feelings of frustration or disappointment if their recovery does not progress as anticipated.
Dealing with tennis elbow can be tricky, and sometimes surgery is the best option. While it’s a relatively common procedure, it’s important to consider the overall health picture. For example, understanding the challenges faced by families dealing with muscular dystrophy in children, like the muscular dystrophy in children diagnosis, can provide a broader perspective on the recovery process.
Ultimately, surgery for tennis elbow, like any procedure, requires careful consideration of the patient’s specific needs and circumstances.
Common Feelings and Emotions
Patients undergoing tennis elbow surgery often experience a spectrum of emotions. Anxiety about the procedure, uncertainty about the outcome, and apprehension about the recovery process are common. Patients may also experience relief once the surgery is completed, followed by varying degrees of pain, discomfort, and emotional responses to their changing physical condition. Fear of long-term complications, including potential limitations in activities, is also a potential concern.
Acceptance and patience are vital in managing these emotional responses.
Importance of Patient Communication
Open communication between patients and their surgical team is crucial for a successful outcome. Patients should actively participate in discussions about their condition, treatment options, and recovery plans. Asking questions, expressing concerns, and seeking clarification about any uncertainties can significantly impact the overall experience. A clear understanding of expectations and realistic timelines for recovery is essential.
Emotional Support During Recovery
The emotional well-being of patients undergoing tennis elbow surgery is just as important as their physical recovery. Support from family, friends, or support groups can play a vital role in providing encouragement and reducing stress during the rehabilitation process. Recognizing the emotional toll of the surgery and the recovery period is essential for successful outcomes.
Summary of Patient Experiences
| Category | Description | Positive Experiences | Negative Experiences |
|---|---|---|---|
| Pain Management | Effectiveness of pain management strategies. | Effective pain control leading to rapid recovery. | Challenges with pain management leading to prolonged discomfort. |
| Recovery Time | Duration of the recovery process. | Faster-than-expected recovery and return to normal activities. | Slower-than-expected recovery and difficulties with rehabilitation. |
| Emotional Impact | Emotional responses to the surgery. | Strong support systems and positive outlook during recovery. | Anxiety, fear, and frustration during the recovery process. |
| Surgical Team Interaction | Patient’s perception of the surgical team. | Positive interactions and clear communication with the surgical team. | Communication issues or difficulties with the surgical team. |
Potential Complications and Risks
While tennis elbow surgery is generally safe and effective, like any surgical procedure, it carries potential complications. Understanding these risks is crucial for informed decision-making. Patients should discuss these potential issues with their surgeon to ensure a comprehensive understanding of the procedure and the possibility of encountering complications.Surgical interventions, even those deemed minor, introduce the possibility of unforeseen outcomes.
A thorough evaluation of potential complications and an open dialogue with the surgeon are essential for patients to make well-informed decisions.
Types of Potential Complications
Potential complications can range from minor discomfort to more serious issues. The body’s response to surgery and individual patient factors play a significant role in the likelihood and severity of these complications. The potential complications are categorized below.
Surgical Site Infections
Surgical site infections (SSIs) are a possible consequence of any invasive procedure. Risk factors include compromised immune systems, the presence of existing infections, and poor surgical technique. Prompt diagnosis and treatment with antibiotics are crucial in managing SSIs. Surgical site infections, if not addressed promptly, can lead to significant discomfort and even necessitate further procedures to resolve the infection.
Nerve Damage
Nerve damage, although rare, is a possible risk associated with surgery near nerves. The proximity of the ulnar nerve and other structures in the elbow region increases the possibility of accidental injury during surgery. Careful surgical technique, meticulous dissection, and the use of nerve-monitoring devices during surgery are implemented to minimize this risk. The severity of nerve damage can vary, and appropriate treatment strategies, which may include physical therapy or, in extreme cases, surgical intervention, are employed to manage the resulting issues.
Stiffness or Limited Range of Motion
Post-operative stiffness or limited range of motion is a relatively common, but often temporary, complication. This can be attributed to swelling, scar tissue formation, or pain management techniques. Physical therapy, including exercises to maintain joint mobility, plays a crucial role in restoring normal function. Patient compliance with the rehabilitation program is critical in mitigating this complication.
Bleeding or Hematoma Formation
Bleeding or hematoma formation is another potential concern. Risk factors may include pre-existing blood clotting disorders or certain medications. Careful surgical technique, meticulous hemostasis (stopping bleeding), and compression dressings help minimize this risk. In cases of significant bleeding, additional procedures may be required. Patients with known bleeding disorders may require pre-emptive interventions.
Numbness or Tingling
Numbness or tingling, often temporary, may occur in the affected area due to nerve irritation. The location and duration of these sensations can vary, and they typically resolve with time as the body heals. Patients should promptly report any persistent or worsening numbness to their surgeon.
Table of Potential Complications
| Potential Complication | Likelihood | Treatment Options | Examples of Rare/Serious Complications |
|---|---|---|---|
| Surgical Site Infection | Moderate | Antibiotics, wound care, possible surgical debridement | Sepsis (rare but serious) |
| Nerve Damage | Low | Physical therapy, nerve repair surgery (if needed) | Complete nerve paralysis (extremely rare) |
| Stiffness/Limited ROM | Moderate | Physical therapy, exercises | Permanent loss of function (uncommon) |
| Bleeding/Hematoma | Low | Compression, additional surgical intervention (if needed) | Massive hemorrhage requiring blood transfusion (extremely rare) |
| Numbness/Tingling | Low | Observation, pain management | Chronic nerve pain (uncommon) |
Final Review
In conclusion, surgery for tennis elbow is a significant choice that requires careful consideration. While it can offer relief for persistent pain, it’s crucial to understand the various surgical options, potential risks, and recovery process. Weighing the pros and cons, along with exploring alternative treatments, empowers you to make the best decision for your specific needs. Remember to discuss your options with your healthcare provider for personalized guidance.