Understanding your PSA results is crucial for prostate health. This comprehensive guide delves into what a PSA test is, how results are interpreted, and the factors that can influence them. We’ll cover everything from normal ranges and potential causes of elevated PSA to the relationship between PSA levels and prostate cancer risk, as well as next steps after receiving your results.
From simple explanations to detailed interpretations, we aim to make understanding your PSA results accessible and empowering. We’ll use visual aids and case studies to further clarify the process and provide actionable insights.
Understanding PSA Test Results – General Overview
The Prostate Specific Antigen (PSA) test is a common blood test used to screen for prostate cancer. It measures the level of PSA, a protein produced by the prostate gland. While a high PSA level doesn’t definitively mean cancer, it can indicate the need for further investigation. Understanding the results requires a careful consideration of various factors, including age and potential contributing conditions.A crucial aspect of interpreting PSA results involves understanding that PSA levels can fluctuate naturally, influenced by factors like recent ejaculation, or certain medical conditions.
This variability necessitates a nuanced approach to evaluating the significance of any given PSA reading. A detailed analysis considering the individual’s medical history and other relevant factors is essential for accurate interpretation.
What is a Prostate Specific Antigen (PSA) Test?
The PSA test measures the amount of Prostate Specific Antigen (PSA) in a man’s blood. PSA is a protein produced by the prostate gland. It’s often used as a screening tool for prostate cancer, though it’s important to remember that an elevated PSA level doesn’t automatically indicate cancer. Other factors, such as benign prostatic hyperplasia (BPH), can also contribute to higher PSA levels.
Figuring out your PSA results can feel a bit daunting, but understanding the numbers is key. It’s important to discuss these results with your doctor, and, while we’re on the topic of health, did you know about the nasal flu vaccine? Learning about options like what is the nasal flu vaccine flumist can help you make informed decisions about your health.
Ultimately, a thorough understanding of your PSA results, and your health in general, is crucial for good health management.
Why is the PSA Test Performed?
The PSA test is a screening tool used to detect potential prostate problems, primarily prostate cancer. It helps identify men who might need further evaluation and potentially more specialized diagnostic procedures. Early detection of prostate cancer can significantly improve treatment outcomes. However, it’s crucial to recognize that PSA screening isn’t perfect, and false positives can occur.
Interpreting PSA Levels, Understanding your psa results
PSA levels are measured in nanograms per milliliter (ng/mL). The interpretation of PSA levels is not straightforward and needs to be considered within the context of the individual’s age, medical history, and lifestyle.
- Age-Related Variations: PSA levels naturally increase with age. Younger men generally have lower PSA levels, while older men may have higher levels. A PSA level that might be considered elevated in a younger man might fall within the normal range for an older man. This highlights the importance of age-specific reference ranges when evaluating PSA results.
- Elevated PSA Levels: An elevated PSA level may signal the presence of prostate cancer, but other conditions, such as benign prostatic hyperplasia (BPH), can also cause elevated PSA levels. The interpretation requires additional clinical information, including digital rectal examination (DRE) findings, medical history, and family history.
- Normal PSA Ranges: The normal range for PSA levels varies significantly based on a man’s age. The following table provides a general guideline, but it’s crucial to consult with a healthcare professional for an accurate assessment of individual results.
| Age Group | Normal PSA Range (ng/mL) |
|---|---|
| 40-49 | 0.0-2.5 |
| 50-59 | 0.0-3.5 |
| 60-69 | 0.0-4.5 |
| 70+ | 0.0-6.5 |
Typical Steps in Assessing PSA Results
The following flow chart Artikels the typical steps involved in assessing PSA results. This is a general guideline, and specific procedures may vary based on individual circumstances.
This flow chart demonstrates a logical approach to evaluating PSA test results, beginning with the initial PSA measurement and progressing through additional assessments to reach a definitive diagnosis or to rule out concerning conditions. Early intervention and ongoing monitoring are key components of effective prostate health management.
Factors Affecting PSA Levels
Understanding your PSA results is crucial for your health, but it’s important to realize that various factors can influence PSA levels, making interpretation complex. A simple blood test might show elevated levels, but it doesn’t automatically mean you have prostate cancer. This section delves into the factors beyond prostate cancer that can affect PSA readings.Elevated PSA levels can stem from a multitude of causes other than prostate cancer.
These factors can be influenced by lifestyle choices, underlying medical conditions, and even recent medical procedures. Accurate diagnosis relies on a comprehensive evaluation considering these diverse influences.
Causes of Elevated PSA Levels (Beyond Prostate Cancer)
Several medical conditions and factors can lead to elevated PSA levels, clouding the interpretation of a PSA test result. It’s crucial to understand these possibilities to ensure accurate diagnosis and treatment.
- Benign Prostatic Hyperplasia (BPH): An enlargement of the prostate gland, a common condition in older men, can increase PSA levels. This non-cancerous enlargement often leads to urinary issues. For example, a man in his 60s experiencing frequent urination might have elevated PSA levels due to BPH.
- Prostatitis: Inflammation of the prostate gland, often caused by bacterial infection or other irritants, can also elevate PSA levels. Symptoms might include pain in the pelvic region, difficulty urinating, and fever. In a case where a man presents with urinary pain, the elevated PSA could be due to prostatitis, not cancer.
- Recent Prostate Procedures: Procedures like prostate biopsies or surgery can temporarily increase PSA levels due to tissue trauma. The elevated PSA in this case is a direct result of the procedure and is temporary.
- Certain Medications: Some medications, such as some types of alpha-blockers or certain anti-inflammatory drugs, can affect PSA levels. This is a known side effect that doctors should consider during diagnosis.
Medical Conditions Affecting PSA Results
A wide range of medical conditions can influence PSA levels. These conditions, when present, need to be taken into account when interpreting PSA results.
- Urinary Tract Infections (UTIs): Infections in the urinary tract can cause inflammation, potentially affecting PSA levels. For example, a man experiencing urinary symptoms alongside a fever might have an elevated PSA related to a UTI.
- Recent Physical Activity: Vigorous exercise or strenuous physical activity can temporarily elevate PSA levels. This is a transient effect that typically returns to normal within a short period.
- Stress and Anxiety: Stressful situations can impact hormone levels, which might indirectly affect PSA. While not a direct cause, stress can be a contributing factor.
Impact of Age, Lifestyle, and Medical Procedures
Age, lifestyle, and certain medical procedures play a significant role in influencing PSA levels. This is important to note in order to avoid misinterpreting the results.
- Age: PSA levels naturally tend to increase with age, even in the absence of prostate cancer. This age-related increase is a significant factor to consider when assessing PSA levels.
- Lifestyle: Diet, exercise, and overall health can indirectly affect PSA levels. A healthy lifestyle is crucial for overall well-being, which indirectly impacts PSA.
- Medical Procedures: Procedures like cystoscopy or other prostate-related procedures can cause temporary elevations in PSA levels due to tissue irritation.
Comparison of Common Causes of Elevated PSA
The following table summarizes common causes of elevated PSA levels, highlighting their potential impact on results and the differences in their characteristics.
| Cause | Description | Potential Impact on PSA | Typical Symptoms (if any) |
|---|---|---|---|
| Prostate Cancer | Uncontrolled cell growth in the prostate | Elevated PSA, often persistently | Often asymptomatic in early stages; may include urinary symptoms or pain |
| Benign Prostatic Hyperplasia (BPH) | Enlargement of the prostate gland | Elevated PSA, often moderately | Frequent urination, difficulty urinating, weak urine stream |
| Prostatitis | Inflammation of the prostate gland | Elevated PSA, possibly acutely | Pain in the pelvic region, difficulty urinating, fever |
| Recent Prostate Procedures | Biopsies, surgery, or other prostate procedures | Elevated PSA, temporarily | Pain, bleeding, discomfort related to the procedure |
Interpreting Your Results – A Deeper Look
Understanding your PSA test results is a crucial step in assessing your prostate health. It’s important to remember that a single PSA reading isn’t definitive. Interpreting the results requires considering several factors, including the PSA density and free PSA levels, and the context of your overall health. This section delves deeper into these aspects to help you understand what your numbers mean.Interpreting a PSA test result is a multi-faceted process.
It’s not simply a matter of comparing your number to a pre-defined “normal” range. The significance of your PSA level is better understood when viewed alongside other crucial factors, such as the density of the PSA and the proportion of free PSA. Crucially, your medical history, lifestyle choices, and other health indicators also play a significant role in the interpretation.
PSA Density
PSA density is a calculation that considers the PSA level in relation to the size of your prostate gland. A higher PSA density often suggests a higher likelihood of prostate cancer, even if the overall PSA level is within the “normal” range. This is because a higher density indicates a greater concentration of PSA in the prostate tissue, which can be a sign of abnormal activity.
The calculation is often used by urologists to determine the risk level of potential prostate cancer.
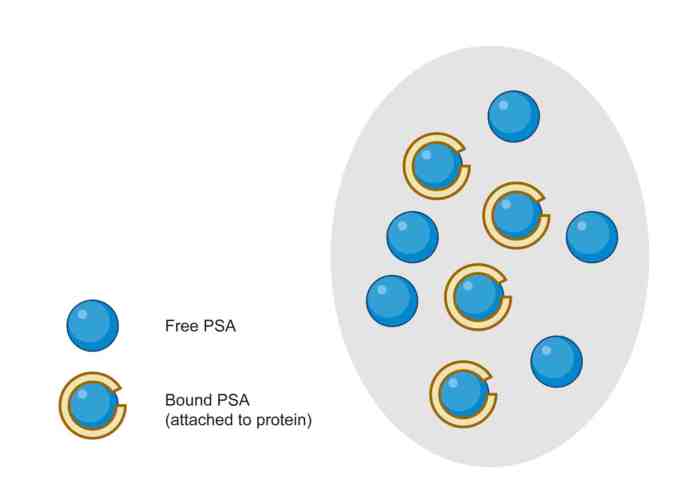
Free PSA
Free PSA refers to the proportion of PSA in the blood that is not bound to other proteins. A higher percentage of free PSA often indicates a lower likelihood of prostate cancer. This is because free PSA is naturally produced by the prostate, whereas bound PSA may be associated with more abnormal processes. Knowing the percentage of free PSA is a significant piece of the puzzle in determining the risk of prostate cancer.
Contextual Factors
Your overall health history and lifestyle factors are critical to interpreting your PSA results. These factors can influence your PSA levels and should be considered alongside the PSA density and free PSA levels. For example, age, race, family history of prostate cancer, and recent medical procedures (like prostate biopsies) all contribute to the overall assessment.
Potential Implications of Various PSA Levels
The following table provides a general overview of potential implications based on different PSA levels. It’s crucial to remember that this is not a definitive diagnosis and must be discussed with your doctor. This table should not be used for self-diagnosis.
| PSA Level (ng/mL) | Potential Implications |
|---|---|
| < 2.5 | Generally considered a lower risk of prostate cancer. |
| 2.5 – 10 | May indicate a moderate risk of prostate cancer. Further investigation is often recommended. |
| > 10 | Indicates a higher risk of prostate cancer. Further investigation and potentially more extensive testing are usually required. |
PSA Test Results and Prostate Cancer Risk
The PSA test, while a valuable tool in prostate health screenings, doesn’t definitively diagnose prostate cancer. Instead, it provides a measure of the amount of PSA in the blood, a protein produced by cells in the prostate gland. Elevated PSA levels can be a sign of various conditions, not just cancer. Understanding the relationship between PSA levels and prostate cancer risk is crucial for accurate interpretation and informed decision-making.Elevated PSA levels are associated with an increased likelihood of prostate cancer, but not all elevated levels indicate cancer.
Figuring out your PSA results can feel a bit overwhelming, but understanding the nuances is key. It’s important to know what your numbers mean, and whether the healthcare system you’re in is a universal coverage system or a single payer system, as the differences can impact how your results are interpreted and managed. For a deeper dive into the nuances of difference between universal coverage and single payer system , check out this helpful resource.
Ultimately, knowing your PSA numbers, and the system you’re part of, is crucial for proactive health management.
Numerous factors influence PSA levels, including age, prostate size, and inflammation. A comprehensive evaluation by a healthcare professional, considering these factors, is necessary to assess the significance of any elevated PSA result.
Correlation Between PSA Levels and Risk
PSA levels don’t directly equate to a specific cancer risk. A higher PSA level generally suggests a greater probability of prostate cancer, but the relationship isn’t linear. Many men with elevated PSA levels never develop prostate cancer, while some men with low PSA levels do.
PSA Velocity
PSA velocity, or the rate at which PSA levels are increasing over time, provides additional context. A rapidly rising PSA level may indicate a more aggressive form of prostate cancer. Monitoring PSA velocity alongside total PSA levels can help assess the potential risk. For instance, a steady increase might suggest a slower progression of the disease, while a sudden surge could be indicative of a more aggressive condition.
Risk Categories Based on PSA Levels and Other Factors
Different risk categories are used to help determine the appropriate course of action for patients with elevated PSA levels. These categories take into account not only the PSA level but also other factors such as age, family history, digital rectal exam findings, and other relevant medical information.
| Risk Category | PSA Level (ng/mL) | Other Important Factors | Implications |
|---|---|---|---|
| Low Risk | < 2.5 | Normal digital rectal exam, no family history of prostate cancer, or other concerning factors | Routine monitoring, potentially less frequent screenings. |
| Intermediate Risk | 2.5-10 | One or more risk factors are present, such as a family history of prostate cancer, or a slightly abnormal digital rectal exam. | More frequent monitoring, possible additional imaging studies, and a conversation with a healthcare professional about further diagnostic procedures. |
| High Risk | >10 | Multiple risk factors, or a significantly abnormal digital rectal exam, family history of prostate cancer. | Further investigation, including biopsy, to determine the nature of the elevated PSA. |
Important Note: This table is for illustrative purposes only and should not be used for self-diagnosis. Consulting a healthcare professional is essential for accurate risk assessment and appropriate management strategies. Each individual’s situation is unique, and a personalized evaluation is crucial.
Next Steps After Receiving Results
Understanding your PSA test results is a crucial first step, but it’s equally important to know what to do next. This involves a careful discussion with your healthcare provider and potentially further diagnostic tests. Your doctor can help you interpret the results in the context of your overall health and medical history, guiding you towards the best course of action.A proactive approach to your health is key.
Taking the necessary steps after receiving your PSA test results ensures you receive the appropriate care and monitoring. This involves actively engaging with your doctor and following their recommendations, which may include further testing to determine the best course of action for your specific situation.
Discussing Results with Your Healthcare Provider
Effective communication with your doctor is essential. Sharing your results and any concerns you have is vital for accurate interpretation and personalized recommendations. This includes discussing any symptoms you may be experiencing, your medical history, and any family history of prostate cancer. Open communication facilitates a thorough understanding of your individual situation.
Further Diagnostic Tests
Further diagnostic tests may be necessary to determine the cause of elevated PSA levels or to assess the risk of prostate cancer. These tests could include a digital rectal exam (DRE), transrectal ultrasound (TRUS), or a biopsy. These procedures are crucial for obtaining a more comprehensive understanding of your condition. The decision to perform these tests is made in conjunction with your doctor, considering the PSA level, the DRE findings, and your overall health.
Questions to Ask Your Doctor
Asking thoughtful questions about your results empowers you to make informed decisions about your health. These questions should be tailored to your specific circumstances. Some examples include: “What does my PSA level mean in the context of my overall health?”, “What are the next steps based on my results?”, “Are there any other tests I should consider?”, “What is the likelihood of having prostate cancer given my results?”, “What are the risks and benefits of each recommended course of action?”
Figuring out your PSA results can feel a bit daunting, but understanding the numbers is key. While we’re on the topic of health, did you know that collagen supplements for skin, like those discussed on this site , can have a positive impact on your overall well-being? Ultimately, taking the time to understand your PSA results is crucial for making informed decisions about your health.
Actions to Take After Receiving PSA Test Results
Taking the following actions after receiving your PSA test results will help ensure you receive the best possible care:
- Schedule a follow-up appointment with your doctor as soon as possible to discuss the results and any concerns you may have.
- Be prepared to discuss your medical history, symptoms, and family history with your doctor.
- Ask specific questions about your results and any recommended tests.
- Follow your doctor’s recommendations for further testing or treatment.
- Be proactive in your health management and regularly monitor your condition as advised by your doctor.
Managing Prostate Health – Prevention and Lifestyle
Taking proactive steps to maintain prostate health is crucial, particularly as we age. A healthy lifestyle, encompassing diet, exercise, and regular check-ups, plays a significant role in reducing the risk of prostate problems. This proactive approach can empower individuals to make informed decisions about their well-being and potentially mitigate future health concerns.A focus on preventative measures, rather than solely reactive ones, can significantly impact the trajectory of prostate health.
By understanding the interplay between lifestyle choices and prostate health, men can take control of their well-being and potentially reduce the risk of developing prostate issues.
Importance of Lifestyle Choices
Lifestyle choices have a profound impact on prostate health. Maintaining a balanced diet, engaging in regular physical activity, and adhering to a healthy routine can contribute to a lower risk of developing prostate-related issues. The benefits extend beyond prostate health, positively affecting overall well-being and longevity.
Diet and Prostate Health
Diet plays a vital role in maintaining prostate health. A balanced diet rich in fruits, vegetables, and whole grains is generally recommended. Limiting processed foods, red meat, and saturated fats is often advised, as these dietary elements may potentially contribute to certain health conditions.
- Fruits and vegetables are rich in antioxidants and vitamins, which may support healthy prostate function.
- Whole grains provide essential fiber and nutrients that can contribute to overall well-being.
- Limiting red meat and processed foods can help regulate inflammation and promote healthy prostate function.
Exercise and Prostate Health
Regular physical activity is beneficial for overall health, including prostate health. Maintaining a healthy weight, through exercise, can also contribute to reduced risk. Exercise can help regulate hormones and maintain overall fitness, impacting prostate health in positive ways.
- Moderate-intensity exercise, such as brisk walking or cycling, can improve circulation and promote overall health.
- Maintaining a healthy weight can contribute to a reduced risk of prostate-related issues.
- Regular exercise can help regulate hormone levels, positively affecting overall health and potentially influencing prostate health.
Significance of Regular Check-ups
Regular check-ups with a healthcare professional are essential for monitoring prostate health. These check-ups, often including PSA tests and digital rectal exams, help in early detection and prompt intervention if needed. Proactive screening can significantly improve treatment outcomes.
- Regular check-ups allow for early detection of potential issues, enabling prompt intervention.
- These check-ups help monitor prostate health over time and identify any changes.
- Early intervention often leads to better treatment outcomes and improved prognosis.
Dietary Recommendations for Prostate Health
The following table Artikels dietary recommendations for promoting prostate health. It’s important to remember that individual needs may vary, and consulting a healthcare professional is always recommended.
| Food Category | Specific Recommendations | Rationale |
|---|---|---|
| Fruits and Vegetables | Focus on a variety of colorful fruits and vegetables, including berries, citrus fruits, leafy greens, and cruciferous vegetables. | Rich in antioxidants and vitamins that may support healthy prostate function. |
| Whole Grains | Choose whole-grain breads, cereals, and pasta over refined grains. | Provide essential fiber and nutrients that contribute to overall well-being. |
| Lean Protein | Include lean protein sources like fish, poultry, and beans. | Provides essential nutrients without excess saturated fat. |
| Healthy Fats | Incorporate healthy fats from sources like avocados, nuts, and olive oil. | Support overall health and hormone regulation. |
| Dairy Products (Moderate) | Consume dairy products in moderation. | May impact hormone balance. |
| Limit Processed Foods, Red Meat, and Saturated Fats | Reduce intake of processed foods, red meat, and foods high in saturated fats. | May contribute to inflammation and certain health conditions. |
Illustrative Case Studies: Understanding Your Psa Results
Understanding PSA results is crucial, but interpreting them in the context of an individual’s health history and lifestyle is equally important. These case studies illustrate how a holistic approach to evaluating PSA levels can lead to a more accurate assessment of prostate health. Remember, these are hypothetical examples and should not be used for self-diagnosis. Always consult with a healthcare professional.A comprehensive evaluation of a patient’s PSA results necessitates consideration of multiple factors beyond the numerical value itself.
This includes medical history, lifestyle choices, family history, and other relevant clinical findings.
Case Study 1: Elevated PSA Level
A 55-year-old male presents with a slightly elevated PSA level of 3.5 ng/mL. His medical history is unremarkable, except for a family history of prostate cancer in his father at age 65. He reports a sedentary lifestyle with a history of smoking. The diagnostic steps typically involve a thorough physical examination, including a digital rectal exam (DRE) to assess the prostate for any abnormalities.
Further investigation might include a repeat PSA test, transrectal ultrasound (TRUS), and potentially a prostate biopsy to obtain tissue samples for microscopic examination. A multiparametric MRI scan might also be considered to assess the prostate structure.The importance of a holistic approach in this case is evident. The elevated PSA level, while suggestive of potential prostate issues, does not definitively confirm cancer.
The patient’s family history, lifestyle, and other clinical findings are all significant factors to consider. The patient’s age and smoking history could also contribute to the elevated PSA level.
Case Study 2: Normal PSA Level
A 62-year-old male with a history of hypertension and a family history of benign prostatic hyperplasia (BPH) presents with a normal PSA level of 2.0 ng/mL. He reports maintaining a healthy diet and regular exercise. In this scenario, the normal PSA level suggests a lower risk of prostate cancer. However, a normal PSA does not guarantee the absence of any prostate problems.
Benign prostatic hyperplasia, an enlargement of the prostate gland, is a common cause of urinary symptoms. The patient’s lifestyle choices and history of BPH in his family further contribute to the interpretation of his normal PSA level. Regular checkups and monitoring are crucial to assess any potential changes over time.
Visual Aids and Explanations
Understanding your PSA results can be a complex process. Visual aids and detailed explanations can significantly help you grasp the nuances of prostate health and the PSA test. This section provides a visual representation of a healthy prostate and one with cancerous growth, along with an explanation of prostate anatomy, the PSA blood test process, and the pathway of a PSA molecule in the body.
This will help contextualize the numerical results you receive and allow you to better understand the possible implications.
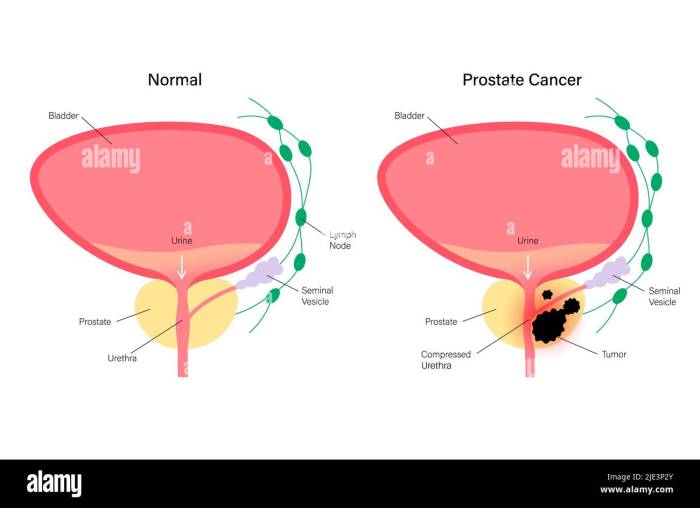
Healthy vs. Cancerous Prostate
A healthy prostate gland is a walnut-shaped organ, typically about the size of a fist. The images would show a smooth, even surface. A cancerous prostate gland, on the other hand, may exhibit irregular shapes, growths, or masses. These abnormal areas might appear as bulges or lumps within the overall structure. These visual differences can help differentiate normal prostate tissue from cancerous tissue.
These differences in appearance are often evident in medical imaging.
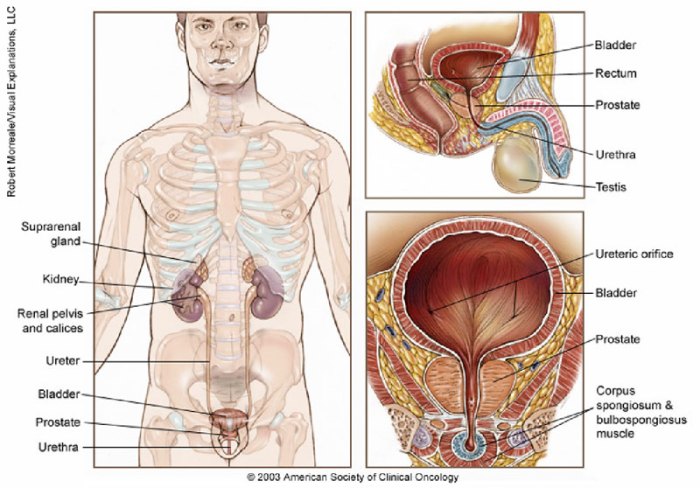
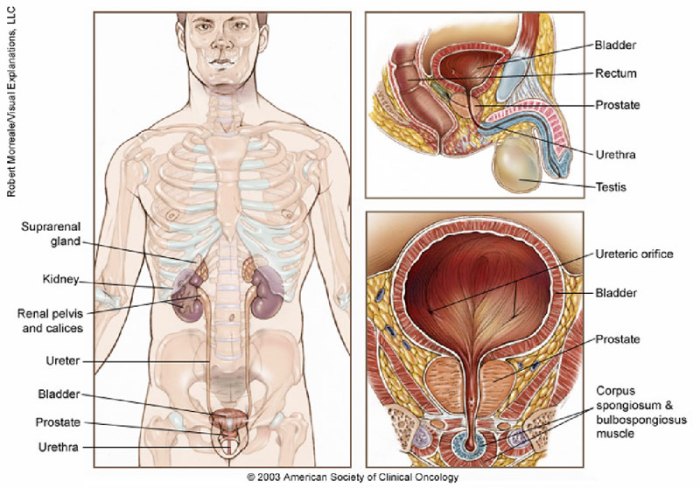
Prostate Anatomy
The prostate gland is a complex organ, composed of several parts that work together to produce seminal fluid. A diagram would be helpful here, showing the lobes of the prostate (e.g., anterior, posterior, lateral, and median lobes) and their respective locations within the pelvic region. This would also indicate the urethra passing through the center of the prostate, which is essential for understanding the prostate’s role in urination and ejaculation.
Accurate anatomical knowledge is vital for interpreting PSA test results.
The PSA Blood Test Process
A PSA blood test involves drawing a blood sample, which is then analyzed for the presence of prostate-specific antigen. A diagram illustrating this process would show a patient with a needle being inserted into a vein to collect the blood sample. The sample is then sent to a laboratory where the levels of PSA are measured. A detailed explanation should accompany the diagram, outlining the steps involved, from sample collection to laboratory analysis, and the crucial importance of proper blood collection technique to ensure accurate results.
PSA Molecule Pathway
The pathway of a PSA molecule in the body would be represented graphically. The diagram should show the production of PSA in the prostate gland, its release into the bloodstream, and its eventual detection in the blood sample during the PSA test. Highlighting specific tissues or organs that might influence PSA levels, and the potential factors impacting the levels, will provide a comprehensive understanding of the molecule’s journey.
This illustration would also include information on how PSA might be cleared from the body. For instance, it could highlight the potential roles of the liver or kidneys in this process.
Final Summary
In conclusion, understanding your PSA results is a multifaceted process that requires a comprehensive approach. This guide has provided a foundational understanding of PSA testing, interpretation, and potential risks. Remember, always discuss your results with a healthcare professional. They can provide personalized guidance and support you in making informed decisions about your health.