Reverse walking in physical therapy is a powerful technique gaining traction for improving balance, gait, and strength. This approach challenges the typical forward motion, offering unique benefits for various patient populations. We’ll explore the biomechanics, benefits, and safety considerations, along with exercise progressions and modifications. This comprehensive guide dives into the specifics of reverse walking,…
Tag: physical therapy
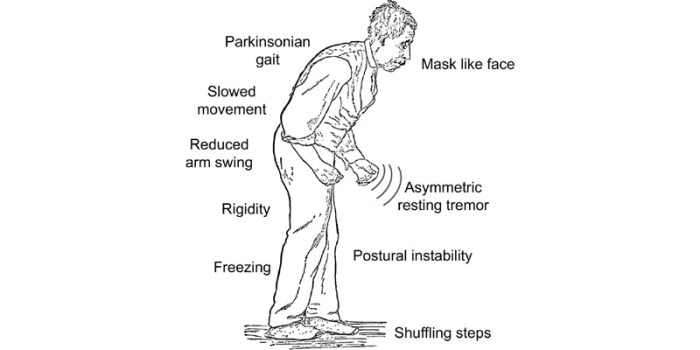
Gait Training in Physical Therapy A Comprehensive Guide
Gait training in physical therapy focuses on restoring and improving normal walking patterns. It’s crucial for daily life, impacting everything from mobility to overall health. Physical therapists address a wide range of gait abnormalities, tailoring interventions to specific needs. This comprehensive guide explores the entire process, from assessment and evaluation to interventions, patient selection, and…
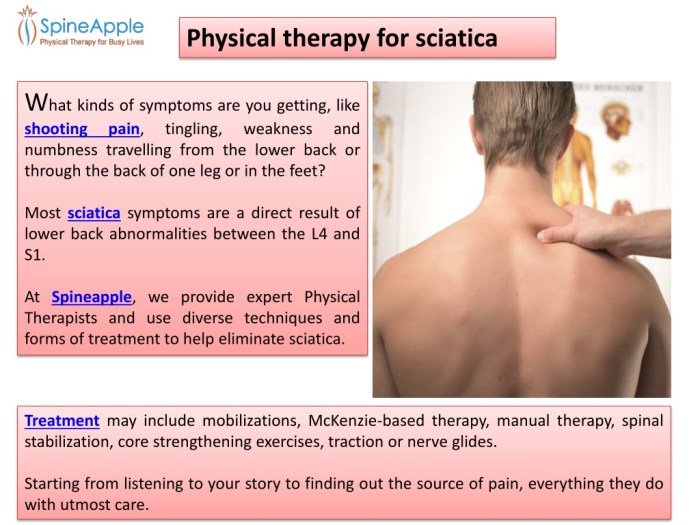
Physical Therapy for Sciatica A Comprehensive Guide
Physical therapy for sciatica offers a powerful approach to managing and relieving this debilitating condition. It delves into understanding the root causes, identifying effective treatments, and empowering patients with self-management strategies. This guide will explore the various techniques and exercises used in physical therapy to alleviate sciatica pain, improve posture, and enhance overall well-being. This…
Treating Diastasis Recti with Physical Therapy A Guide
Treating diastasis recti with physical therapy is a comprehensive approach to managing this common postpartum condition. It involves a personalized plan encompassing assessment, targeted exercises, and patient education to effectively address the separation of abdominal muscles, often accompanied by associated symptoms like back pain and pelvic floor dysfunction. This guide delves into the various aspects…
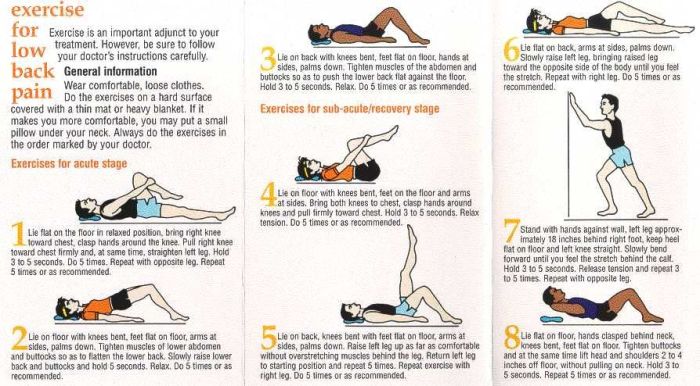
Physical Therapy and Exercises for Low Back Pain A Comprehensive Guide
Physical therapy and exercises for low back pain offer a powerful approach to managing and alleviating discomfort. This guide delves into the various types of exercises, tailored programs, and crucial lifestyle considerations to effectively address low back pain. We’ll explore everything from understanding the different types of back pain to creating a personalized home exercise…
Do I Need a Knee Brace? A Comprehensive Guide
Do I need a knee brace? This comprehensive guide delves into the complexities of knee pain and when a brace might be the right solution. We’ll explore various types of knee pain, potential causes, and the importance of consulting a healthcare professional. Beyond simply answering the question, we’ll equip you with the knowledge to make…