Patella anatomy function and treatment is a comprehensive look at the kneecap’s role in movement, potential problems like pain and dislocation, and the various treatment options available. Understanding the patella’s structure, its function in the knee joint, and the different conditions affecting it is crucial for anyone seeking to improve knee health and performance. We’ll explore everything from its intricate structure and role in knee extension to the causes and treatments of common knee problems.
This detailed exploration delves into the complex interplay of the patella with surrounding structures, including the femur and various soft tissues. It examines how the patella contributes to smooth knee movements, absorbs impact, and influences the patellofemoral joint’s mechanics. The discussion will cover the anatomy of the patella, its function in normal and various activities, and the different pathologies that can affect its function.
We’ll also touch on the role of imaging techniques in diagnosing problems and the importance of rehabilitation after injury or surgery.
Patella Structure
The patella, often called the kneecap, is a remarkably important sesamoid bone within the knee joint. Its unique shape and location play a crucial role in the mechanics of knee extension and patellofemoral stability. Understanding its structure is fundamental to comprehending its function and potential pathologies.The patella’s precise anatomical features, from its surface textures to its relationship with surrounding tissues, contribute significantly to its overall function.
Its robust structure allows for the transmission of forces during movement, but also necessitates a high level of structural integrity to prevent injury.
Patella Shape and Size
The patella is roughly triangular in shape, though its exact dimensions can vary between individuals. Its base, the wider, superior portion, is broader than its apex, the pointed inferior tip. The size of the patella is also influenced by factors like gender and body type. On average, the patella measures approximately 5 centimeters in length and 3 centimeters in width.
Its location is critical to its function, situated anterior to the distal femur and superior to the tibial tuberosity.
Understanding patella anatomy, function, and treatment is crucial for overall knee health. It’s a small but vital component of the knee joint, facilitating smooth movement. However, sometimes, a completely different issue can present with similar symptoms – severe stomach pain. If you’re experiencing this, it’s important to know when to seek immediate medical attention, like when visiting the ER.
For guidance on this, check out this helpful resource: severe stomach pain when to go to the er. Regardless of the cause of pain, proper diagnosis and treatment of conditions like patella issues are essential for recovery.
Patella Location and Surrounding Structures
The patella’s location, nestled within the quadriceps tendon superiorly and the patellar ligament inferiorly, positions it centrally within the knee joint. This strategic positioning allows it to act as a pulley, improving the mechanical advantage of the quadriceps muscle during knee extension. Crucially, the patella is flanked by the vastus medialis and vastus lateralis muscles, and its articulation with the femoral condyles is pivotal for proper knee movement.
Patellar Layers and Surfaces
The patella is composed of layers of dense cortical bone and spongy cancellous bone. The anterior surface is typically smooth and convex, whereas the posterior surface is characterized by articular cartilage, which is crucial for smooth gliding against the femoral condyles. This smooth, articular cartilage layer is thinner on the posterior surface compared to the anterior. Differences in the thickness and composition of these surfaces reflect the different mechanical stresses each area experiences during knee flexion and extension.
Bony Landmarks of the Patella
Various bony landmarks define the patella and contribute to its overall architecture. The superior pole, the inferior pole, and the medial and lateral borders are crucial for identifying the patella’s position and orientation within the knee joint. These landmarks aid in the precise assessment of patellar tracking and potential abnormalities. These landmarks are critical for surgeons during surgical procedures and for diagnosing conditions like patellar dislocations.
Summary of Patellar Structures
| Name | Description | Location | Function |
|---|---|---|---|
| Patellar Base | Broad, superior portion | Superior aspect of the patella | Broadens the area for tendon attachment |
| Patellar Apex | Pointed, inferior tip | Inferior aspect of the patella | Attachment point for the patellar ligament |
| Anterior Surface | Smooth, convex | Facing the front of the knee | Facilitates gliding over the femur |
| Posterior Surface | Articular cartilage | Facing the femur | Provides a smooth surface for articulation with the femur |
| Medial Border | Inner edge | Inner side of the patella | Helps define the shape and position |
| Lateral Border | Outer edge | Outer side of the patella | Helps define the shape and position |
Patella Function in Knee Movement
The patella, or kneecap, is a remarkably important component of the knee joint, playing a crucial role in extending and flexing the leg. Its unique shape and position within the knee joint influence the mechanics of the patellofemoral joint, a critical part of overall knee function. This section will explore the patella’s role in knee movement, detailing its impact on joint mechanics and its function in distributing forces during various activities.The patella acts as a sort of movable pulley, significantly enhancing the efficiency of knee extension.
Its positioning within the quadriceps tendon allows for a more direct line of force transmission, which is particularly important for activities requiring powerful leg extensions. This leverage system is crucial for tasks such as walking, running, and jumping. Further, the patella plays a key role in protecting the underlying articular cartilage of the knee joint.
Role of the Patella in Knee Extension
The patella is intricately linked to the quadriceps muscle group. During knee extension, the quadriceps muscle contracts, pulling on the patellar tendon. The patella’s smooth surface and the patellofemoral groove of the femur facilitate a smooth gliding motion, enhancing the efficiency of the extension process. This action increases the leverage of the quadriceps muscle, making knee extension stronger and more effective.
This optimized force transmission is crucial for activities requiring substantial leg strength, like jumping or climbing stairs.
Influence on Patellofemoral Joint Mechanics
The patella’s shape and position directly impact the patellofemoral joint’s mechanics. The patella’s smooth articular cartilage and the matching groove in the femur create a low-friction gliding surface. This allows for smooth movement during both flexion and extension. Any abnormalities in the patella’s tracking or the patellofemoral groove can lead to pain and discomfort, highlighting the importance of proper patellar function.
Patella’s Function in Force Distribution
During weight-bearing activities, the patella plays a vital role in distributing forces across the knee joint. The patella acts as a load-bearing component, redirecting forces from the quadriceps muscle to the femur. This force distribution is essential for preventing excessive stress on the joint and maintaining its integrity during activities such as walking and running. This force redirection is especially crucial during activities that involve high-impact loading, like jumping.
Understanding patella anatomy, function, and treatment options is crucial for knee health. A strong, properly functioning patella is essential for smooth movement and preventing injuries. Supporting optimal gut health through a balanced diet including probiotics plus fiber, like those found in probiotics plus fiber gut health , can contribute to overall well-being, potentially impacting joint health as well.
Ultimately, proper nutrition and care for the patella are key to maintaining a healthy, active lifestyle.
Patella Interaction with Femur During Flexion and Extension
The patella’s interaction with the femur during flexion and extension follows a specific pattern. During knee extension, the patella glides superiorly along the femoral groove. As the knee flexes, the patella glides inferiorly along the groove. This coordinated movement is essential for smooth and efficient knee function. The patella’s movement is tightly coupled with the action of the quadriceps muscle and the surrounding ligaments.
Patella Function in Various Activities
| Activity | Patella’s Role |
|---|---|
| Walking | The patella facilitates smooth, controlled knee extension and flexion during each step. Force distribution is crucial for maintaining stability. |
| Running | The patella supports increased loading forces and rapid changes in knee flexion and extension. The smooth glide is critical to avoid impact-related stress. |
| Jumping | The patella experiences high forces during the extension phase, crucial for propelling the body upwards. Force distribution is maximized to prevent injury. |
Patellofemoral Pain Syndrome (PFPS)
Patellofemoral pain syndrome (PFPS), often referred to as runner’s knee, is a common condition causing pain around the kneecap. This discomfort can significantly impact daily activities and athletic performance. Understanding the causes, contributing factors, symptoms, and treatment options is crucial for effective management.
Common Causes of PFPS
PFPS arises from various factors affecting the patellofemoral joint, where the kneecap (patella) glides within the groove of the thigh bone (femur). Overuse, muscle imbalances, and biomechanical issues are frequently implicated. Poor tracking of the patella, or its improper movement within the groove, is a major contributor. Trauma, while less common, can also lead to PFPS.
Contributing Factors to Patellar Tracking Issues
Several factors can disrupt the smooth gliding motion of the patella. Muscle imbalances, particularly weakness in the quadriceps muscles or the muscles that stabilize the knee (e.g., vastus medialis obliquus), can lead to improper tracking. Tightness in the surrounding soft tissues, such as the iliotibial band or hamstrings, can also contribute to abnormal patellar movement. Furthermore, structural abnormalities, like a shallow patellar groove, can predispose individuals to patellar tracking problems.
Variations in leg length and foot pronation can also affect the biomechanics of the knee, contributing to PFPS.
Typical Symptoms Associated with PFPS
Pain in the front of the knee, often worsening with activity, is a hallmark symptom of PFPS. The pain may be localized directly around the patella or more diffuse, radiating to the sides of the knee. Swelling and tenderness around the kneecap are also common. Some individuals experience clicking, popping, or grinding sensations within the knee joint, especially during certain movements.
Common Risk Factors Associated with PFPS
Several factors increase the risk of developing PFPS. Individuals who participate in activities that involve repetitive knee bending, such as running, jumping, or squatting, are more susceptible. Females are disproportionately affected compared to males. Obesity, which can lead to increased stress on the knee joint, is another risk factor. Athletes in sports requiring frequent changes in direction or jumping are at heightened risk.
A history of previous knee injuries or trauma can also increase susceptibility to PFPS.
Treatment Options for PFPS
| Category | Treatment Options | Description |
|---|---|---|
| Conservative Treatments | Rest and activity modification | Avoiding activities that exacerbate pain is essential. Gradual return to activity is crucial. |
| Conservative Treatments | Physical therapy | Strengthening exercises, particularly of the quadriceps and hip muscles, are often crucial. Stretching tight muscles and improving flexibility are also important. Proper biomechanical assessment and correction are frequently implemented. |
| Conservative Treatments | Bracing or taping | Provides support and helps to stabilize the patella, reducing pain and improving tracking. |
| Conservative Treatments | Medications | Over-the-counter pain relievers (NSAIDs) can help manage pain and inflammation. |
| Conservative Treatments | Injections | Corticosteroid injections can reduce inflammation, but their long-term efficacy and potential side effects should be considered. |
| Surgical Treatments | Arthroscopy | Involves minimally invasive procedures to address underlying structural issues, such as loose bodies or cartilage damage. |
| Surgical Treatments | Patellar realignment surgery | Procedures like tibial tubercle osteotomy (TTO) or patellar resurfacing may be considered for severe cases with persistent pain and dysfunction. |
Patellar Dislocation
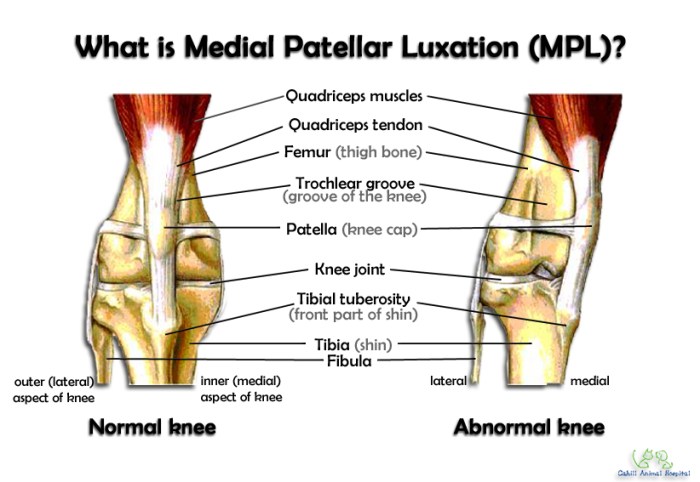
Patellar dislocation, a common knee injury, involves the patella (kneecap) moving out of its normal position in the groove of the femur (thigh bone). This painful condition can result in significant limitations in daily activities and, if left untreated, may lead to long-term problems. Understanding the causes, diagnosis, and treatment options is crucial for effective management.
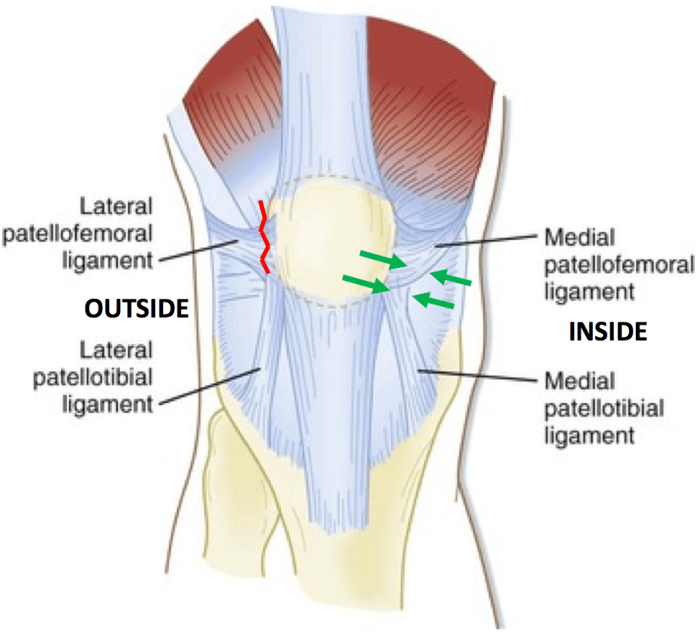
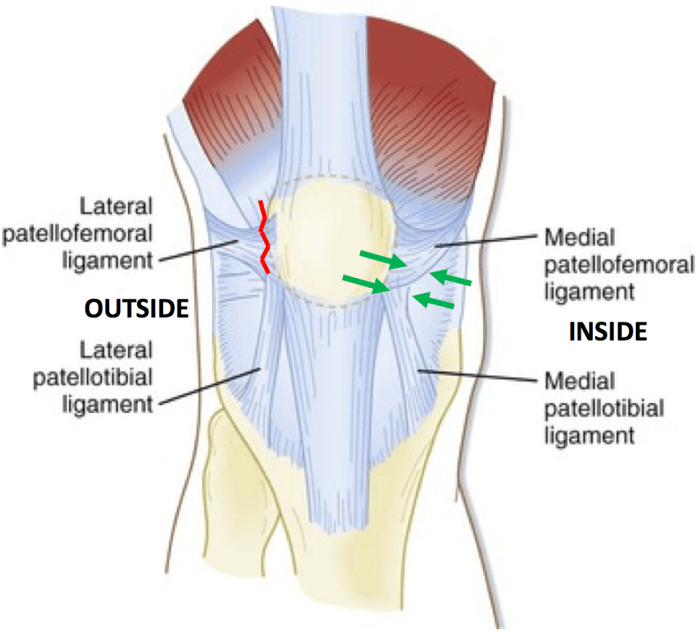
Anatomical Structures Providing Patellar Stability
The patella’s stability relies on a complex interplay of anatomical structures. These structures work together to maintain the patella within the trochlear groove. Crucially, the patellofemoral joint’s shape, the surrounding soft tissues, and the dynamic forces exerted during movement all contribute to this stability. A shallow or malformed groove, inadequate soft tissue support, or muscular imbalances can increase the risk of dislocation.
Mechanism of Patellar Dislocation
Patellar dislocation typically occurs when a significant force is applied to the knee, often during a twisting or lateral (sideways) movement. This forceful movement overcomes the stabilizing structures, causing the patella to shift out of its normal position. Common causes include sports activities involving sudden changes in direction or impact. For instance, a lateral blow to the knee during basketball or a forceful twisting motion during skiing can induce patellar dislocation.
Clinical Presentation of Patellar Dislocation
The clinical presentation of patellar dislocation varies depending on the severity of the injury. Patients often report a sudden, sharp pain in the knee, accompanied by a feeling of the kneecap popping out of place. The knee may appear deformed, with the patella visibly displaced. Immediate swelling, bruising, and tenderness are also common. Limited range of motion and difficulty bearing weight are frequently observed.
In addition to the above, associated symptoms such as numbness or tingling may be present, particularly if the nerves around the knee have been affected by the injury.
Types of Patellar Dislocations, Patella anatomy function and treatment
Patellar dislocations can be categorized based on the direction of the displacement. The most common type is lateral patellar dislocation, where the patella moves outward. Medial patellar dislocations, where the patella moves inward, are less frequent. These distinctions are important as they influence the specific treatment approach and potential recurrence risk. Understanding the specific type of dislocation is essential to develop an effective treatment plan.
Surgical Techniques for Patellar Stabilization
Surgical intervention is often necessary for recurrent patellar dislocations to restore stability and prevent future episodes. Various surgical techniques are employed, each with its own advantages and disadvantages.
| Surgical Technique | Description | Advantages | Disadvantages |
|---|---|---|---|
| Lateral Release | Surgical release of tight lateral structures (e.g., IT band, lateral retinaculum) to allow more freedom for the patella. | Relatively less invasive; can be performed arthroscopically. | Potential for increased patellar tracking problems if not performed carefully. |
| Medial Plication | Reinforcing the medial structures (e.g., medial retinaculum) to improve patellar stability. | Effective in addressing medial instability. | May cause tightness if not properly performed. |
| Tibial Tubercle Advancement | Moving the tibial tubercle (where the patellar tendon attaches) medially. | Addresses underlying skeletal malalignment issues. | More invasive procedure; longer recovery time. |
| Patellar Resurfacing | Smooths the articular surfaces of the patella and trochlear groove. | Addresses cartilage damage. | Higher risk of complications if the cartilage is not damaged. |
| Combined Techniques | Combining multiple techniques to address various aspects of patellar instability. | Highly effective for complex cases. | More invasive and demanding. |
Patella Imaging Techniques: Patella Anatomy Function And Treatment
Understanding the patella’s intricate structure and function often necessitates the use of imaging techniques. These methods provide crucial visual insights into the patella and surrounding tissues, aiding in accurate diagnoses and guiding treatment strategies. This section explores the various imaging modalities used to evaluate patellar conditions, highlighting typical findings and their application in diagnosing fractures, dislocations, and other pathologies.Imaging plays a pivotal role in evaluating patellar alignment, tracking, and overall health.
Different imaging techniques offer varying levels of detail and are chosen based on the specific clinical question and suspected pathology. Radiographs, MRIs, and ultrasounds are the primary modalities employed, each with unique strengths and weaknesses.
Radiographic Assessment of the Patella
Radiographs, or X-rays, are frequently the initial imaging modality used to evaluate patellar conditions. Their accessibility, low cost, and rapid acquisition make them valuable screening tools. Specific views are crucial for assessing patellar alignment and tracking. The standard anteroposterior (AP) view and lateral view are often employed. The Merchant view, specifically designed to assess patellar tracking, is particularly helpful in identifying patellofemoral pain syndrome (PFPS) and other alignment issues.
“Radiographs are essential for evaluating the patella’s overall shape, size, and any evidence of fractures or dislocations.”
Magnetic Resonance Imaging (MRI)
MRI provides detailed soft tissue visualization, making it invaluable for assessing patellar cartilage, ligaments, tendons, and surrounding structures. This allows for the evaluation of cartilage damage, meniscal tears, and soft tissue injuries associated with patellar problems.
“MRI excels in visualizing the soft tissues surrounding the patella, providing valuable insights into the condition of the cartilage and supporting structures.”
Ultrasound
Ultrasound offers a real-time, dynamic assessment of the patella and surrounding soft tissues. It can be particularly useful for evaluating tendonitis, bursitis, and other soft tissue conditions. Ultrasound is also useful in evaluating for fluid collections (effusions) around the patella.
“Ultrasound provides a real-time, dynamic view of the patella and surrounding structures, which is helpful for evaluating soft tissue injuries.”
Typical Imaging Findings
Radiographs typically reveal fractures, dislocations, and significant changes in patellar alignment. MRI can highlight cartilage lesions, meniscal tears, ligamentous injuries, and edema within the surrounding soft tissues. Ultrasound demonstrates the presence of fluid collections, tendon tears, and bursitis.
Imaging Techniques for Specific Pathologies
Radiographs are essential in detecting patellar fractures, often displaying a disrupted patellar cortex. MRIs are superior for assessing the extent of cartilage damage and identifying associated soft tissue injuries in patellar dislocations. Ultrasound can be used to guide needle aspiration for effusions or to assess for soft tissue tears, particularly in cases of suspected tendinopathy.
Radiographic Views for Patellar Alignment and Tracking
The Merchant view, an axial view, is crucial for assessing patellar tracking and evaluating patellofemoral joint congruency. It provides a detailed image of the patellar position relative to the femoral trochlear groove. The lateral view helps determine patellar tilt and height. These views, when carefully analyzed, can identify subtle deviations in patellar alignment.
Comparison of Imaging Techniques
| Imaging Technique | Advantages | Disadvantages |
|---|---|---|
| Radiograph | Low cost, quick acquisition, readily available | Limited soft tissue detail, does not visualize cartilage or ligaments |
| MRI | Excellent soft tissue contrast, visualization of cartilage and ligaments | Higher cost, longer acquisition time, potential for artifacts |
| Ultrasound | Real-time imaging, portable, relatively inexpensive | Limited depth penetration, operator dependent, less detail than MRI |
Patella Rehabilitation
Proper patellar rehabilitation is crucial for a successful recovery from injury or surgery. A well-structured program helps restore strength, flexibility, and function to the knee, minimizing the risk of future problems and promoting a return to pre-injury activities. This involves carefully progressing through various phases, focusing on targeted exercises and mindful attention to pain management.
Importance of Proper Rehabilitation
Effective rehabilitation following patellar injury or surgery is vital for long-term knee health. It aims to rebuild strength and stability around the patella, ensuring proper tracking and minimizing the risk of re-injury. A tailored rehabilitation program, carefully guided by a healthcare professional, helps patients regain full knee function and return to their desired activities.
Phases of a Typical Patellar Rehabilitation Program
The rehabilitation process typically involves distinct phases, each with specific goals and exercises. These phases are designed to gradually increase the load and complexity of the exercises as the knee heals and regains strength. Early phases focus on protecting the injured area and promoting healing, progressing to strengthening and functional exercises as healing progresses.
Common Strengthening Exercises
Strengthening the muscles surrounding the patella is essential for restoring stability and function. This includes the quadriceps, hamstrings, and hip muscles, all of which play a role in proper knee mechanics. Exercises are carefully selected and progressively intensified to avoid overexertion and promote optimal healing.
Understanding patella anatomy, function, and treatment is crucial for knee health. The patella, or kneecap, plays a vital role in knee extension and stability. Different treatments exist for patella problems, depending on the specific issue. While exploring these treatments, it’s important to consider the nuances of alternative pain management options, like comparing the efficacy of medications like suboxone vs methadone, which can be useful in some cases.
Suboxone vs methadone how do they differ This comparison can offer insights into potential side effects and efficacy when considering long-term pain management strategies. Ultimately, a comprehensive approach focusing on the patella’s anatomy and function remains key to successful recovery.
- Quadriceps Strengthening: Strengthening the quadriceps is paramount for knee stability. Exercises like straight leg raises, quad sets, and stationary bike exercises, progressively increasing resistance, are key components of this phase. Proper form is crucial to prevent further injury and ensure the muscles are being worked effectively.
- Hamstring Strengthening: Strengthening the hamstrings is equally important for knee stability and preventing patellar tracking issues. Exercises like hamstring curls, glute-ham raises, and leg extensions, with gradual increases in resistance, are essential. Maintaining proper form is essential to avoid straining the hamstring muscles and promoting their full potential.
- Hip Strengthening: Strengthening hip muscles is critical for overall knee health and stability. Exercises targeting hip abductors, adductors, and external rotators, like clamshells, side-lying hip abductions, and hip bridges, help to improve balance and stability. The hip plays a crucial role in maintaining patellar tracking and should be carefully strengthened to ensure proper function.
Proprioceptive Training
Proprioceptive training focuses on improving the body’s awareness of joint position and movement. This is essential for restoring balance and stability to the knee after injury or surgery. It enhances the neuromuscular control of the knee joint, helping to prevent future problems and improve performance.
Exercises for Strengthening Muscles
The following table provides examples of exercises for strengthening the quadriceps, hamstrings, and hip muscles. Progression and modifications are crucial depending on the individual’s specific needs and recovery stage.
| Muscle Group | Exercise | Description |
|---|---|---|
| Quadriceps | Straight Leg Raises | Lie on back, raise one leg straight, maintaining a controlled movement. |
| Quadriceps | Quad Sets | Squeeze quadriceps muscles for several seconds, repeatedly. |
| Quadriceps | Leg Press | Use a leg press machine with proper form and controlled movement. |
| Hamstrings | Hamstring Curls | Use a hamstring curl machine or resistance band. |
| Hamstrings | Glute-Ham Raises | Focus on hip extension and hamstring contraction. |
| Hip | Clamshells | Lie on side, lift the top knee, maintaining a controlled movement. |
| Hip | Side-lying Hip Abduction | Lie on side, lift leg out to the side with resistance band. |
| Hip | Hip Bridges | Lie on back, lift hips off the ground, squeezing glutes. |
Patellar Anatomy Variations
The kneecap, or patella, plays a crucial role in knee function, and its anatomy isn’t a one-size-fits-all. Variations in patellar size, shape, and orientation can significantly influence how the patella tracks within the knee joint. Understanding these variations is essential for recognizing potential predispositions to patellofemoral pain and other knee problems.Variations in patellar anatomy are a complex interplay of genetic and developmental factors, which can impact patellar tracking and stability.
These variations can affect the patella’s position relative to the femur (thigh bone) and the surrounding soft tissues. Such variations can be subtle or more pronounced, and their impact can vary widely between individuals. Recognizing these variations can be helpful in assessing risk factors for patellar issues.
Patellar Size Variations
Patellar size can vary considerably between individuals. A larger patella might increase the potential for impingement or maltracking during knee movement. Conversely, a smaller patella might not provide adequate support, leading to instability. A significant size difference compared to the femoral groove can contribute to patellar tracking issues. This is further influenced by the relationship between the patella and the trochlear groove of the femur.
Patellar Shape Variations
Patellar shape is another crucial aspect of anatomy. Variations in the shape of the patella’s anterior (front) surface or the lateral (outer) aspect can affect its interactions with the surrounding tissues. A patella with a more pronounced lateral facet (the side surface) or a less-rounded shape might increase the risk of lateral tracking problems. The variations in shape and the degree of curvature can lead to differences in patella stability.
Patellar Orientation Variations
The orientation of the patella in the knee joint is critical. A patella that’s positioned more laterally or medially (toward the inner or outer side of the knee) might not track correctly within the trochlear groove. This deviation from the ideal alignment can increase stress on the patellofemoral joint and predispose the individual to patellar tracking issues. A patella that is more obliquely positioned, for example, could lead to increased lateral pressure on the joint.
Genetic and Developmental Factors
Genetic predispositions play a role in shaping patellar anatomy. Certain genes might influence the development of the patella and its relationship with the femur. Furthermore, factors like the rate of skeletal maturation can influence patellar development. This interplay of genetics and development can create a wide range of patellar variations. The development of the knee joint and the surrounding soft tissues during growth is also important in determining the patellar orientation and stability.
Anatomical Factors Predisposing to Patellar Problems
Several anatomical factors can increase the risk of patellar problems. These factors include:
- Deep trochlear groove: A shallow trochlear groove can result in inadequate support for the patella, increasing the likelihood of patellar maltracking. This shallowness might not allow for appropriate patellar guidance.
- High patella: A patella positioned higher in the femoral groove may increase stress on the joint. This positioning can lead to maltracking during knee flexion and extension.
- Q-angle: The Q-angle, formed by the femur and tibia, describes the alignment of the lower limbs. A significant Q-angle variation may contribute to lateral tracking problems and increased stress on the patellofemoral joint.
- Lateral patellar tilt: A patella that tilts laterally might not track correctly in the femoral groove. This can lead to increased friction and pain.
Summary Table of Patellar Variations
| Variation Type | Description | Potential Implications |
|---|---|---|
| Patellar Size | Larger or smaller than average | Increased risk of impingement or instability |
| Patellar Shape | Pronounced lateral facet, less-rounded shape | Increased risk of lateral tracking problems |
| Patellar Orientation | Lateral or medial deviation | Potential for maltracking, increased stress on joint |
| Trochlear Groove Depth | Shallow groove | Inadequate support for patella, increased maltracking risk |
| High Patella | Higher position in femoral groove | Increased stress on joint, potential maltracking |
| Q-Angle | Significant deviation from normal | Lateral tracking problems, increased stress on patellofemoral joint |
| Lateral Patellar Tilt | Lateral tilt of the patella | Maltracking, increased friction, potential pain |
Closing Summary
In conclusion, the patella’s intricate anatomy and crucial role in knee function are highlighted. We’ve examined the intricate relationship between the patella and the surrounding structures, its critical role in knee extension and impact absorption, and the range of conditions that can affect its function. Understanding the causes, symptoms, and treatment options for various patellar problems is essential for maintaining knee health.
This overview serves as a foundational knowledge base, emphasizing the importance of proper care and rehabilitation to ensure optimal knee function.