How to coughing after surgery is a crucial aspect of post-operative care. This guide delves into the complexities of post-surgical coughing, exploring the physiological reasons behind it, and providing practical strategies for effective management. From understanding the underlying mechanisms to implementing preventative measures and patient support, we’ll cover every facet of this essential topic. This…
Tag: pain management
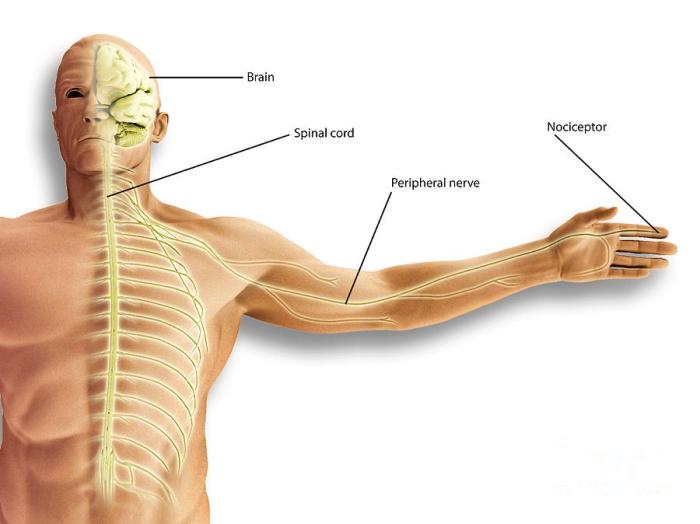
What is Nociceptive Pain A Deep Dive
What is nociceptive pain? It’s pain originating from actual or potential tissue damage. This isn’t just a fleeting discomfort; it’s a complex physiological response triggered by various stimuli. From a simple burn to a persistent muscle strain, understanding the mechanisms behind nociceptive pain is crucial for effective pain management. This exploration delves into the science…
Dosing Hydrocodone How Much Is Safe?
Dosing hydrocodone how much is safe? This crucial question is often at the forefront of pain management discussions. Understanding the proper dosage of hydrocodone is paramount to ensuring its effective use while minimizing potential risks. Hydrocodone, a commonly prescribed opioid, plays a vital role in pain relief, but its use carries inherent dangers. Proper administration,…
Naltrexone for Pain Management What Can It Treat?
Naltrexone for pain management what can it treat – Naltrexone for pain management: what can it treat? This exploration dives into the potential of naltrexone, a medication primarily known for its role in addiction treatment, as a novel approach to managing chronic pain. We’ll examine its mechanism of action, potential benefits, and drawbacks, comparing its…
Massage Therapy Helps Relieve Pain A Deep Dive
Massage therapy helps relieve pain, offering a holistic approach to managing discomfort. This exploration delves into various massage techniques, their physiological effects, and the types of pain they can address. We’ll examine specific muscle groups and areas often targeted for relief, along with a comparative analysis of different massage styles. Beyond the basics, we’ll investigate…
Can I Keep Working with Fibromyalgia and CFS?
Can I keep working with fibromyalgia and CFS? This question is crucial for many, as these conditions can significantly impact daily life and work performance. This guide explores the complexities of maintaining employment while living with fibromyalgia (FM) and chronic fatigue syndrome (CFS), providing insights into understanding these conditions, exploring work options, managing symptoms, and…
Painkiller Withdrawal Chronic Pain A Deep Dive
Painkiller withdrawal chronic pain sets the stage for this exploration, delving into the complex interplay of chronic pain, opioid use, and the challenges of withdrawal. This journey navigates the science behind chronic pain, from its various types and causes to the physiological effects of painkillers. We’ll also examine the often-overlooked aspects of withdrawal, from the…
Celebrex vs Ibuprofen Which Pain Reliever?
Celebrex vs ibuprofen how to decide which you should use – Celebrex vs ibuprofen: how to decide which you should use. Choosing between these common pain relievers can be tricky. Both ibuprofen and celecoxib are effective, but they work differently in the body and have varying side effects. This guide will walk you through the…
Skin Pain in Psoriasis A Deep Dive
Skin pain in psoriasis is a significant concern for many sufferers, impacting their daily lives and overall well-being. This detailed exploration delves into the various types of pain, their mechanisms, and the factors that exacerbate them. We’ll also examine the profound impact on daily routines, mental health, and social interactions. Further, we’ll discuss diagnosis, management…
Steroid Injections Chronic Back Pain A Deep Dive
Steroid injections chronic back pain are a potential treatment option, but understanding the specifics is crucial. This in-depth look explores the mechanics, efficacy, procedures, patient considerations, and alternatives to help you make informed decisions. We’ll cover everything from the different injection types and their mechanisms of action to the potential risks and long-term management strategies….