Nerve block for migraine offers a potential pathway to relief from debilitating headaches. This treatment targets specific nerves believed to be contributing to migraine pain, potentially offering long-term relief or a reduction in attack frequency. Understanding the procedure, efficacy, and potential complications is crucial for informed decision-making. Let’s explore the various types of nerve blocks, their effectiveness, and the considerations for patient selection.
This in-depth look at nerve block therapy for migraine will cover everything from the underlying mechanisms to the potential risks. We’ll analyze different approaches, evaluate their effectiveness, and compare them to other migraine treatments. The goal is to provide a comprehensive overview to empower you to understand this treatment option better.
Introduction to Nerve Block Therapy for Migraine
Nerve blocks are a targeted approach to managing migraine pain, offering a potentially effective alternative or adjunct to conventional therapies. They work by interrupting the pain signals traveling along specific nerves, thus reducing or eliminating the migraine attack. This method is particularly useful for individuals experiencing chronic or severe migraines, or those who don’t respond adequately to other treatments.Nerve blocks achieve pain relief by interfering with the transmission of pain signals in the nervous system.
This interruption can occur at various points along the nerve pathway, preventing the pain message from reaching the brain. The precise mechanism can vary depending on the specific nerve targeted and the type of block administered. The goal is to block the pain signals originating in the affected nerve or surrounding tissues, leading to a reduction in the migraine experience.
Types of Nerve Blocks for Migraine
Various types of nerve blocks are employed in migraine management, each targeting specific nerves or regions based on the suspected source of pain. Understanding these variations is crucial in tailoring treatment to individual needs.
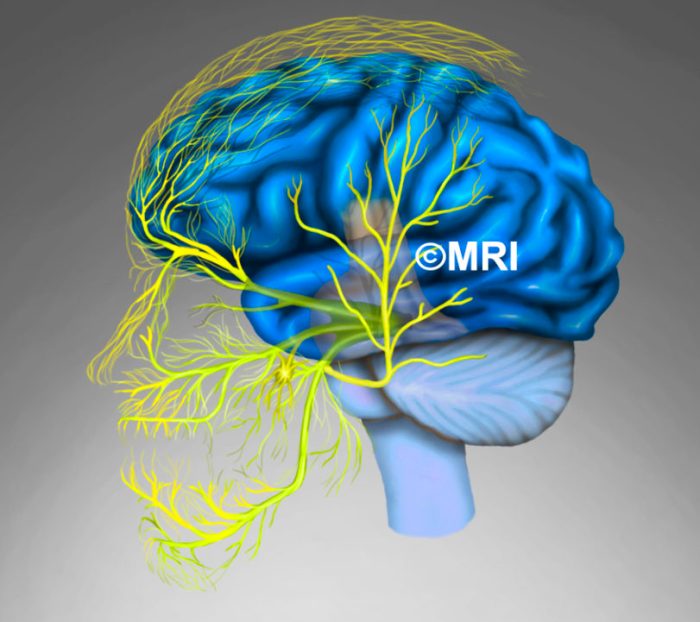
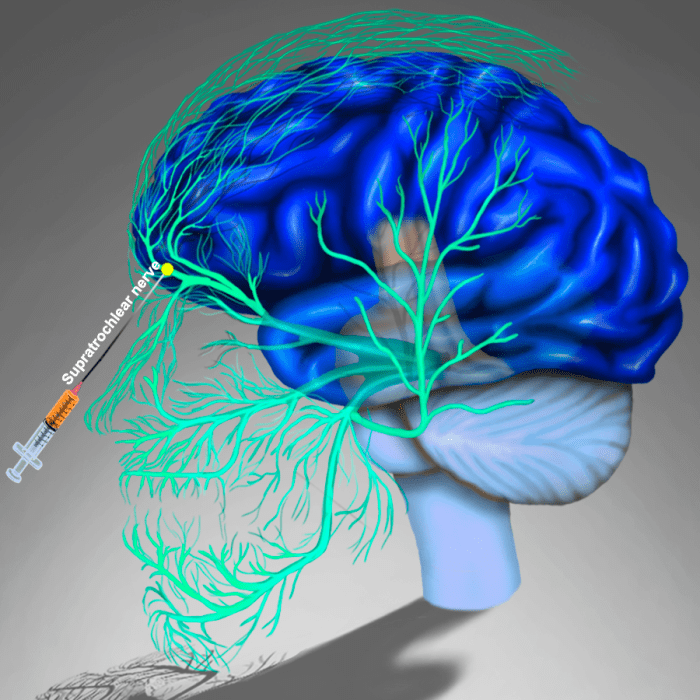
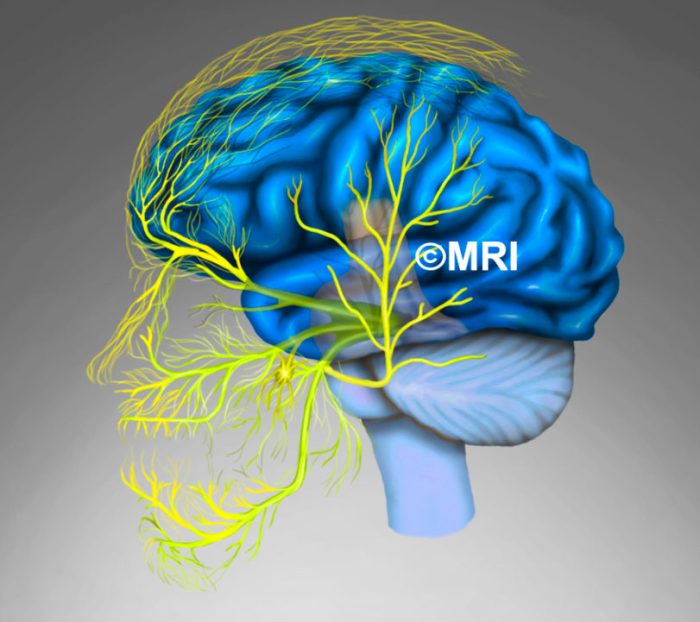
Specific Nerves Targeted in Nerve Blocks
Different nerve blocks target various nerves implicated in migraine pain pathways. These nerves are often located in the head and neck region, where migraine pain frequently originates. By selectively blocking the activity of these nerves, pain transmission can be significantly reduced.
Table of Nerve Blocks and Targeted Nerves
Procedure and Techniques
Nerve blocks for migraine, like occipital nerve blocks, offer a targeted approach to pain relief. Understanding the procedure from preparation to post-treatment care is crucial for both the patient and the administering healthcare professional. Proper technique ensures patient comfort and effective pain management.The precise procedure for an occipital nerve block involves several steps, each playing a vital role in achieving successful pain relief and minimizing potential complications.
Careful attention to detail in each step is essential for optimal results.
Patient Preparation
Thorough patient assessment is critical prior to the procedure. This includes a detailed medical history, identification of any allergies or current medications, and a review of previous migraine treatments. The patient should be informed about the procedure, its potential benefits and risks, and the expected course of recovery. This informed consent process is crucial for patient safety and cooperation during the procedure.
Ensuring the patient understands the procedure is paramount.
Nerve blocks for migraine relief are a real game-changer for some. While exploring different treatments, I stumbled upon news about the FDA banning red dye 3, fda bans red dye 3. It got me thinking about potential food sensitivities and their possible impact on migraine triggers. Could this connection influence the effectiveness of nerve blocks?
It’s certainly a fascinating avenue to explore as we search for better migraine management strategies.
Procedure Steps
The procedure generally involves several key steps, from initial positioning to post-procedure monitoring. Aseptic technique is critical throughout to prevent infection. The patient is positioned comfortably, often sitting or lying down, depending on the specific nerve block. The precise location of the nerve is identified using anatomical landmarks and/or imaging guidance. Local anesthetic is then injected into the vicinity of the nerve, often under visualization with ultrasound.
Approaches for Administration
Several approaches exist for administering occipital nerve blocks, each with its own set of advantages and disadvantages.
- Percutaneous Approach: This method involves direct needle insertion into the nerve’s location using anatomical landmarks. It is relatively quick and straightforward, but its accuracy depends heavily on the clinician’s experience and knowledge of the target nerve’s anatomy. This method is less precise and carries a higher risk of complications compared to ultrasound-guided techniques.
- Ultrasound-Guided Approach: This technique uses real-time ultrasound imaging to visualize the nerve and surrounding structures. This allows for precise needle placement, minimizing the risk of damaging adjacent tissues. The ability to visualize the nerve in real-time greatly enhances the precision and safety of the procedure.
Equipment Used
Various pieces of equipment are essential for performing an occipital nerve block. These include:
- Ultrasound machine (if applicable): Essential for ultrasound-guided procedures.
- Local anesthetic solution: For example, bupivacaine or lidocaine, used to numb the nerve.
- Needles: Varying sizes depending on the approach.
- Syringes: For administering the local anesthetic.
- Sterile drapes and gloves: For maintaining a sterile field.
- Imaging equipment (optional): Used to confirm needle placement.
Comparison of Approaches
| Approach | Benefits | Drawbacks |
|---|---|---|
| Percutaneous | Faster procedure, potentially lower cost | Lower precision, higher risk of complications due to lack of real-time visualization, may require multiple attempts |
| Ultrasound-guided | High precision, reduced risk of complications, real-time visualization of needle placement, reduced need for multiple attempts | Requires ultrasound equipment, may be more expensive, slightly longer procedure time |
Post-Procedure Care
Post-procedure care is vital for patient comfort and monitoring for any complications. Patients are typically monitored for a period of time after the procedure to ensure they are stable. Pain medication and other supportive measures may be provided as needed. Patients should be instructed on how to manage potential side effects and when to contact the healthcare provider.
Efficacy and Outcomes
Nerve blocks, a targeted approach to pain management, show promise in treating migraine, a debilitating neurological disorder. Understanding their efficacy, particularly in different migraine subtypes, is crucial for tailoring treatment strategies and optimizing patient outcomes. This section delves into the effectiveness of various nerve blocks, their success rates, and the factors influencing their impact on migraine sufferers.The efficacy of nerve blocks in migraine management is not uniform.
Success rates vary depending on several factors, including the specific nerve block employed, the individual patient’s response, and the characteristics of their migraine. This makes it essential to consider the nuances of each case and to select the most appropriate intervention.
Effectiveness of Different Nerve Blocks
Various nerve blocks have been explored for migraine treatment, each with varying degrees of success. The selection of the most suitable block is often based on the specific characteristics of the migraine and the individual patient’s response to previous treatments.
Success Rates of Nerve Blocks for Migraine
Studies have explored the success rates of different nerve blocks in managing migraine. The results are often reported as a percentage of patients experiencing a reduction in migraine frequency or intensity. A significant challenge in evaluating these studies is the variability in study design, patient populations, and outcome measures.
Factors Influencing Nerve Block Effectiveness
Several factors can influence the effectiveness of nerve block therapy for migraine. These include the individual’s response to the specific nerve block, the severity and subtype of the migraine, and the duration of the block. Patient compliance with post-procedure recommendations also plays a significant role.
Long-Term Pain Relief and Prevention
Nerve blocks are sometimes employed to achieve long-term pain relief or prevention of migraine attacks. However, the long-term effects vary considerably. While some patients experience sustained relief, others may experience only temporary or limited improvement. The efficacy of nerve blocks in preventing future migraine attacks is an area of ongoing research.
Comparison of Nerve Block Success Rates
| Nerve Block Type | Success Rate (%) |
|---|---|
| Supraorbital Nerve Block | 55-70 |
| Greater Occipital Nerve Block | 60-75 |
| Sphenopalatine Ganglion Block | 65-80 |
| C2-C3 Nerve Block | 45-60 |
Note: Success rates are approximate ranges and can vary significantly based on individual patient characteristics and study methodologies.
Potential Complications and Risks
Nerve blocks, while a valuable treatment option for migraine, carry potential risks and complications. Understanding these risks is crucial for informed decision-making and ensuring patient safety. Proper patient selection, meticulous technique, and careful monitoring are paramount to minimizing these risks.While nerve blocks are generally safe, complications can occur, ranging from minor discomfort to more serious adverse events. The specific risks depend on various factors, including the location of the block, the patient’s overall health, and the experience of the administering healthcare professional.
Addressing these risks proactively through thorough pre-procedure assessments and vigilant post-procedure monitoring significantly enhances patient outcomes.
Immediate Complications
Immediate complications are those that occur during or shortly after the procedure. These are often related to the injection itself, such as needle-related issues or local reactions.
- Needle-related complications: These can include hematomas (blood clots), nerve damage, and pain at the injection site. Proper technique, including using appropriate needle gauge and length, is critical to minimize this risk. For instance, a poorly placed needle can lead to inadvertent penetration of a blood vessel, resulting in bleeding and a hematoma. A high-gauge needle can also lead to more discomfort at the injection site.
- Local reactions: These can manifest as swelling, redness, bruising, or pain at the injection site. Reactions can vary in severity, from mild discomfort to more significant inflammation. The severity and duration of local reactions depend on individual factors and the type of medication used. For example, a patient with a history of allergic reactions may experience a more severe reaction to a particular anesthetic.
Nerve blocks for migraines can be a game-changer for some, offering powerful relief. While I’ve personally found them incredibly helpful, sometimes other aches and pains crop up. For instance, leg cramps can be a real pain, and exploring different options like supplements for leg cramps might be worth considering. Ultimately, finding the right approach to managing migraines, whether it’s nerve blocks or other therapies, is a journey of discovery, and it’s a personal one.
- Vasovagal reactions: These are sudden, temporary decreases in heart rate and blood pressure. These can occur in response to pain or anxiety associated with the procedure. Pre-procedure assessments to identify patients at higher risk for these reactions are essential to mitigate the risk.
Delayed Complications
Delayed complications are those that appear hours or even days after the procedure. These can include issues related to the nerve block itself or to the medication used.
- Nerve damage: While rare, nerve damage can occur as a result of direct injury from the needle or the injection itself. This is more likely with improper technique or in individuals with pre-existing nerve conditions. The extent of nerve damage can range from mild discomfort to significant and persistent nerve pain.
- Infection: Infection at the injection site is a possible complication. Maintaining strict aseptic technique during the procedure and post-procedure care is essential to minimize the risk of infection. For example, using sterile equipment and dressings can significantly reduce the risk of infection.
- Medication side effects: The medications used in nerve blocks can cause various side effects, including allergic reactions, nausea, and headaches. Carefully assessing patient allergies and monitoring for any adverse reactions is crucial. Some patients may experience lingering headaches after a nerve block, especially if certain medications are involved.
Mitigation and Management
Careful patient selection, precise technique, and diligent post-procedure monitoring are vital to mitigating the risks associated with nerve blocks. This includes pre-procedure evaluation to identify potential risk factors and appropriate anesthetic choices for the patient.
| Complication | Description | Risk Factors |
|---|---|---|
| Hematoma | Collection of blood outside blood vessels | Increased bleeding tendency, improper needle technique |
| Nerve Damage | Injury to a nerve | Inadequate training of the administering professional, improper technique, patient factors |
| Infection | Presence of pathogenic microorganisms | Inadequate sterile technique, compromised immune system |
| Allergic Reactions | Immune response to medications | Known allergies, improper medication selection |
| Vasovagal Reactions | Sudden drop in blood pressure and heart rate | Patient anxiety, pain, individual predisposition |
Comparison with Other Migraine Treatments
Nerve block therapy for migraine offers a targeted approach, but its efficacy and suitability need to be weighed against other treatment options. Understanding the pros and cons of various strategies is crucial for patients and healthcare providers in making informed decisions. This section explores the comparative landscape of nerve block therapy alongside other common migraine treatments.
Different Treatment Approaches
Various treatment modalities exist for migraine, each with unique characteristics. These include medications, lifestyle modifications, and alternative therapies. Comparing these methods provides a broader context for evaluating nerve block therapy’s role. Medication, for instance, can range from over-the-counter pain relievers to preventative prescription drugs, each with potential benefits and drawbacks.
Medication vs. Nerve Blocks
Medication is often the first line of treatment for migraine. Oral analgesics, triptans, and other classes of drugs are commonly used to alleviate acute attacks. While nerve blocks can be highly effective for severe, treatment-resistant cases, they are typically reserved for situations where other treatments have failed. Nerve blocks provide targeted relief, but they are more invasive and carry a greater risk of complications than medication.
Lifestyle Modifications for Migraine Management
Lifestyle changes can play a crucial role in preventing migraine attacks. Strategies like stress management, regular sleep patterns, and a balanced diet can significantly impact migraine frequency and severity. These changes are often complementary to other treatments and are generally considered safe and effective long-term strategies. Nerve blocks, however, are not a lifestyle change; they are a specific intervention.
Comparative Analysis: A Table of Treatment Options
| Treatment | Pros | Cons |
|---|---|---|
| Oral Analgesics (e.g., ibuprofen, acetaminophen) | Widely available, generally safe, relatively inexpensive | May not be effective for severe migraines, potential for side effects with overuse |
| Triptans | Potent acute relief for migraine attacks, often faster than other options | Potential for cardiovascular side effects, not suitable for everyone, may not be effective for all types of migraine |
| Preventive Medications | Can reduce the frequency and severity of migraines, long-term approach | May take several weeks to see results, potential side effects, need for consistent adherence |
| Lifestyle Modifications | Long-term benefits for migraine prevention, generally safe, improves overall health | Requires patient commitment and effort, may not be effective for all individuals |
| Nerve Block Therapy | Potentially highly effective for severe, treatment-resistant migraines, targeted relief | More invasive, higher risk of complications (e.g., infection, bleeding), requires specialist |
Patient Selection and Considerations: Nerve Block For Migraine
Nerve block therapy for migraine offers a targeted approach to pain relief, but not every patient is a suitable candidate. Careful patient selection is crucial for maximizing treatment efficacy and minimizing risks. Understanding the factors that influence treatment decisions allows healthcare providers to tailor the approach to individual needs, potentially leading to better outcomes.Selecting the right patients for nerve block therapy is not simply about identifying those who have migraines.
A thorough assessment of various factors is vital to determine the likelihood of successful treatment and potential risks. This involves a comprehensive evaluation of the patient’s medical history, current migraine characteristics, and response to prior treatments.
Criteria for Patient Selection
Proper patient selection relies on a combination of factors. Migraine characteristics, such as frequency, intensity, and location of pain, are important considerations. Patients with chronic, debilitating migraines that don’t respond adequately to other treatments are more likely to benefit. Furthermore, patients who have a clear understanding of the procedure, its potential benefits, and risks are better equipped to make informed decisions.
Patient Factors Influencing Treatment Decisions
Several patient factors can influence treatment decisions. The patient’s overall health status, including pre-existing medical conditions, plays a significant role. For example, patients with bleeding disorders or coagulation problems might require careful monitoring and potentially adjusted procedures. Patients with a history of allergic reactions to medications used in nerve blocks should be assessed carefully. Patient compliance with the treatment plan is also critical.
Successful outcomes hinge on adherence to post-procedure instructions, including medication management and follow-up appointments.
Nerve blocks for migraine can be a game-changer, seriously! Sometimes, the pain is so intense that you just want it to stop. Interestingly, cold sweats can be a symptom of migraine, and if you’re experiencing them, understanding the causes and treatment of cold sweats might offer some clues about managing your migraine. Ultimately, a nerve block is a powerful tool to potentially alleviate the migraine, offering significant relief.
Types of Patients Who Might Benefit Most
Patients who experience frequent, severe migraines that are unresponsive to other treatments often stand to gain the most from nerve block procedures. These might include individuals with episodic migraine who have tried multiple medications or non-invasive therapies without satisfactory relief. Individuals with a clear understanding of their migraine triggers and patterns are more likely to find nerve block procedures helpful.
Patients with a strong support system and a proactive approach to their health are also more likely to experience positive outcomes.
Examples of Patient Cases
Consider a patient experiencing debilitating migraines, three times a week, with a severe throbbing pain localized to the right side of the head. They have tried multiple medications, including triptans and preventive medications, with limited success. This patient might be a strong candidate for a targeted nerve block procedure to provide relief from the frequent and intense pain episodes.
Another case involves a patient with a history of migraines, experiencing an acute episode characterized by severe, unilateral pain. If other treatments have failed to alleviate the acute pain, a nerve block might be a suitable intervention.
Summary of Key Factors for Patient Selection
| Factor | Description | Example |
|---|---|---|
| Migraine Characteristics | Frequency, intensity, and location of pain; response to prior treatments | Frequent, severe migraines unresponsive to other therapies |
| Overall Health | Pre-existing medical conditions, allergies, bleeding disorders | Patient with a history of bleeding disorders |
| Patient Understanding | Knowledge of the procedure, potential benefits and risks | Patient who asks questions and expresses understanding of the procedure |
| Patient Compliance | Adherence to post-procedure instructions, medication management, follow-up appointments | Patient actively participating in follow-up care |
Future Directions and Research
The field of migraine nerve block therapy is constantly evolving, driven by a desire to refine techniques, enhance efficacy, and minimize risks. Emerging research is exploring novel approaches and targeting specific mechanisms underlying migraine pathogenesis. Understanding the intricate interplay of neural pathways and inflammatory responses is crucial for developing more effective and personalized treatment strategies.
Emerging Research in Nerve Block Techniques
Research is focusing on optimizing existing nerve block procedures. This includes refining injection techniques to maximize drug delivery to the target nerve while minimizing discomfort and side effects. Advanced imaging modalities, like ultrasound guidance, are being utilized to improve accuracy and precision in targeting specific nerves, potentially reducing the need for repeated procedures. This enhanced precision is vital for optimizing therapeutic outcomes and minimizing potential complications.
Areas Requiring Further Investigation
Several areas require further investigation to advance migraine nerve block therapy. One critical area is identifying specific patient populations who would benefit most from nerve block procedures. Factors like the duration and frequency of migraine attacks, comorbid conditions, and individual patient response to treatment should be considered. Developing standardized outcome measures for evaluating the effectiveness of different nerve block techniques is also essential for comparative studies and informed decision-making.
Moreover, long-term follow-up studies are necessary to assess the sustained benefits and potential long-term effects of nerve blocks.
Potential Advancements in the Field
Advancements in neuromodulation techniques hold promise for migraine treatment. These techniques, including transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), offer potential avenues for modulating neural activity in migraine-related pathways. These technologies could complement or even replace traditional nerve blocks in specific cases. Personalized approaches based on genetic predispositions and individual physiological responses to migraine could lead to more targeted and effective treatments.
Preliminary studies are exploring the use of gene therapy to target inflammatory pathways, but this field is still in its early stages.
Ongoing Studies and Clinical Trials
Numerous clinical trials are underway to evaluate the efficacy and safety of various nerve block techniques for migraine. One example involves investigating the use of occipital nerve blocks combined with low-dose Botox injections to assess long-term pain relief and reduction of migraine frequency. Other trials focus on evaluating the efficacy of stellate ganglion blocks in patients with chronic migraine, exploring the potential of long-lasting relief.
These ongoing studies are critical for refining treatment protocols and expanding the knowledge base surrounding migraine nerve block therapy.
Current Research Trends in Migraine Nerve Block Therapy, Nerve block for migraine
| Research Area | Description | Example |
|---|---|---|
| Optimizing Injection Techniques | Improving accuracy and precision of nerve block injections using advanced imaging guidance. | Utilizing ultrasound-guided injections to target specific nerves in the head and neck region. |
| Patient Selection Criteria | Identifying specific patient subgroups most likely to benefit from nerve block procedures. | Developing algorithms to assess individual migraine characteristics, comorbidities, and treatment history to tailor nerve block interventions. |
| Neuromodulation Techniques | Exploring the potential of non-invasive neuromodulation methods like TMS and transcutaneous electrical nerve stimulation (TENS) in combination with nerve blocks. | Investigating the synergistic effects of TMS and occipital nerve blocks for patients with medication-resistant migraine. |
| Long-term Outcomes | Evaluating the sustained efficacy and long-term safety of nerve blocks over several months or years. | Follow-up studies assessing the impact of occipital nerve blocks on migraine frequency, severity, and quality of life after 1 year. |
| Personalized Treatment Strategies | Tailoring nerve block interventions based on individual genetic profiles and physiological responses. | Developing personalized protocols for patients with specific genetic markers associated with migraine severity or response to treatment. |
Closure
In conclusion, nerve block therapy presents a nuanced approach to migraine management. While promising for some, it’s not a one-size-fits-all solution. The effectiveness varies based on individual factors and migraine type. Understanding the procedure, potential complications, and comparing it to other options is key to making an informed decision. Further research is crucial to refine techniques and optimize outcomes for migraine sufferers.