What are neutrophils p2? This exploration delves into the crucial role of neutrophils, a type of white blood cell, within the context of P2. We’ll uncover their significance in the immune system, examining their structure, function, and behavior in a P2 environment. From the intricacies of their normal function to their response in P2 conditions, this detailed overview will reveal the importance of understanding neutrophil activity in various contexts.
Neutrophils, the body’s first responders to infection, play a vital role in the immune system. Their presence is crucial for maintaining health, and any abnormalities in their function or numbers can have significant implications. This detailed look at neutrophils in P2 conditions will cover the nuances of how these cells behave in this particular environment.
Neutrophils: The Body’s First Line of Defense
Neutrophils are a crucial component of the innate immune system, playing a vital role in the body’s defense against invading pathogens. They are the most abundant type of white blood cell, making up a significant portion of the circulating leukocytes. Their rapid response and potent antimicrobial capabilities are essential for combating infections. They are often the first responders to sites of inflammation and infection.
Defining Neutrophils
Neutrophils are a type of granulocyte, a category of white blood cells characterized by the presence of granules in their cytoplasm. These granules contain enzymes and antimicrobial substances that are crucial for their function. Their primary role is to engulf and destroy pathogens through a process called phagocytosis. This process involves the neutrophil extending pseudopods to surround the pathogen, engulfing it within a vacuole, and then releasing the granules to destroy it.
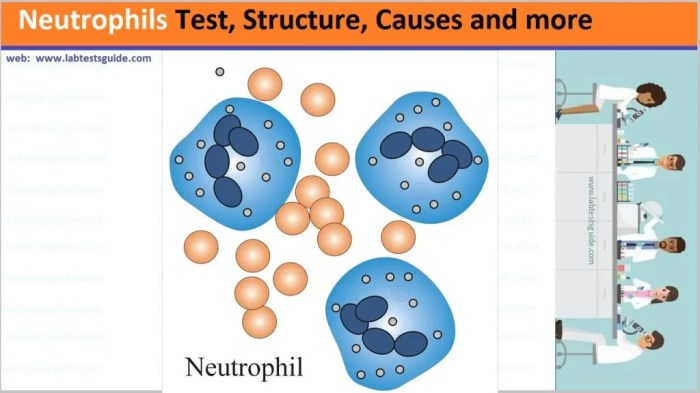
Neutrophil Structure and Morphology
Neutrophils are typically spherical or slightly irregular in shape. Their cytoplasm contains numerous granules that stain with neutral dyes, hence the name. These granules contain various enzymes, proteins, and antimicrobial substances. The nucleus of a neutrophil is segmented into 2 to 5 lobes, connected by thin filaments. This segmented appearance is characteristic of mature neutrophils.
The specific appearance of the nucleus and granules is crucial in identifying neutrophils under a microscope.
Types of Neutrophils (Granulocytes)
While neutrophils are classified as a single cell type, variations in the staining characteristics and maturity of their granules can be observed. These differences are primarily due to the various stages of neutrophil development and maturation. There isn’t a strict categorization into different types. Instead, the focus is on the maturity levels and the contents of the granules.
Normal Range of Neutrophils
The normal range for neutrophils in the blood is typically between 1,500 and 8,000 per microliter of blood. Variations can occur based on factors such as age, health status, and recent infections. A significant deviation from this range can indicate various underlying health conditions.
Key Features of Neutrophils
| Feature | Description | Image Description | Additional Notes |
|---|---|---|---|
| Structure | Neutrophils are granulocytes with a multi-lobed nucleus and cytoplasmic granules. The granules contain enzymes and antimicrobial proteins. The nucleus typically has 2-5 lobes. | A diagram showing a neutrophil with its segmented nucleus and cytoplasmic granules would be helpful here. | The segmented nucleus is a hallmark of mature neutrophils. |
| Function | Neutrophils are phagocytic cells, engulfing and destroying pathogens like bacteria and fungi. They release antimicrobial substances from their granules to kill ingested pathogens. They are a key component of the innate immune system. | A diagram depicting phagocytosis by a neutrophil would be beneficial. | Their rapid response and potent antimicrobial abilities are essential for fighting infections. |
Neutrophils in P2 Context
Neutrophils, the body’s first responders in the immune system, play a crucial role in combating infections. Understanding their behavior in specific contexts, like a P2 condition, is vital for accurate diagnosis and effective treatment. This exploration delves into the significance of neutrophils in a P2 context, focusing on potential causes for elevated or decreased counts, and the clinical implications of these variations.Elevated or decreased neutrophil counts in a P2 context can signal underlying issues.
A detailed analysis of these changes, coupled with other diagnostic tests, helps clinicians tailor treatment plans to address the specific needs of the patient. This section also compares neutrophil response in a P2 condition to typical immune responses, highlighting the nuanced differences that can arise in specific disease states.
Significance of Neutrophils in P2
Neutrophils are essential components of the innate immune system, rapidly mobilizing to sites of infection or tissue damage. Their primary function is phagocytosis, engulfing and destroying pathogens. In a P2 context, the significance of neutrophils is amplified due to the complex interplay of immune cells and potential inflammatory processes characteristic of this condition. This can result in either an enhanced or suppressed neutrophil response, impacting the body’s ability to fight off infections or heal injuries.
Potential Reasons for Elevated Neutrophils in P2
Elevated neutrophil counts, known as neutrophilia, in a P2 context may stem from several factors. Bacterial infections, inflammation, and certain medications are common causes. Acute stress responses can also lead to temporary increases in neutrophil counts. In a P2 setting, this could be linked to inflammatory processes or complications associated with the underlying disease. Additionally, some autoimmune diseases can result in increased neutrophil production.
Precise diagnosis necessitates considering the patient’s medical history, symptoms, and results from other tests.
Potential Reasons for Decreased Neutrophils in P2
Decreased neutrophil counts, or neutropenia, in a P2 context can arise from various factors. Bone marrow disorders, chemotherapy, certain infections, and autoimmune diseases can all contribute to reduced neutrophil production or increased destruction. In a P2 context, the underlying disease or its treatment could be suppressing the bone marrow’s ability to produce neutrophils. Severe infections, particularly those involving sepsis, can also cause neutropenia.
This decrease can significantly compromise the body’s ability to fight infection.
Clinical Implications of Neutrophil Abnormalities in P2
Neutrophil abnormalities in a P2 context can have significant clinical implications. Elevated neutrophil counts might indicate an active infection or inflammatory process, potentially requiring targeted antibiotic or anti-inflammatory therapies. Conversely, decreased counts can increase susceptibility to infections, necessitating careful monitoring and prophylactic measures to prevent serious complications. Monitoring neutrophil counts is crucial in managing P2 patients, as it provides valuable insights into the disease’s progression and the effectiveness of treatment.
Comparison of Neutrophil Response in P2 to Other Immune Responses
The neutrophil response in a P2 condition often differs from responses seen in other immune situations. For example, in a typical bacterial infection, a rapid and robust neutrophil influx is observed. In a P2 context, the response might be delayed, or less pronounced due to the underlying condition’s impact on immune cell function. The specific interplay of various immune cells in P2 conditions influences the overall inflammatory response, which in turn affects the neutrophil response.
This nuanced difference necessitates a tailored approach to diagnosis and treatment.
Comparison of Neutrophil Function in Normal vs. P2 Conditions
| Condition | Normal Neutrophil Function | Neutrophil Function in P2 | Comparison |
|---|---|---|---|
| Healthy State | Rapidly recruited to sites of infection or tissue damage; efficiently phagocytize and destroy pathogens; participate in tissue repair. | Recruitment and function may be altered by the underlying P2 condition; potential for impaired phagocytosis or reduced efficiency in pathogen destruction; involvement in the complex inflammatory response within P2. | Neutrophils are still present but their function and response may be affected. |
| P2 Condition | (N/A) | Function can be altered depending on the specific P2 condition. For example, in certain P2 conditions, neutrophils may be dysfunctional or have reduced mobility. | Neutrophil response is impacted by the specific P2 context, potentially leading to altered function and effectiveness. |
Diagnostic Procedures
Understanding neutrophil levels is crucial for diagnosing and managing various health conditions. Accurate assessment relies on a combination of diagnostic procedures that measure neutrophil counts and evaluate their characteristics. These procedures provide valuable insights into the body’s immune response and potential underlying diseases.Neutrophils, as the body’s first responders to infection, play a critical role in the immune system.
Neutrophils, specifically p2, are a fascinating type of white blood cell. They play a crucial role in our immune system, but recent research is exploring their potential connection to various health conditions, including the increased risk of fatty liver disease, particularly during menopause. Understanding the relationship between neutrophils p2 and menopause fatty liver disease risk is a crucial step in developing preventative strategies.
Further research is needed to fully understand the complex interplay between these factors and the implications for overall health.
Anomalies in their count or function can indicate a wide range of issues, from mild infections to more serious conditions. Diagnostic tests are essential for identifying these anomalies and guiding appropriate treatment strategies.
Complete Blood Count (CBC)
The complete blood count (CBC) is a fundamental diagnostic test for evaluating blood cell counts, including neutrophils. It provides a comprehensive overview of the cellular components of the blood, offering a baseline assessment of overall health. The CBC measures the number of various blood cells, including red blood cells, white blood cells (like neutrophils), and platelets. Variations in these counts can indicate a variety of conditions.
Peripheral Blood Smear
A peripheral blood smear is a microscopic examination of a blood sample. It allows for a visual assessment of the morphology (shape and structure) of blood cells, including neutrophils. This visual analysis can detect abnormalities in neutrophil size, shape, and granulation patterns, providing insights beyond simple numerical counts. These observations can help differentiate between various types of infections or inflammatory conditions.
Neutrophil Count Measurement
Neutrophil counts are typically determined as part of a complete blood count (CBC). Automated hematology analyzers are widely used for this purpose. These instruments use optical or electrical impedance methods to detect and quantify different blood cell types. The instruments process blood samples quickly and accurately, providing results within minutes. Manual counting methods are less common now but remain important in research and quality control.
Interpreting Neutrophil Count Results
Interpreting neutrophil count results requires considering the context of other clinical findings and the patient’s overall health status. A normal neutrophil count (typically in the range of 1500 to 8000 cells/µL) indicates a healthy immune response. However, deviations from this range can signal various conditions. For instance, an elevated neutrophil count (neutrophilia) may suggest an infection, inflammation, or other conditions.
Conversely, a decreased neutrophil count (neutropenia) may indicate bone marrow disorders, certain medications, or severe infections.
Neutrophils, crucial components of our immune system, are a fascinating part of the body’s defense mechanisms. Understanding their role is key to overall health. While neutrophils are important for fighting infection, if you’re dealing with a peptic ulcer, it’s vital to consider what you eat; a balanced diet, including specific foods, is often recommended for healing. For more information on what foods to include or avoid, check out this helpful guide on what can i eat if i have a peptic ulcer.
Ultimately, neutrophils and a healthy diet go hand-in-hand for a robust immune response.
Summary of Diagnostic Tests for Neutrophils in P2
| Test | Method | Interpretation | Clinical Significance |
|---|---|---|---|
| Complete Blood Count (CBC) | Automated hematology analyzers measure different blood cell types, including neutrophils, using optical or electrical impedance methods. | Normal neutrophil count (1500-8000 cells/µL) suggests a healthy immune response. Elevated counts (neutrophilia) may indicate infection or inflammation. Decreased counts (neutropenia) may suggest bone marrow disorders or severe infections. | Provides a broad overview of blood cell counts, including neutrophils, for evaluating overall health and identifying potential abnormalities. |
| Peripheral Blood Smear | Microscopic examination of a blood sample to assess the morphology (shape and structure) of blood cells, including neutrophils. | Visual assessment of neutrophil size, shape, and granulation patterns can identify abnormalities indicative of various conditions. | Provides detailed information about neutrophil morphology, aiding in the differentiation of conditions and guiding further investigations. |
Treatment and Management
Treating conditions involving neutrophil abnormalities in P2 requires a multifaceted approach, tailored to the specific cause and severity of the issue. Effective management focuses on addressing the underlying disease process while supporting neutrophil function and preventing complications. This involves a combination of pharmacological interventions, supportive care, and meticulous monitoring of neutrophil counts and function.
Treatment Strategies for Neutrophil Abnormalities
Different strategies are employed based on the specific cause of the neutrophil abnormality. For example, infections are treated with appropriate antibiotics, while autoimmune disorders might require immunosuppressants. Underlying hematological malignancies may necessitate chemotherapy or stem cell transplantation. A thorough evaluation of the patient’s medical history and a comprehensive diagnostic workup are crucial to determining the most suitable course of action.
Role of Medications in Managing Neutrophil Levels
Medications play a critical role in managing neutrophil levels, either by directly stimulating neutrophil production or by treating the underlying cause of the abnormality. Granulocyte colony-stimulating factor (G-CSF) is a frequently used medication that stimulates the bone marrow to produce more neutrophils. However, the use of such medications is not without potential side effects, which must be carefully considered in conjunction with the potential benefits.
Monitoring for these side effects is essential. Careful consideration of the risks and benefits is crucial when choosing specific medications.
Monitoring Neutrophil Counts During Treatment
Regular monitoring of neutrophil counts is essential during treatment. This allows clinicians to assess the effectiveness of the chosen strategy and promptly adjust treatment if necessary. Changes in neutrophil counts can indicate a response to therapy, the development of adverse effects, or the emergence of complications. Frequent blood tests are necessary to track neutrophil counts and ensure they remain within a healthy range.
Neutrophils P2 are a fascinating part of the immune system, but sometimes, health conditions like PCOS can throw things off balance. Finding ways to support overall health, like exploring inositol for PCOS info, inositol for pcos info can be beneficial. This, in turn, could potentially influence neutrophil function, but further research is needed to understand the specific connections.
Ultimately, understanding neutrophils P2 requires a deeper look into their role in the body’s defenses.
A consistent monitoring strategy is crucial for managing neutrophil disorders effectively.
Evaluating Treatment Efficacy on Neutrophil Function in P2
Evaluating the efficacy of treatment on neutrophil function in P2 goes beyond simply measuring absolute neutrophil counts. Assessing functional aspects, such as chemotaxis, phagocytosis, and oxidative burst, is crucial. Specialized laboratory tests are used to measure these aspects of neutrophil function. For example, the ability of neutrophils to migrate to sites of infection or engulf pathogens is assessed.
Results of these tests provide a more comprehensive understanding of how the treatment is impacting neutrophil function, allowing for more precise and effective management of the condition.
Illustrative Examples: What Are Neutrophils P2

Understanding the intricate relationship between neutrophils and P2 requires examining real-world scenarios. This section delves into case studies and hypothetical situations to illustrate the crucial role neutrophils play in P2, highlighting the importance of thorough neutrophil evaluation in diagnosis and management. These examples provide concrete insights into the complexities of this interaction.
A Case Study: Neutrophil Dysfunctional Response in P2
A 35-year-old male presented with symptoms consistent with P2. Blood tests revealed a reduced neutrophil count, a finding often observed in P2 cases. However, further analysis revealed a significant dysfunction in neutrophil chemotaxis, meaning the neutrophils were unable to effectively migrate to the site of infection or inflammation. This impaired response contributed to the prolonged and severe nature of the P2 presentation.
Treatment focused on addressing the underlying neutrophil dysfunction alongside standard P2 management protocols. The case underscores the importance of evaluating not just the neutrophil count, but also their functional capacity in P2 patients.
Fictional Scenario: Neutrophil-Mediated Inflammation in P2
Imagine a patient with a known history of P2 experiencing a severe respiratory infection. The inflammatory response, typically orchestrated by neutrophils, was significantly amplified in this case. This exaggerated inflammatory response, though crucial in fighting the infection, caused significant tissue damage in the lungs, hindering respiratory function. The patient’s neutrophils, while actively engaging in the inflammatory process, failed to effectively control the inflammation.
This scenario emphasizes the delicate balance needed between neutrophil-mediated immunity and tissue damage, particularly in the context of P2.
Neutrophil Role in P2-Associated Sepsis
Neutrophils are pivotal in combating bacterial infections, a common complication in P2. In a case of P2-associated sepsis, neutrophils are the first responders, rapidly migrating to the site of infection to engulf and destroy bacteria. Their efficiency in this process directly influences the patient’s outcome. A reduced or dysfunctional neutrophil response can lead to a more severe septic course, highlighting the critical role of neutrophils in preventing sepsis progression.
The ability of neutrophils to effectively eliminate bacteria and regulate inflammation is essential in preventing the escalation of sepsis.
Clinical Importance of Neutrophil Evaluation in P2, What are neutrophils p2
A 60-year-old female with a history of P2 presented with fever and malaise. Initial blood tests showed a normal white blood cell count, but further analysis of neutrophil subsets revealed a significant decrease in the proportion of mature neutrophils. This atypical neutrophil profile, while not immediately apparent from basic blood counts, strongly suggested a possible infection or exacerbation of P2.
Early identification of this pattern through thorough neutrophil evaluation allowed for prompt intervention, preventing the potential progression to a life-threatening condition. This case highlights the crucial role of a detailed neutrophil analysis in the timely diagnosis and management of P2 patients.
Importance of Thorough Neutrophil Examination in P2: A Case Study
A young adult with a newly diagnosed P2 was initially treated with standard protocols. However, the patient’s condition did not improve. A thorough examination of the neutrophils, including their morphology, function, and specific subsets, revealed an atypical pattern suggesting an underlying immune deficiency. This in-depth analysis led to the identification of a rare genetic condition interacting with P2.
This comprehensive examination allowed for a more targeted and effective treatment plan, leading to a positive outcome. This example demonstrates the vital role of a comprehensive neutrophil evaluation in identifying underlying conditions and tailoring treatment strategies in patients with P2.
Last Word
In summary, neutrophils p2 represent a critical aspect of understanding immune responses within the context of P2 conditions. We’ve explored their structure, function, diagnostic procedures, and treatment approaches. Understanding their behavior in P2 is essential for proper diagnosis and management. The importance of a thorough examination of neutrophils in P2 conditions cannot be overstated. Further research in this area is vital for advancements in healthcare.