What is a myotome? It’s a crucial concept in understanding how our muscles are controlled by the nervous system. Imagine a specific group of muscles, all working together, coordinated by a particular segment of the spinal cord. That’s essentially a myotome. This isn’t just an academic curiosity; myotome assessment plays a vital role in diagnosing neurological conditions.
From pinpointing the source of muscle weakness to understanding the intricate pathways of the nervous system, exploring myotomes reveals a fascinating interplay between structure and function.
This comprehensive guide delves into the world of myotomes, examining their definition, anatomy, function, clinical relevance, and assessment methods. We’ll uncover how these intricate muscle groups are organized, the role of nerve roots, and how evaluating myotomes helps diagnose and understand various neurological issues. Get ready to explore the fascinating science behind your body’s movement!
Definition and Scope
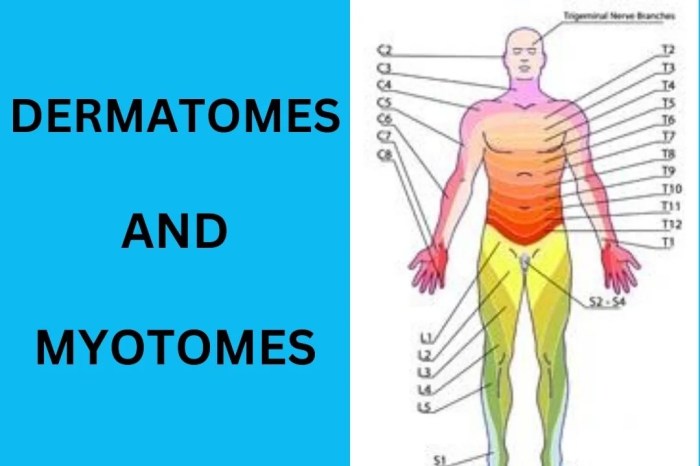
A myotome is a group of muscles innervated by a specific spinal nerve root. Understanding myotomes is crucial for clinicians, as they provide a pathway to assess the integrity of the motor pathways of the nervous system. It’s a fundamental concept in neurology, helping pinpoint the location of potential nerve damage.Myotomes and dermatomes, while both associated with spinal nerves, differ in their function.
Dermatomes map sensory innervation, while myotomes map motor innervation. Damage to a specific nerve root can manifest as weakness or paralysis in the associated myotome, allowing clinicians to pinpoint the affected area. This localized weakness helps determine the level of spinal cord or nerve root compromise.
Myotome Definition and Relationship to Dermatomes
A myotome is a group of muscles that are controlled by a single spinal nerve root. This contrasts with dermatomes, which map the sensory areas served by the same nerve root. The relationship between the two is based on the common spinal nerve root origin. Clinical correlation between sensory and motor deficits, observed in dermatomes and myotomes respectively, allows clinicians to pinpoint the affected spinal segment and the extent of the damage.
A myotome is basically a group of muscles that a single spinal nerve root controls. Understanding these muscle groups is crucial for diagnosing and treating pain, especially when considering active and passive pain management strategies. For example, if you’re experiencing pain in a specific area, evaluating the corresponding myotome can help pinpoint the source of the issue. This kind of assessment can help you determine the best course of action, such as exploring different approaches to pain relief, including active and passive pain management techniques.
Ultimately, knowing your myotomes can give you a better understanding of your body and how to manage any discomfort effectively.
This integrative approach is vital in diagnosing and treating various neurological conditions.
Clinical Significance of Myotomes
Myotomes are essential in clinical settings for diagnosing nerve root or spinal cord lesions. Weakness or paralysis in a specific myotome can indicate a problem with the corresponding spinal nerve root, often associated with conditions like herniated discs, spinal stenosis, or multiple sclerosis. The pattern of muscle weakness can help determine the precise location and extent of the neurological damage.
Description of Myotomes
Myotomes can be described in various ways. An anatomical description focuses on the specific muscles within the group. A functional description emphasizes the movements the myotome enables. Different methods of testing can also provide a detailed description, focusing on the specific movements and muscles involved in the examination. These methods are integral to the clinical evaluation.
Table of Myotomes
| Myotome Name | Associated Muscles | Nerve Root | Clinical Significance |
|---|---|---|---|
| Cervical Myotome C5 | Deltoid, biceps brachii, brachialis | C5 spinal nerve root | Weakness in shoulder abduction and elbow flexion can suggest C5 nerve root compression. |
| Cervical Myotome C6 | Biceps brachii, wrist extensors | C6 spinal nerve root | Weakness in wrist extension and elbow flexion indicates possible C6 nerve root impingement. |
| Lumbar Myotome L2 | Hip flexors | L2 spinal nerve root | Paralysis in hip flexion may point to L2 nerve root compression. |
| Lumbar Myotome L4 | Knee extensors | L4 spinal nerve root | Weakness in knee extension often suggests L4 nerve root damage, potentially due to disc herniation. |
| Sacral Myotome S1 | Plantar flexors, ankle evertors | S1 spinal nerve root | Weakness in plantar flexion and ankle eversion can indicate S1 nerve root pathology. |
Anatomy and Structure: What Is A Myotome
Myotomes are fascinating segments of the body, directly linked to the intricate network of nerves and muscles. Understanding their anatomical arrangement is crucial for diagnosing and treating neuromuscular disorders. This section delves into the detailed structure of myotomes, illustrating their organization and the specific components that contribute to their function.The arrangement of myotomes reflects the segmental organization of the nervous system.
They are essentially functional units, each controlled by a specific group of nerve roots. The specific muscles controlled by each myotome are essential in coordinating movement, posture, and other functions. This knowledge is fundamental in assessing neurological integrity.
Anatomical Arrangement of Myotomes, What is a myotome
The spinal cord segments and corresponding nerve roots organize myotomes in a precise pattern. Imagine a vertical arrangement of segments, each responsible for controlling muscles in a specific region of the body. This organization allows for precise control and coordination of movement, enabling us to perform a vast array of actions. This arrangement also allows for efficient communication between the brain and different parts of the body.
Components of a Myotome
A myotome comprises the nerve root(s) that innervate it and the specific muscle groups it controls. These components are interconnected, forming a functional unit. The nerve roots carry signals from the spinal cord to the muscles, enabling contraction and movement. The muscle groups are the effectors of this signal, performing the intended actions. Together, these elements create a complete functional unit.
Nerve Root Innervation
The nerve roots are the essential communication channels connecting the spinal cord to the muscles. Each myotome receives its innervation from specific nerve roots, which originate from the spinal cord. These nerve roots relay signals from the central nervous system to the muscle fibers, triggering contractions. The precise location of these roots is essential in determining the specific myotome.
Spinal Cord Segments Involved
The spinal cord is divided into segments, each corresponding to a specific region of the body. These segments are crucial in the formation of myotomes, as they are the source of the nerve roots. Each segment sends signals to the corresponding muscle groups, controlling their actions. The precise location and function of each spinal cord segment are essential in understanding myotome function.
This information is used to diagnose and treat various neuromuscular conditions.
Myotome Table
This table illustrates the relationship between myotome, nerve root(s), and the muscle groups controlled. It highlights the crucial role of nerve roots in activating specific muscle groups, which together create the function of a myotome. This information is critical in assessing neurological function and diagnosing neuromuscular disorders.
| Myotome | Nerve Root(s) Innervating It | Muscle Groups Controlled |
|---|---|---|
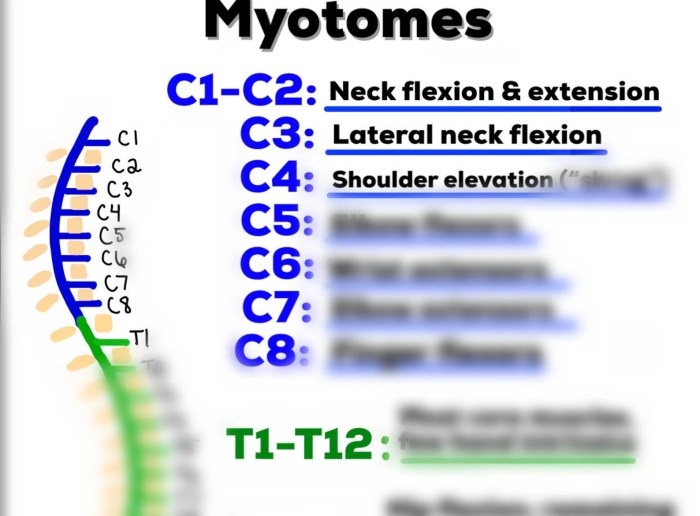
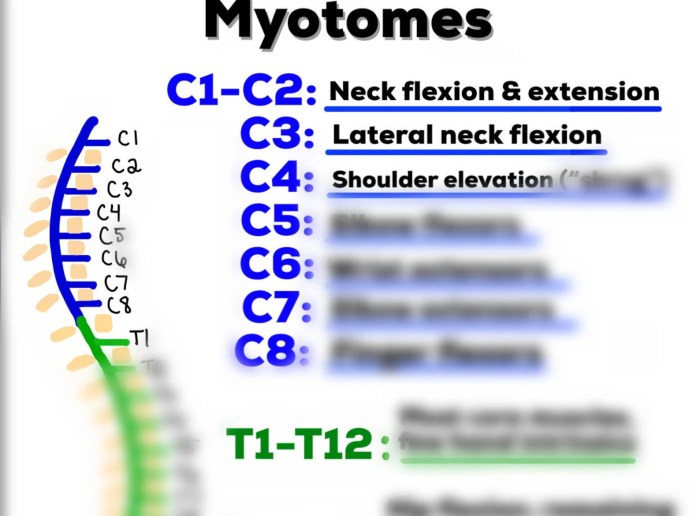
| Cervical Myotomes (C1-C8) | C1-C8 | Neck, shoulder, arm, hand muscles |
| Thoracic Myotomes (T1-T12) | T1-T12 | Intercostal muscles, back muscles |
| Lumbar Myotomes (L1-L5) | L1-L5 | Hip, thigh, knee muscles |
| Sacral Myotomes (S1-S5) | S1-S5 | Leg, foot muscles |
Neural Pathways Involved in Myotome Function
The neural pathways involved in myotome function are complex, but they can be described as follows. Sensory input from the muscle and surrounding tissues is conveyed to the spinal cord through sensory nerves. Motor commands are then sent from the spinal cord via motor nerves to the muscle fibers. This two-way communication allows for precise control and coordination of movement.
The intricate nature of these pathways underscores the importance of a well-functioning nervous system.
Function and Clinical Relevance
Myotomes, as we’ve explored, represent a specific group of muscles innervated by a single spinal nerve root. Understanding their function is crucial in evaluating neurological health. This section delves into the practical applications of myotome assessment in clinical settings.Myotome assessment provides valuable insights into the integrity of the peripheral nervous system. Clinicians utilize this information to pinpoint potential nerve root impingements, spinal cord lesions, or peripheral neuropathies.
The accuracy of this assessment is pivotal in formulating a diagnosis and developing a targeted treatment plan.
Myotome Function
Myotomes are responsible for specific movements or actions. Each myotome corresponds to a particular set of muscles, and the coordinated activation of these muscles allows for a range of body movements. For example, the C5 myotome controls shoulder abduction, while the L4 myotome facilitates dorsiflexion of the foot. Understanding the specific movements controlled by each myotome helps clinicians assess the extent of potential neurological damage.
Myotome Assessment in Clinical Practice
Clinicians evaluate myotomes through a series of standardized muscle strength tests. These tests involve asking the patient to perform specific movements, and the examiner assesses the strength and range of motion of the corresponding muscles. The examiner grades the strength using a standardized scale, often a 0-5 scale, where 0 indicates no muscle contraction and 5 represents normal strength.
The precise movements and muscle groups tested depend on the suspected area of neurological impairment. Thorough and careful examination is crucial to ensure accurate assessment.
Clinical Uses of Myotome Testing
Myotome testing serves as a vital diagnostic tool in identifying and evaluating neurological conditions. It helps pinpoint the level of spinal cord or nerve root involvement, aiding in differential diagnosis. This testing is particularly useful in cases of suspected nerve root compression, such as from herniated discs, or in conditions like spinal stenosis. Furthermore, myotome assessment can help monitor the progression or response to treatment in various neurological disorders.
A myotome is a group of muscles that are innervated by a single spinal nerve root. Maintaining good kidney health is crucial for overall well-being, and a balanced diet plays a key role. Eating foods rich in antioxidants and low in sodium, such as those highlighted in this resource on foods for kidney health , can contribute significantly to kidney function.
Understanding myotomes is important for diagnosing and treating neuromuscular conditions.
Conditions Where Myotome Assessment is Important
Myotome assessment is critical in several neurological conditions. The information gathered aids in pinpointing the location and extent of the damage to the nervous system. By evaluating muscle strength, clinicians can identify the specific nerve roots or spinal cord segments that are affected. This allows for a more accurate diagnosis and facilitates appropriate treatment.
Examples of Conditions and Expected Myotome Weakness
| Condition | Expected Myotome Weakness | Diagnostic Significance |
|---|---|---|
| Cervical Radiculopathy (C6-C7) | Weakness in elbow flexion and wrist extension | Indicates nerve root compression at the C6-C7 level, potentially from a herniated disc. |
| Lumbar Radiculopathy (L5) | Weakness in foot dorsiflexion and great toe extension | Suggests nerve root compression at the L5 level, possibly due to spinal stenosis or a herniated disc. |
| Spinal Cord Injury (Thoracic Level) | Weakness in shoulder abduction, elbow flexion, and wrist extension. | Indicates a spinal cord lesion, and the level of the lesion can be determined by the specific myotomes affected. |
| Peripheral Neuropathy | Gradual, symmetric weakness in multiple myotomes | Suggests a diffuse or systemic process affecting the peripheral nerves. |
Assessment and Testing
Assessing myotome function is crucial for evaluating neuromuscular health and identifying potential nerve or muscle pathologies. Proper myotome testing involves a systematic approach to evaluate the strength and power of specific muscle groups innervated by particular spinal nerve roots. This allows clinicians to pinpoint the location of potential damage or dysfunction.
Methods for Assessing Myotome Function
Various methods are employed to assess myotome function, each with its strengths and limitations. These methods range from simple manual muscle testing to more sophisticated electromyographic (EMG) studies. Manual muscle testing is a widely used, cost-effective method that relies on the clinician’s observation of the patient’s ability to perform specific movements against resistance. EMG studies provide a more detailed evaluation of muscle electrical activity, allowing for a deeper understanding of muscle function and identifying any neuromuscular disorders.
Steps Involved in a Myotome Examination
A comprehensive myotome examination involves several key steps. First, a thorough patient history and neurological examination are essential to understand the patient’s presenting complaint and potential contributing factors. Second, the examination should focus on identifying the specific muscle groups associated with the relevant myotomes. Third, standardized manual muscle testing procedures should be meticulously followed to ensure accuracy and reliability.
Lastly, interpretation of the findings should be performed with careful consideration of the patient’s overall clinical presentation.
Importance of Proper Technique in Myotome Testing
Proper technique is paramount in myotome testing to ensure accurate and reliable results. Inconsistent or improper techniques can lead to inaccurate assessment and potentially misdiagnosis. Clinicians should adhere to standardized procedures and ensure that the patient is properly positioned and relaxed during the test. Accurate measurement and consistent evaluation criteria are crucial for reliable results. Standardized protocols should be used to maintain consistency and reproducibility.
Step-by-Step Procedure for Testing Specific Myotomes
- Biceps Myotome (C5-C6): Assess the patient’s ability to flex the elbow against resistance. The examiner should position the patient supine or sitting with the elbow flexed at 90 degrees. The examiner applies resistance to the patient’s forearm while the patient attempts to maintain elbow flexion. Note the degree of resistance the patient can overcome. The examiner should observe for any weakness, atrophy, or tremors during the test.
- Triceps Myotome (C6-C7): Assess the patient’s ability to extend the elbow against resistance. The examiner should position the patient supine or sitting with the elbow flexed at 90 degrees. The examiner applies resistance to the patient’s forearm while the patient attempts to extend the elbow. Observe the degree of resistance the patient can overcome. Look for any weakness, atrophy, or tremors during the test.
So, what exactly is a myotome? Basically, it’s a group of muscles that are innervated by a single spinal nerve root. Understanding these muscle groups is crucial for diagnosing nerve damage, and for people exploring natural health options like AHCC supplements, for example, AHCC benefits and safety is an important consideration. Knowing how AHCC might interact with your myotomes is key to potential therapeutic benefits.
Ultimately, a good understanding of myotomes is essential for anyone working with the body’s complex systems.
Note that a weak triceps response can suggest damage to the radial nerve.
- Wrist Extensors (C6-C7): Assess the patient’s ability to extend the wrist against resistance. The patient should be positioned supine or sitting with the forearm supported and the wrist in a neutral position. The examiner applies resistance to the dorsal aspect of the hand as the patient attempts to extend the wrist. Assess the strength and note any weakness. This test evaluates the integrity of the radial nerve.
- Iliopsoas Myotome (L2-L3): Assess hip flexion. The patient should be supine with the knee flexed and the hip at a 90-degree angle. The examiner should apply resistance to the patient’s thigh while they attempt to maintain hip flexion. Record the patient’s ability to maintain the flexion against resistance. Assess for any weakness, atrophy, or other abnormalities.
This is crucial for assessing the integrity of the lumbar plexus and the associated nerves.
Clinical Cases and Examples
Myotome testing plays a crucial role in diagnosing and localizing neurological impairments. By assessing the strength and function of specific muscle groups, clinicians can pinpoint the level of the nervous system affected, whether it’s a peripheral nerve, spinal cord, or brain. Understanding the clinical presentation and interpretation of myotome weakness is vital for developing an accurate diagnosis and appropriate treatment plan.Interpreting myotome testing results requires careful consideration of the patient’s overall neurological presentation.
The presence of other symptoms, such as sensory changes, reflexes, and cognitive impairments, provides valuable context and helps differentiate between various neurological conditions. These combined findings contribute to a comprehensive picture of the patient’s neurological status.
Myotome Weakness in Cervical Radiculopathy
Cervical radiculopathy, often caused by nerve root compression in the neck, frequently leads to specific myotome weakness. The affected myotomes are typically those innervated by the affected nerve roots. For example, C5 and C6 nerve root involvement might result in weakness of the biceps and deltoid muscles, affecting shoulder abduction and flexion.
Myotome Weakness in Spinal Cord Injury
Spinal cord injuries can result in varying degrees of myotome weakness, depending on the level and extent of the damage. A complete spinal cord lesion at the C5 level, for example, would likely produce significant weakness in the muscles innervated by the C5 nerve root and below, leading to weakness in shoulder abduction, elbow flexion, wrist extension, and hand movements.
Myotome Weakness in Peripheral Neuropathy
Peripheral neuropathies encompass a broad range of conditions affecting peripheral nerves. These conditions can lead to varying degrees of myotome weakness depending on the affected nerves. For instance, a diabetic neuropathy can lead to distal muscle weakness affecting the muscles of the feet and legs, impacting ambulation and balance.
Interpreting Myotome Testing Results
Interpreting myotome testing results in conjunction with other neurological findings is crucial for accurate diagnosis. For example, if a patient presents with weakness in the C7 myotome (triceps) but normal reflexes, the cause might be localized to the peripheral nerve rather than the spinal cord. Consideration of the patient’s medical history, symptoms, and other neurological examination findings further enhances diagnostic accuracy.
Case Studies of Myotome Involvement
| Case Scenario | Myotome Affected | Symptoms | Diagnosis |
|---|---|---|---|
| Patient with neck pain, radiating down the arm, and weakness in biceps and wrist extensors. | C5, C6, C7 | Pain, numbness, tingling in the arm and hand, weakness in elbow flexion and wrist extension. | Cervical radiculopathy |
| Patient with a history of a fall, presenting with decreased sensation in the lower extremities and weakness in hip flexion and knee extension. | L2, L3, L4 | Numbness and tingling in the lower extremities, weakness in hip flexion, knee extension, and dorsiflexion. | Spinal cord injury |
| Patient with a history of diabetes, experiencing gradual weakness in the foot and ankle. | L4, L5, S1 | Gradual weakness and numbness in the feet and ankles, difficulty with ambulation. | Diabetic neuropathy |
Variations and Considerations
Myotomes, while providing a valuable framework for assessing neuromuscular function, aren’t a perfect fit for every individual. Variations in their organization and the influence of various factors can significantly affect how a myotome is assessed and interpreted. Understanding these variations and considerations is crucial for accurate diagnoses and effective treatment plans.The consistency in myotome organization, though a useful guide, is not absolute.
Individual variations in muscle fiber type, size, and innervation patterns can affect the specific muscles that make up a myotome. This variability in anatomy necessitates a careful and nuanced approach to myotome assessment, always considering the individual’s unique characteristics.
Variations in Myotome Organization
Individual differences in muscle anatomy and innervation can lead to variations in myotome boundaries. These variations can sometimes result in a muscle being innervated by a nerve root slightly different from the expected pattern. This can cause a myotome to be slightly larger or smaller in some individuals than in others. Factors like genetic predisposition and previous injuries can also play a role in these anatomical variations.
Factors Influencing Myotome Assessment
Several factors can impact the accuracy of myotome testing. Patient cooperation and motivation are critical, as muscle strength is affected by psychological factors like fear and anxiety. Pain, fatigue, and other medical conditions can also influence the ability to perform muscle tests, potentially leading to inaccurate or misleading results. Furthermore, the examiner’s skill and experience in performing the tests directly impacts the reliability of the assessment.
Careful consideration of these influencing factors is paramount to obtaining meaningful and reliable results.
Limitations of Myotome Testing
Myotome testing, despite its usefulness, has limitations. It provides a general indication of nerve root function but doesn’t offer a precise measurement of the extent of the nerve damage. The test’s resolution is limited, and subtle deficits may be missed. Additionally, myotome testing relies on the patient’s ability to cooperate, which can be affected by factors like pain or cognitive impairment.
It’s important to recognize that myotome testing is a component of a broader neurological assessment, not a stand-alone diagnostic tool.
Considerations for Assessing Myotomes in Different Age Groups
Age significantly impacts muscle strength and the ability to perform motor tasks. Children and older adults may have different baseline strength levels, requiring adjusted assessment methods and interpretations. The developmental stages of children, for example, need to be taken into account. In children, the myotome assessment might focus on milestones and developmental norms, rather than precise strength measurements.
Table: Age Group Considerations for Myotome Assessment
| Age Group | Potential Variations | Assessment Considerations |
|---|---|---|
| Infants (0-1 year) | Immature neuromuscular system, limited voluntary movement | Focus on developmental milestones, use of reflexes, parental input |
| Children (2-12 years) | Varying developmental stages, rapid growth spurts | Use age-appropriate tasks, consider developmental norms, assess cooperation |
| Adults (18-65 years) | Stable muscle mass, generally consistent motor abilities | Standard myotome testing methods are generally applicable |
| Older Adults (65+) | Decreased muscle mass, decreased strength, potential comorbidities | Adjust testing to accommodate limitations, assess for confounding factors, use caution |
Imaging and Techniques
Visualizing myotomes, the groups of muscles innervated by a single spinal nerve root, presents unique challenges. While direct visualization of muscle function isn’t possible with standard imaging, these techniques can provide valuable information about the structures involved, aiding in the diagnosis and understanding of neuromuscular conditions. Understanding the limitations of these techniques is equally crucial for accurate interpretation.Imaging modalities offer insights into the anatomy of myotomes, but don’t directly measure their functional capacity.
This is critical to remember when interpreting results, as imaging findings must be correlated with other assessments like electromyography (EMG) and nerve conduction studies (NCS) to gain a comprehensive picture. Indirect assessments of myotome involvement are possible through visualization of neural pathways and structures related to muscle function.
MRI and CT Imaging
Magnetic resonance imaging (MRI) and computed tomography (CT) scans are valuable tools for visualizing the anatomy of the spine, spinal cord, and surrounding tissues. These techniques can depict the spinal nerves, which are crucial for understanding myotome function. MRI excels at providing detailed soft tissue images, highlighting potential spinal cord compression or nerve root impingement, which can affect the associated myotomes.
CT, on the other hand, provides excellent bone detail, aiding in identifying bony structures that might contribute to nerve root compression.
Limitations of Imaging Techniques
Imaging techniques primarily visualize thestructures* involved in myotome function, not the function itself. For example, an MRI might reveal a herniated disc compressing a nerve root, but it doesn’t directly demonstrate the resultant weakness in the muscles of the corresponding myotome. Other factors, like the severity of the compression or the individual’s response to the condition, can also affect the myotome’s function and are not directly measurable by these techniques.
Visualizing Neural Pathways
Visualization of neural pathways involves advanced techniques. Advanced MRI techniques, such as diffusion tensor imaging (DTI), can map the pathways of nerve fibers, providing insights into the integrity of neural connections. This is crucial in cases of suspected nerve damage or disease, aiding in identifying the affected myotomes.
Electrodiagnostic Studies (EMG and NCS)
Electromyography (EMG) and nerve conduction studies (NCS) are essential for evaluating the electrical activity of muscles and nerves. EMG measures the electrical activity of muscle fibers, while NCS assesses the speed and amplitude of nerve impulses. These studies can directly assess the functional integrity of the myotomes, detecting issues like denervation (loss of nerve supply) or axonal damage.
For instance, if a specific myotome shows reduced or absent electrical activity, it suggests a potential problem with the nerve root or the muscles it supplies.
Comparison of Imaging Modalities
| Imaging Modality | Strengths | Limitations | Application in Myotome Assessment |
|---|---|---|---|
| MRI | Excellent soft tissue detail, visualization of spinal cord and nerve roots | Limited visualization of bone structures, can be expensive | Identifying spinal cord compression, nerve root impingement |
| CT | Excellent bone detail, rapid acquisition | Limited soft tissue contrast, higher radiation exposure | Identifying bony structures contributing to nerve root compression |
| DTI | Visualization of neural pathways | Requires specialized software and interpretation, more expensive than standard MRI | Assessing nerve fiber integrity, identifying areas of potential damage |
| EMG/NCS | Direct assessment of muscle and nerve function | Invasive procedure, requires specialized expertise for interpretation | Evaluating the functional integrity of the myotomes, detecting denervation or axonal damage |
Ending Remarks
In conclusion, understanding myotomes provides a critical lens through which we can appreciate the intricate relationship between the nervous system and our muscles. From a clinical standpoint, myotome assessment is invaluable for pinpointing the source of neurological issues. This guide has explored the key aspects of myotomes, offering a clear understanding of their definition, anatomy, function, and clinical applications.
We’ve seen how these muscle groups, coordinated by specific nerve roots, are crucial for our everyday movements and how their assessment is a valuable tool in diagnosing various conditions. Myotomes are more than just anatomical structures; they’re essential for our health and well-being.