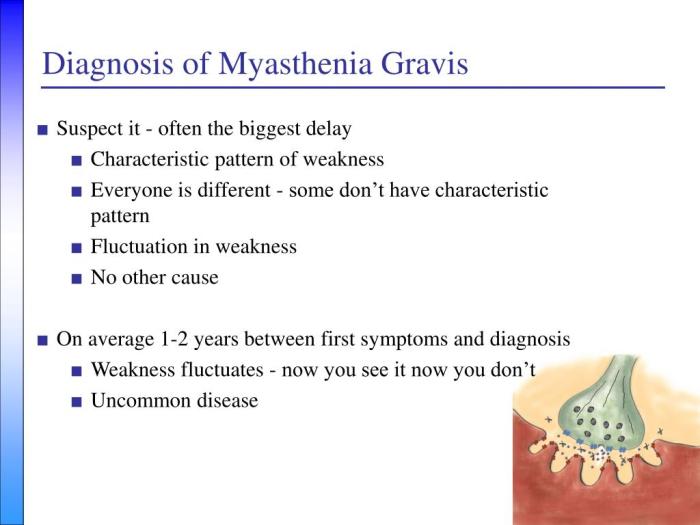
How myasthenia gravis is diagnosed is a crucial process, often involving a multifaceted approach. This journey begins with recognizing the subtle and sometimes overlooked initial symptoms, progressing through neurological examinations, and culminating in a series of diagnostic tests. Understanding the various methods used in the diagnostic process can help patients and their families navigate this complex health challenge with greater awareness and confidence.
This comprehensive guide explores the different steps involved in diagnosing myasthenia gravis, from initial symptom assessment to advanced laboratory tests and imaging techniques. We’ll delve into the nuances of muscle weakness, neurological evaluations, and the crucial role of diagnostic tests such as the Edrophonium test and repetitive nerve stimulation. A detailed understanding of these processes can help those affected better navigate the diagnostic pathway.
Initial Symptoms and Presenting Complaints

Myasthenia gravis (MG) is a chronic autoimmune neuromuscular disease characterized by fluctuating muscle weakness. Understanding the initial symptoms and presenting complaints is crucial for early diagnosis and effective management. Recognizing the diverse ways MG manifests is essential to avoid delayed diagnosis, which can lead to a poorer prognosis. The symptoms vary widely, depending on the specific muscles affected.
Common Initial Symptoms
Initial symptoms of myasthenia gravis often begin subtly, with gradual worsening of muscle weakness over time. The hallmark feature is fluctuating muscle weakness, meaning the strength of the affected muscles can change throughout the day, and sometimes even within hours. This fluctuation can make it challenging for patients to accurately describe their symptoms. Common initial complaints often involve muscles used for repetitive or sustained activity.
Presenting Complaints by Muscle Group
The presenting complaints in myasthenia gravis can vary greatly depending on the muscle groups affected. Patients might experience difficulty with various tasks due to the varying weakness.
- Ocular Symptoms: Double vision (diplopia) is a frequent and often the first symptom. It typically affects one or both eyes, often worse at the end of the day or after prolonged use. Ptosis (drooping eyelids) is another common ocular symptom, often occurring in conjunction with diplopia.
- Facial Symptoms: Difficulty smiling, chewing, or making facial expressions is common. Weakness of facial muscles can lead to a characteristic “mask-like” appearance. Difficulty with swallowing (dysphagia) can also present as an early symptom.
- Bulbar Symptoms: Difficulty speaking, swallowing, or chewing (bulbar weakness) can indicate involvement of the cranial nerves controlling these functions. These symptoms often manifest as slurred speech, difficulty with mastication, and progressive dysphagia.
- Limb Symptoms: Weakness in the arms and legs, often affecting both sides equally, can occur. This weakness can present as difficulty with tasks like lifting objects, climbing stairs, or walking.
Typical Onset and Progression of Different MG Subtypes
The onset and progression of myasthenia gravis can vary significantly, even within the same patient. This variability necessitates a comprehensive understanding of the disease.
| Subtype | Typical Onset | Progression | Notes |
|---|---|---|---|
| Ocular MG | Often insidious, starting with ptosis or diplopia | Slowly progressive, may not affect other muscle groups | Frequently the first subtype to appear |
| Generalized MG | Can start in any muscle group | Rapid progression affecting multiple muscle groups | Symptoms often more severe and widespread |
| Bulbar MG | Often starts with dysphagia, dysarthria, or both | Can lead to significant swallowing and speaking difficulties | May progress to respiratory compromise |
Triggers and Exacerbating Factors
Several factors can exacerbate symptoms of myasthenia gravis. These factors are important to consider when assessing a patient’s condition.
- Fatigue: Physical or mental exertion can significantly worsen muscle weakness. This is often a major factor for patients, leading to reduced functional capacity.
- Stress: Emotional stress and anxiety can trigger or worsen symptoms. This can be an important consideration for managing symptoms.
- Infection: Infections, especially viral infections, can temporarily worsen the symptoms of myasthenia gravis.
- Certain Medications: Some medications, including antibiotics, can temporarily exacerbate symptoms.
Indicators of Myasthenia Gravis in General Weakness
General weakness can be a symptom of many conditions, but several indicators can suggest myasthenia gravis.
- Fluctuating Weakness: Weakness that comes and goes, improving with rest and worsening with activity, is a strong indicator. This is a key differentiating feature from other causes of weakness.
- Presence of Ocular Symptoms: The presence of ptosis or diplopia, even in the absence of other symptoms, should raise suspicion for myasthenia gravis.
- Family History: A family history of autoimmune disorders may increase the likelihood of myasthenia gravis.
- Exacerbation with Repetitive Activity: If the weakness worsens with repeated muscle use, it might suggest a neuromuscular junction problem like myasthenia gravis.
Neurological Examination Procedures
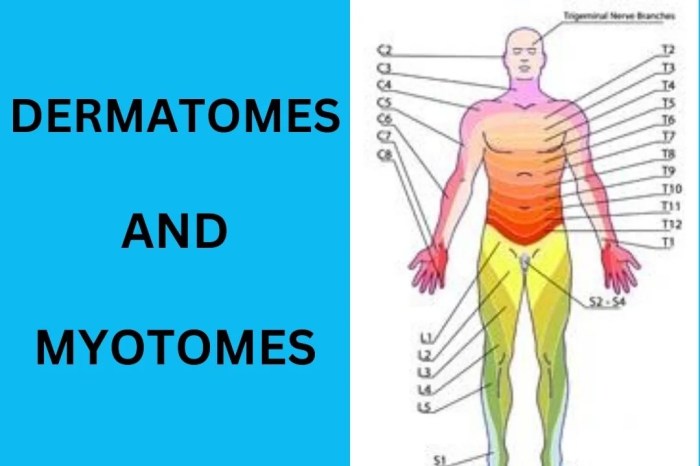
Unraveling the complexities of Myasthenia Gravis often hinges on meticulous neurological examinations. These procedures provide crucial insights into the patient’s muscle strength, function, and the specific involvement of the neuromuscular junction. By identifying characteristic patterns of weakness and evaluating cranial nerve function, clinicians can narrow down the diagnosis and tailor treatment strategies.
Muscle Strength and Function Assessment
Neurological examinations for myasthenia gravis (MG) focus on assessing muscle strength and fatiguability. Clinicians utilize various techniques to evaluate the extent and pattern of weakness. These techniques are designed to identify the characteristic fatigability patterns, a key diagnostic feature of MG. Precise documentation of these findings is vital for monitoring disease progression and treatment efficacy.
Neuromuscular Junction Evaluation
Specific tests are employed to evaluate the neuromuscular junction (NMJ), the site where nerves communicate with muscles. These tests aim to assess the efficiency of nerve impulse transmission. The rationale behind each procedure is to pinpoint any disruptions in the NMJ, which may be indicative of MG.
Key Neurological Findings in Myasthenia Gravis
| Neurological Finding | Description | Clinical Significance | Example |
|---|---|---|---|
| Muscle Weakness | Varying degrees of muscle weakness, particularly in muscles controlling eye movements, facial expression, swallowing, and limb movements. Weakness often worsens with repetitive use or prolonged activity. | A hallmark symptom of MG, indicating impaired neuromuscular transmission. | Difficulty raising eyelids, drooping eyelids (ptosis), double vision (diplopia), facial weakness, difficulty chewing, or swallowing. |
| Cranial Nerve Dysfunction | Impairment in cranial nerves, most commonly affecting those controlling eye movement (III, IV, VI), facial expression (VII), and swallowing (IX, X). | Suggests the presence of neuromuscular dysfunction affecting specific nerve pathways. | Ocular palsies, dysarthria, dysphagia, and facial weakness. |
| Fatiguability | Progressive weakening of muscles with sustained or repetitive use. | A crucial diagnostic sign in MG, reflecting the impaired ability of the NMJ to maintain the necessary neurotransmitter release. | Weakness worsens after sustained activity or repetition, like sustained eye movements. |
| Response to Ice Packs | Temporary improvement in muscle strength after applying ice packs to affected muscles. | Can indicate the presence of a myasthenic crisis. | Temporary improvement in eye movement after ice application. |
Detecting Characteristic Patterns of Muscle Weakness
Identifying the characteristic patterns of muscle weakness in MG involves careful observation and testing. Clinicians evaluate the extent and location of weakness, noting whether it affects specific muscle groups or cranial nerves. They observe how weakness changes with rest and activity, specifically if the weakness increases with repeated use or activity. Furthermore, the presence of fatiguability during specific tasks like sustained eye movements is crucial for diagnosis.
Importance of Cranial Nerve Function Evaluation
Evaluating cranial nerve function is essential in a patient suspected of having myasthenia gravis. Cranial nerves innervate vital muscles involved in vision, facial expression, chewing, swallowing, and speech. Any impairment in these functions can significantly impact a patient’s quality of life. The presence of specific cranial nerve palsies, particularly those affecting ocular muscles, strongly suggests the possibility of MG.
Thorough testing and documentation of cranial nerve function provide vital clues for diagnosis and management.
Diagnostic Tests
Navigating the diagnostic journey for Myasthenia Gravis (MG) often involves a combination of clinical assessments and specific tests. A thorough understanding of these tests is crucial for accurate diagnosis and effective management of the condition. The goal is to pinpoint the underlying neuromuscular dysfunction that characterizes MG, enabling the right treatment plan to be implemented.
Diagnosing myasthenia gravis often involves a combination of physical exams, neurological assessments, and blood tests. Doctors look for specific symptoms, like muscle weakness that worships throughout the day, and often, try to rule out other conditions. Switching to healthier alternatives to full-fat dairy products, like healthy alternatives to full fat dairy products , can be a beneficial part of a comprehensive treatment plan, though it’s crucial to remember that this is a complex disease and dietary changes alone won’t diagnose or cure it.
Ultimately, a team of specialists and thorough testing are key to accurate diagnosis.
Edrophonium (Tensilon) Test, How myasthenia gravis is diagnosed
This test is a crucial diagnostic tool in evaluating suspected myasthenia gravis. It involves administering edrophonium, a cholinesterase inhibitor, intravenously. The rationale behind this test is that cholinesterase inhibitors increase the amount of acetylcholine available at the neuromuscular junction. This, in turn, can temporarily improve muscle strength in individuals with MG.
The mechanism of action is straightforward: edrophonium inhibits acetylcholinesterase, the enzyme that breaks down acetylcholine. This leads to an increased concentration of acetylcholine in the synaptic cleft, stimulating muscle contraction more effectively.
During the test, muscle strength is meticulously observed before and after the injection. A positive response, characterized by a marked improvement in muscle strength within minutes of the injection, strongly suggests MG. Conversely, a lack of improvement or a minimal response typically indicates that MG is not the primary cause of the symptoms. Important considerations include potential side effects such as bradycardia, nausea, or muscle fasciculations.
The test should only be performed under strict medical supervision.
Diagnosing myasthenia gravis often involves a combination of physical exams, neurological tests, and sometimes even blood tests. It’s a complex process, much like figuring out how to manage a stuffy nose at night, which can often be a real struggle. Fortunately, there are some simple strategies to try, like using a saline nasal spray, which can help clear up congestion and make breathing easier.
This process of elimination and targeted approaches, similar to figuring out the right combination of strategies for a stuffy nose, is important in diagnosing myasthenia gravis accurately. Ultimately, a doctor will need to consider various factors to make a precise diagnosis. how to reduce a stuffy nose at night can help find relief.
Repetitive Nerve Stimulation (RNS) Testing
RNS testing assesses the neuromuscular junction’s response to repeated nerve stimulation. The rationale is that in MG, repeated nerve stimulation leads to a quicker decline in muscle strength compared to healthy individuals. This decline is a reflection of the fatigued neuromuscular junction’s reduced ability to produce acetylcholine effectively.
The procedure involves electrically stimulating a nerve repeatedly, measuring the strength of the resulting muscle contractions. The test identifies the pattern of muscle weakness as a result of repeated stimulation. A progressive decrease in the amplitude of muscle action potentials is a significant finding suggestive of MG.
Electromyography (EMG)
EMG is a diagnostic procedure that evaluates the electrical activity of muscles. It plays a crucial role in assessing neuromuscular transmission, the process by which nerve impulses trigger muscle contractions. The rationale for using EMG is that it can reveal subtle abnormalities in the electrical signals produced by muscles and nerves, helping to distinguish between different neuromuscular disorders.
Diagnosing myasthenia gravis often involves a combination of physical exams, neurological tests, and sometimes even blood tests. It’s a tricky diagnosis, and sometimes, symptoms can overlap with other conditions like, for example, what is tmj disorder , making accurate identification crucial. Ultimately, a thorough evaluation by a neurologist is key to pinpointing the cause and receiving the right treatment for myasthenia gravis.
During EMG, electrodes are inserted into specific muscles to record their electrical activity. Normal muscle activity is characterized by specific patterns of electrical signals. EMG can reveal characteristic abnormalities in MG, such as reduced amplitude of muscle action potentials and prolonged relaxation times. It’s important to note that EMG findings alone are not always definitive for MG and may require correlation with other clinical and test results.
Comparison of Diagnostic Tests
| Test | Strengths | Limitations | Typical Findings in MG |
|---|---|---|---|
| Edrophonium (Tensilon) Test | Quick, relatively simple, and can provide immediate diagnostic clues. | Can cause adverse reactions, may not be conclusive in all cases, and is not suitable for everyone. | Marked improvement in muscle strength after edrophonium administration. |
| Repetitive Nerve Stimulation (RNS) | Objective measure of neuromuscular junction fatigue, highly sensitive to early signs of MG. | Requires specialized equipment and interpretation by trained personnel. | Progressive decrease in muscle action potential amplitude with repeated stimulation. |
| Electromyography (EMG) | Provides detailed information about muscle and nerve function, helpful in ruling out other conditions. | Can be invasive, requires specialized interpretation, and may not always directly pinpoint MG. | Reduced amplitude of muscle action potentials and prolonged relaxation times. |
Laboratory Tests: How Myasthenia Gravis Is Diagnosed
Beyond the crucial neurological examination, laboratory tests play a vital role in confirming and characterizing myasthenia gravis (MG). These tests help identify specific immune system responses and rule out other conditions with similar symptoms. They provide critical supporting evidence to aid in the diagnosis and management of MG.Laboratory tests are invaluable tools in the diagnostic process for myasthenia gravis, supplementing clinical findings and neurological examination results.
These tests help differentiate MG from other neuromuscular disorders and provide insights into the underlying immune mechanisms.
Serum Acetylcholine Receptor (AChR) Antibody Testing
A crucial laboratory test in MG diagnosis is the serum AChR antibody test. AChR antibodies are autoantibodies that target the acetylcholine receptors (AChRs) at the neuromuscular junction. The presence of these antibodies strongly suggests MG.The procedure involves drawing a blood sample and analyzing it for the presence and level of AChR antibodies. Various methods exist for detecting these antibodies, including enzyme-linked immunosorbent assays (ELISAs).
The interpretation of the results is critical. A positive result, indicating the presence of AChR antibodies, significantly strengthens the suspicion of MG, especially when coupled with clinical symptoms and a neurological examination. The level of antibodies can also provide information about the severity of the disease.
Muscle-Specific Kinase (MuSK) Antibody Testing
MuSK antibodies are another type of autoantibody implicated in MG. These antibodies target the muscle-specific kinase (MuSK) protein, also crucial at the neuromuscular junction. MuSK antibodies are present in a subset of MG patients, often those who do not have detectable AChR antibodies. This finding highlights the complexity of MG and the diverse mechanisms driving the disease.The procedure for MuSK antibody testing is similar to AChR antibody testing, involving blood draws and specialized laboratory analysis.
Interpretation of MuSK antibody test results is essential. A positive result, indicating the presence of MuSK antibodies, suggests a form of MG, particularly when clinical symptoms and neurological examination support the diagnosis.
Other Relevant Laboratory Tests
Thyroid function tests are routinely included in the laboratory workup for MG, even though they are not directly related to the disease. This is because thyroid disorders can sometimes mimic MG symptoms. Other laboratory tests, such as complete blood counts (CBCs), electrolytes, and creatine kinase (CK) levels, might be ordered to rule out other conditions or assess overall health.
These tests are vital for a comprehensive evaluation.
Summary of Laboratory Test Results in Myasthenia Gravis
| Test | Typical Finding in MG | Deviation from Normal | Clinical Significance |
|---|---|---|---|
| Serum AChR Antibodies | Positive | Elevated levels | Strong indication of MG; level may correlate with disease severity |
| Serum MuSK Antibodies | Positive (in some cases) | Elevated levels | Suggests a subtype of MG; often seen in patients negative for AChR antibodies |
| Thyroid Function Tests | Normal | Abnormal thyroid hormone levels (hypothyroidism or hyperthyroidism) | May mimic MG symptoms; necessitates further investigation |
| Complete Blood Count (CBC) | Normal | Anemia, lymphopenia, or other abnormalities | Could suggest other conditions or complications |
| Electrolytes | Normal | Imbalances | May indicate underlying issues or complications |
| Creatine Kinase (CK) | Normal | Elevated levels | Suggests muscle damage; may indicate a complication or other underlying conditions |
Imaging Techniques
Imaging techniques play a limited role in the diagnosis of myasthenia gravis (MG). While they can be helpful in excluding other conditions with similar symptoms, they don’t typically provide definitive evidence of MG. Their utility is most often in ruling out structural abnormalities in the neuromuscular junction or other neurological conditions that might mimic MG.Imaging studies are typically not the first-line diagnostic tools for MG.
A comprehensive neurological examination, along with a detailed medical history and laboratory tests, are usually more critical in reaching a diagnosis. Imaging is often employed only when other tests are inconclusive or when there’s a strong suspicion of an underlying structural problem that might be contributing to the symptoms.
Role of Imaging in MG Diagnosis
Imaging plays a supportive role in the diagnostic process. It can help rule out alternative diagnoses or reveal structural abnormalities that might be affecting neuromuscular transmission, potentially mimicking the symptoms of MG. However, imaging alone is insufficient to establish a definitive diagnosis of MG.
Specific Imaging Modalities
Several imaging techniques may be employed in the evaluation of patients suspected of having MG. The choice depends on the specific clinical questions and the suspected location of any potential abnormality.
Neuroimaging
Neuroimaging techniques, including magnetic resonance imaging (MRI) and computed tomography (CT), are commonly used to evaluate the brain, spinal cord, and other neural structures. These studies can reveal the presence of masses, lesions, or other abnormalities that might be affecting the nervous system. While these techniques are valuable for ruling out other neurological conditions, they rarely show specific findings directly related to MG.
Muscle Imaging
Muscle imaging, using techniques like magnetic resonance imaging (MRI), can be utilized in certain situations. This is typically done when there’s a strong suspicion of muscle involvement that isn’t easily explained by other tests. Muscle MRI can potentially show evidence of muscle atrophy or other structural changes. However, these findings are often not pathognomonic for MG.
Table of Imaging Modalities in MG
| Imaging Modality | Usefulness in Identifying Associated Abnormalities | Relevant Image Findings (Possible but not Specific) | Limitations |
|---|---|---|---|
| MRI of Brain and Spinal Cord | Useful for ruling out other neurological conditions (e.g., tumors, multiple sclerosis). | May show lesions or masses in the brain or spinal cord. | Does not directly visualize neuromuscular junction. |
| MRI of Muscles | May reveal muscle atrophy or structural changes in cases of suspected myopathic involvement. | Potential for showing atrophy or inflammation of specific muscle groups. | Less sensitive for detecting the subtle neuromuscular changes of MG. |
| CT Scan | Less frequently used than MRI for evaluating the nervous system. May be helpful for detecting certain types of masses or bony abnormalities. | May show bony abnormalities or lesions. | Lower resolution compared to MRI for soft tissue structures. |
Differential Diagnosis
Myasthenia gravis (MG) can sometimes masquerade as other neurological disorders, making accurate diagnosis crucial. A thorough differential diagnosis is essential to distinguish MG from conditions with overlapping symptoms, ensuring the correct treatment plan is implemented. This process involves ruling out various possibilities that might cause similar symptoms, such as muscle weakness or fatigue. Failure to identify and exclude these conditions can lead to inappropriate therapies and potentially delay the appropriate treatment for MG.Careful consideration of the patient’s medical history, physical examination findings, and results from various diagnostic tests are vital to differentiate MG from other neuromuscular conditions.
Precise identification of the underlying cause of the symptoms is essential for appropriate management and to avoid potential misdiagnosis.
Conditions Mimicking Myasthenia Gravis
Many neurological and other medical conditions can present with symptoms similar to those of myasthenia gravis, including muscle weakness and fatigue. A comprehensive differential diagnosis considers these possibilities to ensure an accurate assessment of the patient’s condition.
- Other Neuromuscular Disorders: Conditions such as Lambert-Eaton myasthenic syndrome (LEMS), botulism, and other neuromuscular junction disorders share overlapping symptoms with MG. The distinct characteristics of each condition, such as the presence or absence of specific antibodies or responses to different medications, are crucial for differentiation. For instance, LEMS often presents with muscle weakness that improves with repeated use, while MG typically worsens with repeated use.
- Autoimmune Diseases: Systemic lupus erythematosus (SLE), rheumatoid arthritis, and other autoimmune disorders can sometimes cause muscle weakness as a secondary effect. The presence of characteristic symptoms and associated laboratory findings helps in distinguishing these conditions from MG.
- Infectious Diseases: Infections like Lyme disease, poliomyelitis, and others can manifest with muscle weakness. Careful evaluation of the patient’s medical history and laboratory tests, such as serological testing, aid in distinguishing these conditions from MG.
- Neurodegenerative Diseases: Amyotrophic lateral sclerosis (ALS) and other neurodegenerative diseases can cause progressive muscle weakness. The progressive nature and specific neurological findings associated with these diseases help differentiate them from the fluctuating weakness often seen in MG.
- Endocrine Disorders: Hypothyroidism, hyperthyroidism, and other endocrine disorders can cause muscle weakness. Appropriate laboratory tests for thyroid function and other relevant endocrine parameters can aid in distinguishing these conditions.
- Medication Side Effects: Certain medications can cause muscle weakness as a side effect. Carefully reviewing the patient’s medication list and considering the timing of symptom onset in relation to medication use is essential.
- Structural Neuromuscular Diseases: Conditions like muscular dystrophy, myopathies, and peripheral neuropathies can mimic MG. Detailed neurological examination and specific muscle biopsy results help differentiate these from MG.
Distinguishing Features
Accurate diagnosis relies on a thorough understanding of the key differentiating characteristics between MG and other neuromuscular conditions. Precise identification of the distinctive features of each condition helps clinicians arrive at the correct diagnosis.
| Characteristic | Myasthenia Gravis | Lambert-Eaton Myasthenic Syndrome (LEMS) | Amyotrophic Lateral Sclerosis (ALS) |
|---|---|---|---|
| Muscle Weakness | Fluctuating weakness, typically worse with repeated use; improved with rest. Often affecting ocular, bulbar, and limb muscles. | Weakness improves with repeated use; characteristically affects proximal muscles first. | Progressive, symmetrical muscle weakness affecting both upper and lower extremities. |
| Response to Edrophonium (Tensilon) Test | Improved muscle strength following edrophonium administration. | Muscle strength worsens following edrophonium administration. | No significant change in muscle strength with edrophonium. |
| EMG Findings | May show decremental response to repetitive nerve stimulation. | May show incremental response to repetitive nerve stimulation. | May show denervation and fibrillation potentials. |
| Autoantibodies | Presence of acetylcholine receptor antibodies (AChR-Abs) or muscle-specific kinase antibodies (MuSK-Abs). | Presence of presynaptic calcium channel antibodies. | Absence of specific autoantibodies. |
Closing Summary
In conclusion, diagnosing myasthenia gravis requires a careful evaluation of symptoms, neurological findings, and a battery of diagnostic tests. This multifaceted approach ensures a more accurate and timely diagnosis, paving the way for appropriate treatment and management strategies. The key is early detection and intervention, allowing individuals to live more fulfilling lives despite the challenges presented by this condition.