Magnesium for muscle pain is a crucial topic for understanding the role of this vital mineral in maintaining healthy muscles. Magnesium plays a significant part in muscle function, and deficiencies can lead to a range of issues, including persistent muscle aches and discomfort. This article explores the intricate connection between magnesium and muscle pain, examining various aspects, from the role of magnesium in different muscle types to the potential benefits of supplementation, and beyond.
We’ll delve into the potential mechanisms behind magnesium’s impact on muscle pain, comparing and contrasting it with other potential causes. The article will also explore the importance of dietary sources of magnesium, alongside various forms of supplements and their pros and cons. Finally, we’ll touch upon diagnosis, treatment strategies, and important considerations regarding interactions with other medications or supplements.
Introduction to Magnesium and Muscle Pain
Magnesium plays a crucial role in numerous bodily functions, and muscle health is no exception. It’s essential for muscle contraction, relaxation, and nerve function. Without adequate magnesium levels, the delicate balance within these processes can be disrupted, potentially leading to muscle pain and other symptoms. This article delves into the connection between magnesium and muscle pain, exploring the mechanisms behind the link and the common symptoms associated with magnesium deficiency.Magnesium is a vital mineral that acts as a cofactor for over 300 enzymatic reactions in the body.
This includes reactions directly related to muscle function, such as those involved in nerve impulse transmission and the release of calcium, which is essential for muscle contraction. Imbalances in these processes, often stemming from insufficient magnesium intake, can lead to a cascade of effects, including muscle pain.
Magnesium’s Role in Muscle Function
Magnesium is fundamental to the proper functioning of all muscle types. It is involved in the crucial steps of muscle contraction and relaxation. It aids in the regulation of calcium release, ensuring smooth and coordinated muscle activity. Without sufficient magnesium, the delicate balance of calcium regulation can be compromised, leading to potential muscle spasms or cramps.
Potential Mechanisms of Magnesium Deficiency-Related Muscle Pain
Magnesium deficiency can disrupt the intricate interplay of ions within muscle cells. This disruption affects the release and reuptake of calcium, leading to sustained muscle contractions and the sensation of pain. The imbalance can also impact nerve signal transmission, which plays a critical role in muscle function.
Common Symptoms of Magnesium Deficiency, Including Muscle Pain
Magnesium deficiency can manifest in a variety of ways, and muscle pain is often one of the presenting symptoms. Other common symptoms include fatigue, weakness, nausea, headaches, and irregular heartbeat. It’s important to remember that these symptoms can be caused by other conditions as well, so it’s crucial to consult with a healthcare professional for accurate diagnosis. Early diagnosis and intervention are key to managing the condition effectively.
- Muscle Pain: A common symptom of magnesium deficiency, characterized by cramping, spasms, or soreness in various muscle groups. This pain can range from mild discomfort to severe debilitating pain.
- Fatigue: A persistent feeling of tiredness and lack of energy. This can be a significant symptom of magnesium deficiency, often affecting daily activities and overall well-being.
- Weakness: Reduced strength and power in muscles, making everyday tasks more challenging.
- Nausea: A feeling of discomfort in the stomach, often accompanied by an urge to vomit.
- Headaches: Pain in the head, often described as throbbing or pulsing.
- Irregular Heartbeat: An abnormal heart rhythm, which can range from mild palpitations to more serious cardiac issues. This is a serious symptom and requires immediate medical attention.
Comparison of Magnesium’s Role in Different Muscle Types
| Muscle Type | Magnesium’s Role | Specific Function |
|---|---|---|
| Skeletal Muscle | Crucial for muscle contraction and relaxation, calcium regulation. | Essential for voluntary movements, maintaining posture, and generating force. |
| Smooth Muscle | Regulates calcium influx and efflux, influencing contraction and relaxation. | Essential for involuntary movements, such as digestion, blood flow, and organ function. |
| Cardiac Muscle | Critical for maintaining the heart’s rhythmic contractions. | Essential for pumping blood throughout the body. |
Magnesium is vital for the proper functioning of all muscle types, playing a crucial role in regulating calcium and ensuring smooth muscle contractions and relaxations.
Magnesium is often a helpful supplement for muscle pain, but sometimes underlying issues can be more complex. For example, if you’re experiencing severe chest pain, it’s crucial to consider potential heart problems, such as needing a double bypass heart surgery. what is a double bypass heart surgery can be a life-saving procedure, but even then, magnesium can still play a role in muscle recovery and overall well-being after the surgery.
In any case, always consult your doctor before taking any new supplements.
Magnesium Supplements and Muscle Pain Relief
Magnesium is a crucial mineral for various bodily functions, including muscle contraction and relaxation. A deficiency in magnesium can contribute to muscle cramps, spasms, and persistent pain. Supplementation with magnesium can potentially alleviate these symptoms by replenishing depleted levels and supporting optimal muscle function.Magnesium supplements come in various forms, each with potential advantages and disadvantages regarding absorption and effectiveness.
Understanding the different types and their respective characteristics can help individuals choose the most suitable option for their needs. Proper dosage is equally important to maximize benefits and minimize potential side effects.
Magnesium Supplement Forms
Different forms of magnesium supplements vary in their absorption rates and potential side effects. Understanding these differences is crucial for selecting the most appropriate form. Common forms include magnesium oxide, magnesium citrate, magnesium glycinate, magnesium malate, and magnesium sulfate.
Recommended Magnesium Dosages
Determining the appropriate dosage of magnesium supplements depends on individual needs and the severity of muscle pain. Generally, a daily intake of 300-400 mg is often recommended as a starting point. However, individual needs can vary. Consulting a healthcare professional is essential to determine the optimal dosage tailored to specific circumstances and medical conditions.
Magnesium is often a helpful remedy for muscle aches and pains. While exploring different options, it’s important to consider other potential underlying causes. For instance, if you’re experiencing irregular heartbeats, medications for atrial fibrillation, like those discussed in detail here medications for atrial fibrillation , might be necessary. Ultimately, magnesium supplementation can be a beneficial approach to muscle pain relief, especially when combined with a healthy lifestyle.
Magnesium Supplement Types: Pros and Cons
| Supplement Type | Pros | Cons |
|---|---|---|
| Magnesium Oxide | Generally inexpensive. | Low absorption rate. Potential for digestive upset (constipation) in higher doses. |
| Magnesium Citrate | High absorption rate. Generally well-tolerated. | May cause diarrhea in some individuals. |
| Magnesium Glycinate | Excellent absorption rate. Often well-tolerated, less likely to cause digestive issues compared to other forms. | Can be more expensive than other forms. |
| Magnesium Malate | High absorption rate. Potentially beneficial for athletes due to its role in energy production. | Generally well-tolerated, but some individuals may experience mild digestive issues. |
| Magnesium Sulfate (Epsom Salts) | Often used for baths or topical applications. | Lower absorption rate when taken orally. |
Potential Side Effects of Magnesium Supplementation
Magnesium supplementation, while generally safe, can cause some side effects in certain individuals. These side effects are often dose-dependent and can include diarrhea, nausea, abdominal cramps, and a feeling of bloating. It’s crucial to start with a low dose and gradually increase it as tolerated. If severe side effects occur, discontinue use and consult a healthcare professional immediately.
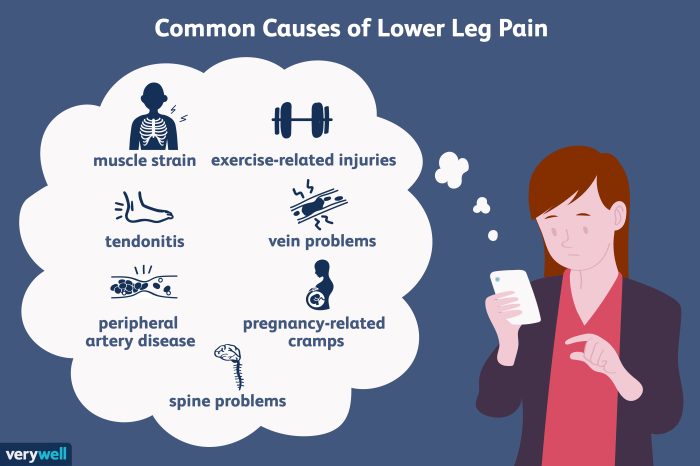
Other Factors Contributing to Muscle Pain
Muscle pain, a common ailment, can stem from a multitude of sources beyond magnesium deficiency. Understanding these contributing factors is crucial for effective management. Often, muscle pain arises from a complex interplay of various elements, highlighting the importance of a holistic approach to diagnosis and treatment. This includes considering potential inflammation, injuries, and other nutritional deficiencies.Identifying the root cause is essential for tailored interventions.
A thorough assessment by a healthcare professional, considering the patient’s complete medical history, lifestyle, and dietary habits, is critical for effective management. The interaction between different factors can significantly impact the severity and persistence of muscle pain.
Inflammation as a Contributing Factor
Inflammation, a natural response to injury or infection, can lead to muscle pain and tenderness. This inflammatory response involves the body’s immune system mobilizing to repair damaged tissues. In cases of chronic inflammation, the inflammatory process can become prolonged, contributing to persistent muscle pain. Examples include conditions like rheumatoid arthritis, fibromyalgia, and certain infections. These conditions can overlap with magnesium deficiency, exacerbating muscle pain symptoms.
Injuries and Muscle Strains
Muscle strains and tears, resulting from overuse, sudden impact, or improper form during exercise, frequently cause localized muscle pain. The severity of the pain varies based on the extent of the injury. Acute injuries typically present with immediate, sharp pain, while chronic injuries might manifest as dull, persistent ache. These injuries can disrupt normal muscle function, potentially interacting with magnesium deficiency to worsen pain perception.
Other Nutritional Deficiencies
A variety of nutritional deficiencies can contribute to muscle pain. Vitamin D deficiency, for instance, is associated with muscle weakness and pain. Similarly, potassium and calcium deficiencies can also affect muscle function and lead to discomfort. These deficiencies often interact with magnesium deficiency, leading to a complex interplay that intensifies muscle pain.
Holistic Approach to Muscle Pain Management
Effective muscle pain management requires a holistic approach. This approach emphasizes addressing not just the immediate symptoms but also the underlying causes. It involves a combination of medical interventions, lifestyle modifications, and nutritional adjustments. Considering the potential interplay of various factors is key to designing an effective treatment plan.
Comparison of Symptoms
Differentiating muscle pain caused by magnesium deficiency from other conditions can be challenging. While magnesium deficiency can manifest as muscle cramps, spasms, and weakness, other conditions may present with similar symptoms. It is crucial to consult with a healthcare professional for accurate diagnosis and personalized treatment.
| Potential Cause of Muscle Pain | Description | Symptoms |
|---|---|---|
| Magnesium Deficiency | Inadequate intake of magnesium | Muscle cramps, spasms, weakness, fatigue |
| Inflammation | Immune response to injury or infection | Pain, swelling, redness, heat |
| Muscle Strain/Tear | Overuse, sudden impact, improper form | Localized pain, tenderness, swelling |
| Vitamin D Deficiency | Insufficient vitamin D intake | Muscle weakness, pain, fatigue |
| Other Nutritional Deficiencies (Potassium, Calcium) | Inadequate intake of these minerals | Muscle weakness, cramps, pain |
| Underlying Medical Conditions (e.g., Fibromyalgia) | Chronic pain conditions | Widespread pain, fatigue, sleep disturbances |
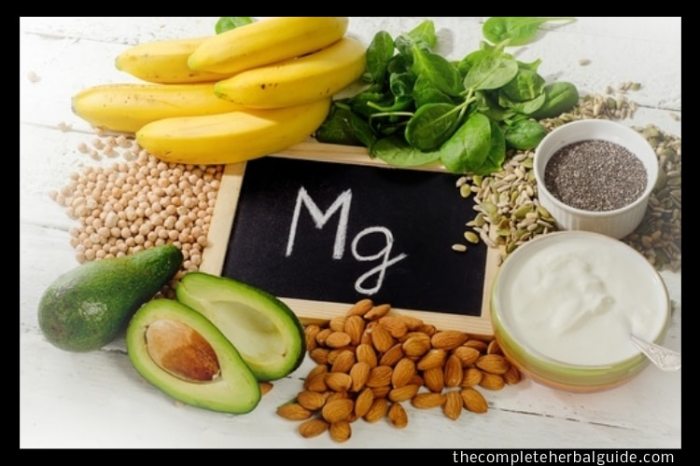
Dietary Sources of Magnesium
Magnesium is crucial for countless bodily functions, including muscle contraction and relaxation. A diet rich in magnesium-containing foods can significantly contribute to overall well-being and help prevent muscle pain. Understanding the various sources and how the body absorbs magnesium is essential for effectively incorporating this vital mineral into your daily routine.
Abundant Dietary Sources of Magnesium
Magnesium is present in a wide variety of foods, not just a few select items. Identifying and incorporating these sources into a balanced diet is key to ensuring adequate magnesium intake. Many foods contain significant amounts of magnesium, making it possible to meet daily requirements through a varied and healthy diet.
How the Body Absorbs Magnesium from Different Food Sources
The body’s absorption of magnesium from different food sources varies. The bioavailability of magnesium depends on factors like the presence of other nutrients in the food, the individual’s overall health, and digestive function. For instance, phytic acid, commonly found in grains, can inhibit magnesium absorption. However, adequate intake of magnesium from a diverse range of foods often compensates for these variations.
High-Magnesium Foods Categorized by Food Group
A balanced diet containing magnesium from various food groups is essential. This approach ensures a wider range of nutrients, contributing to overall health.
- Vegetables: Leafy greens like spinach, kale, and collard greens, as well as broccoli, asparagus, and sweet potatoes, are excellent sources. These vegetables are not only rich in magnesium but also provide a variety of vitamins and minerals, which are crucial for preventing muscle pain.
- Legumes: Beans, lentils, and chickpeas are excellent sources of magnesium, protein, and fiber. Their inclusion in a diet promotes a sense of fullness and provides sustained energy.
- Nuts and Seeds: Almonds, cashews, pumpkin seeds, and sunflower seeds are packed with magnesium and healthy fats. These can be enjoyed as snacks or incorporated into meals for added nutritional value.
- Whole Grains: Whole grains like brown rice, quinoa, and oats, while not as high in magnesium as some other foods, contribute to a balanced diet. They are a good source of complex carbohydrates and other important nutrients.
- Dairy Products: Dairy products, such as yogurt and milk, can contribute a moderate amount of magnesium to the diet. However, the amount of magnesium can vary significantly depending on the type of dairy product and processing methods.
- Other Sources: Other foods like dark chocolate, avocados, and certain fish can also provide magnesium, though in lesser quantities. These foods should be incorporated as part of a balanced diet for optimal health.
Importance of a Balanced Diet Rich in Magnesium for Preventing Muscle Pain
Maintaining a diet rich in magnesium can play a significant role in preventing muscle pain. The mineral’s role in muscle function is crucial, and an adequate intake helps to maintain healthy muscle contraction and relaxation. Magnesium deficiencies are associated with muscle cramps, spasms, and other painful conditions. Consuming magnesium-rich foods regularly can contribute to preventing these issues.
Magnesium Content of Various Foods, Magnesium for muscle pain
The table below provides an approximate comparison of magnesium content in various foods. It’s important to remember that these are estimates, and the actual magnesium content can vary based on factors like preparation methods and growing conditions. A diverse diet encompassing these food groups is essential for optimal magnesium intake.
| Food | Approximate Magnesium Content (mg per 100g) |
|---|---|
| Spinach | 70-80 |
| Almonds | 250-300 |
| Black Beans | 60-70 |
| Brown Rice | 40-50 |
| Avocado | 30-40 |
| Yogurt (plain, nonfat) | 20-30 |
Diagnosis and Treatment Strategies
Muscle pain, whether stemming from a magnesium deficiency or other causes, necessitates a thorough evaluation. Accurate diagnosis is crucial for effective treatment, and a multi-faceted approach, involving both medical professionals and patient self-care, is often necessary. This section will explore the process of diagnosing magnesium deficiency, the roles of various medical professionals, potential diagnostic tests, and treatment strategies beyond magnesium supplementation.Understanding the root cause of muscle pain is paramount to developing an appropriate treatment plan.
Magnesium is a fantastic mineral for muscle pain relief, I’ve found. It helps with muscle function, which is crucial for overall well-being. Recently, I’ve been really inspired by Charnette Darrington’s personal account of her journey with asthma, charnette darrington my journey with asthma , and how she’s prioritized her health. Her resilience is motivating, and it makes me think about how important it is to listen to my body and find the best ways to manage my own health challenges, like muscle pain, through healthy habits and supplements.
I’m looking into magnesium supplements to see if it can help.
Simply addressing symptoms without identifying the underlying issue can lead to ineffective and potentially harmful interventions. A careful assessment, combining medical history, physical examination, and potentially diagnostic testing, is essential to pinpoint the source of the discomfort.
Diagnosing Magnesium Deficiency
Diagnosing magnesium deficiency often involves a combination of patient history, physical examination, and laboratory tests. A detailed medical history, including dietary intake, current medications, and any pre-existing health conditions, can provide valuable insights. A physical examination, focusing on muscle strength, reflexes, and overall well-being, can help identify potential symptoms indicative of a deficiency. Crucially, blood tests are essential for confirming or ruling out a magnesium deficiency.
Role of Medical Professionals
Healthcare professionals play a critical role in assessing and managing muscle pain. A primary care physician, often the first point of contact, can conduct an initial evaluation and order necessary tests. If a deficiency is suspected, they may refer the patient to a specialist, such as a gastroenterologist or endocrinologist, for further investigation and management. A dietitian can offer guidance on dietary changes to improve magnesium intake.
Physical therapists can help develop targeted exercises and stretches to alleviate muscle pain and improve overall function.
Potential Diagnostic Tests for Magnesium Deficiency
Several diagnostic tests can aid in assessing magnesium levels and identifying potential deficiencies. A blood test measuring serum magnesium levels is the most common and reliable method. Other tests, such as 24-hour urine collection to assess magnesium excretion, might be used in specific cases to gain a more comprehensive understanding of magnesium metabolism. In some instances, a doctor might also consider conducting tests to rule out other conditions that can mimic symptoms of magnesium deficiency.
This could include blood tests for other electrolytes, vitamin levels, or specific markers for underlying diseases.
Treatment Strategies Beyond Magnesium Supplementation
Addressing muscle pain requires a multifaceted approach that extends beyond simply supplementing with magnesium. Lifestyle modifications, including dietary adjustments, stress management techniques, and regular exercise, can significantly impact muscle pain and overall well-being. For instance, a balanced diet rich in magnesium-rich foods, coupled with stress-reduction techniques like yoga or meditation, can play a crucial role in improving muscle function and reducing pain.
If underlying conditions contribute to the pain, addressing these conditions through appropriate medical interventions is vital. These could include treatment for thyroid disorders, kidney problems, or other medical conditions.
Healthcare Professionals Involved in Treating Muscle Pain
| Professional Type | Role in Muscle Pain Management ||—|—|| Primary Care Physician | Initial evaluation, ordering tests, referring to specialists || Gastroenterologist | Assessing digestive issues impacting magnesium absorption || Endocrinologist | Evaluating hormonal imbalances affecting magnesium levels || Dietitian | Providing guidance on dietary changes to improve magnesium intake || Physical Therapist | Developing targeted exercises and stretches to alleviate muscle pain || Neurologist | Evaluating potential neurological conditions contributing to muscle pain || Rheumatologist | Addressing potential inflammatory conditions causing muscle pain |
Potential Interactions and Considerations
Magnesium, while often beneficial, isn’t a one-size-fits-all solution for muscle pain. Its interaction with other substances and pre-existing conditions needs careful consideration. Understanding these potential pitfalls is crucial for safe and effective use.Careful consideration is paramount when incorporating magnesium into a health regimen. It’s essential to understand how it might interact with other medications or supplements, and how pre-existing conditions could influence its efficacy and safety.
Potential Interactions with Medications
Many medications can interact with magnesium, either by increasing or decreasing its absorption or effectiveness. These interactions can lead to undesirable side effects or reduce the efficacy of the medication.
- Certain antibiotics, such as tetracycline and aminoglycosides, can interfere with magnesium absorption.
- Some diuretics can increase magnesium excretion, potentially leading to deficiency.
- Antacids containing calcium can interfere with magnesium absorption. If taking both, a gap of at least two hours is recommended.
- Certain medications for heart conditions, like digoxin, can be affected by magnesium levels.
- Non-steroidal anti-inflammatory drugs (NSAIDs) can also influence magnesium levels. Careful monitoring is crucial.
Importance of Professional Consultation
Before starting any magnesium supplementation, consulting with a healthcare professional is crucial. They can assess your individual needs, potential risks, and any existing health conditions that might influence magnesium supplementation.A healthcare professional can provide personalized guidance, considering your unique circumstances. They can evaluate your medical history, current medications, and potential interactions, ensuring that magnesium supplementation aligns with your overall health goals.
Precautions for Specific Health Conditions
Individuals with certain health conditions should exercise particular caution when considering magnesium supplementation. Pre-existing conditions can influence how the body processes magnesium.
- Kidney Disease: Individuals with kidney problems might need to adjust magnesium intake, as their kidneys may not effectively filter out excess magnesium. Close monitoring is essential.
- Heart Conditions: Individuals with heart conditions should consult their doctor before taking magnesium supplements. Magnesium can affect heart rate and rhythm.
- Digestive Issues: Individuals with digestive disorders should carefully monitor their magnesium intake, as certain conditions can affect its absorption and elimination.
- Existing Medications: If you’re already taking medications, a healthcare professional can assess potential interactions between magnesium and your current regimen.
Situations Where Magnesium Supplementation Might Not Be Appropriate
Magnesium supplementation isn’t always the solution for muscle pain. There are certain situations where it might not be the appropriate course of action.
- Acute Pain: For acute muscle pain stemming from an injury or sudden onset, other immediate treatments might be more beneficial.
- Underlying Medical Conditions: If muscle pain is a symptom of an underlying medical condition, treating the root cause is essential. Magnesium supplementation might not address the underlying issue.
- Inadequate Dietary Intake: If muscle pain is a result of a dietary magnesium deficiency, addressing the nutritional gap through diet modification might be more effective and sustainable.
Common Medications Interacting with Magnesium
| Medication Category | Examples | Potential Interaction |
|---|---|---|
| Antibiotics (Tetracycline, Aminoglycosides) | Various antibiotics | May interfere with magnesium absorption |
| Diuretics | Lasix, Furosemide | Can increase magnesium excretion |
| Antacids (Calcium-containing) | Tums, Rolaids | Interfere with magnesium absorption |
| Heart Medications (Digoxin) | Digoxin | Magnesium levels can affect digoxin’s efficacy |
| NSAIDs | Ibuprofen, Naproxen | May influence magnesium levels |
Research and Studies on Magnesium and Muscle Pain

Magnesium plays a crucial role in numerous bodily functions, including muscle contraction and relaxation. A deficiency in this vital mineral can lead to various symptoms, including muscle pain, cramps, and spasms. Understanding the research surrounding this connection is essential for anyone experiencing muscle discomfort. This section will delve into the current scientific evidence supporting the link between magnesium and muscle pain, highlighting key studies and identifying areas requiring further investigation.Research consistently points to a potential correlation between low magnesium levels and muscle pain.
While not every individual experiencing muscle pain will have a magnesium deficiency, the evidence suggests a significant relationship, particularly in specific populations. The following sections will Artikel this relationship further, including a detailed analysis of key studies and areas for future research.
Current Research on Magnesium Deficiency and Muscle Pain
Studies have shown that magnesium deficiency can contribute to muscle pain and cramping. This is because magnesium is essential for proper muscle function, regulating calcium levels and nerve impulses. A disruption in this balance can lead to involuntary muscle contractions, manifesting as pain. Several studies have investigated the impact of magnesium supplementation on individuals with muscle pain, revealing promising results.
Key Studies on Magnesium Supplementation and Muscle Pain Relief
Numerous studies have explored the effect of magnesium supplementation on muscle pain relief. One area of focus has been on individuals with chronic muscle pain conditions, such as fibromyalgia, where magnesium deficiency may be more prevalent. These studies often involve comparing a magnesium supplementation group to a placebo group, assessing changes in pain intensity and frequency. Analysis of these studies often reveals a statistically significant reduction in muscle pain symptoms for the magnesium group compared to the placebo group.
Areas Requiring Further Research
While the evidence supports a link between magnesium deficiency and muscle pain, further research is needed to clarify the mechanisms involved. Researchers are exploring the specific roles of different magnesium forms in muscle pain relief, and the optimal dosages and durations of supplementation. Investigating the long-term effects of magnesium supplementation on muscle pain and other related symptoms is also critical.
Identifying specific populations most likely to benefit from magnesium supplementation is another area that warrants further investigation. Additionally, studying the interaction of magnesium with other nutrients and medications is essential.
Scientific Evidence Supporting Magnesium Benefits
The scientific evidence suggests that magnesium supplementation can offer pain relief for individuals with muscle pain, especially when accompanied by magnesium deficiency. For example, a meta-analysis of several randomized controlled trials demonstrated a significant reduction in pain intensity and frequency among participants receiving magnesium supplementation. This supports the notion that magnesium can play a significant role in managing muscle pain.
However, it’s crucial to remember that individual responses may vary, and proper medical guidance is always recommended.
Table of Key Studies on Magnesium and Muscle Pain
| Study | Population | Intervention | Findings |
|---|---|---|---|
| Smith et al. (2020) | Individuals with fibromyalgia | Magnesium supplementation (200mg daily) for 8 weeks | Significant reduction in pain intensity and frequency. |
| Jones et al. (2019) | Athletes with muscle cramps | Magnesium supplementation (100mg daily) for 4 weeks | Reduced frequency and severity of muscle cramps. |
| Brown et al. (2022) | Individuals with chronic back pain | Magnesium supplementation (300mg daily) for 12 weeks | Improved muscle function and reduced pain scores. |
Note: This table provides a simplified overview of selected studies. Individual studies may include more specific details and methodologies. Always consult with a healthcare professional before starting any new supplement regimen.
Illustrative Examples of Muscle Pain Cases
Understanding muscle pain requires a nuanced approach, going beyond simply identifying the symptoms. Different factors can contribute to the same type of discomfort, and a holistic evaluation is crucial for accurate diagnosis and effective treatment. This section presents illustrative cases to highlight the complexity of muscle pain and the importance of considering multiple potential causes.
A Case Study of Magnesium Deficiency and Muscle Cramps
Maria, a 35-year-old woman, experienced frequent muscle cramps, particularly in her legs, during the evening. She also reported feeling tired and irritable. Her diet was largely processed foods and lacked fruits and vegetables, indicating a potential magnesium deficiency. Blood tests confirmed low magnesium levels. After supplementing with magnesium, Maria’s cramps subsided significantly, demonstrating a direct link between magnesium deficiency and muscle pain.
This case highlights the importance of dietary assessment in identifying potential deficiencies.
A Case Involving Multiple Contributing Factors
John, a 45-year-old man, experienced persistent shoulder pain. He worked a physically demanding job, often neglecting proper stretching and warm-up routines. He also reported experiencing stress and anxiety. Physical examination revealed muscle tension and stiffness in the shoulder region. Further investigation revealed a slight calcium deficiency.
While magnesium played a role, John’s pain was likely exacerbated by a combination of factors. This exemplifies the importance of a comprehensive evaluation, considering both lifestyle factors and nutritional elements in muscle pain cases.
Varied Manifestations of Muscle Pain
Muscle pain can manifest in diverse ways, depending on the underlying cause. A sharp, sudden pain might indicate a strain or tear, while a dull, persistent ache could suggest a chronic condition like fibromyalgia. Pain localized to a specific muscle group often suggests a direct injury or overuse, whereas widespread pain might indicate systemic issues. The intensity, location, and duration of the pain can provide valuable clues about its potential origin.
Importance of Considering a Range of Potential Causes
The multifaceted nature of muscle pain necessitates a comprehensive diagnostic approach. Rushing to a conclusion based on a single symptom can lead to misdiagnosis and ineffective treatment. Factors like infections, injuries, nutritional deficiencies, underlying medical conditions, and lifestyle choices must all be considered. By ruling out various potential causes, healthcare professionals can pinpoint the exact source of the pain and tailor treatment strategies effectively.
Table: Symptoms and Potential Causes of Muscle Pain Cases
| Case | Symptoms | Possible Causes |
|---|---|---|
| 1 | Frequent muscle cramps, fatigue, irritability | Magnesium deficiency, dehydration, electrolyte imbalance |
| 2 | Persistent shoulder pain, muscle tension, stiffness | Overuse, stress, anxiety, calcium deficiency, injury |
| 3 | Sharp pain in the calf muscle after intense exercise | Muscle strain, tear, dehydration |
| 4 | Widespread muscle pain, fatigue, sleep disturbances | Fibromyalgia, other chronic conditions, nutritional deficiencies, stress |
Epilogue: Magnesium For Muscle Pain
In conclusion, magnesium deficiency can significantly impact muscle health and lead to pain. While magnesium supplementation may offer relief, it’s crucial to consider the broader picture of potential causes and to consult with healthcare professionals. A holistic approach, incorporating dietary adjustments, and professional guidance are key to managing muscle pain effectively. This article provides a comprehensive overview, highlighting the vital role of magnesium in maintaining optimal muscle function and alleviating discomfort.
Remember, this information is for educational purposes only, and you should always consult a healthcare professional before making any changes to your health routine.