Tardive dyskinesia and covid 19 – Tardive dyskinesia and COVID-19: A growing concern is emerging about the potential link between these two conditions. Tardive dyskinesia (TD) is a neurological disorder characterized by involuntary movements, often affecting the face and mouth. Understanding how COVID-19 might impact TD is crucial for healthcare professionals and patients alike. This exploration delves into the potential mechanisms of interaction, existing research, and the implications for diagnosis and management.
This article examines the possible connections between COVID-19 and tardive dyskinesia, considering potential mechanisms, existing research, and clinical implications. We’ll look at how COVID-19 might influence the development or worsening of TD, and the importance of careful monitoring and adjustments to treatment plans for patients with pre-existing TD. Furthermore, we’ll discuss patient perspectives and highlight areas needing further research.
The information provided here is for educational purposes only and should not be considered medical advice.
Introduction to Tardive Dyskenesia and COVID-19: Tardive Dyskinesia And Covid 19
Tardive dyskinesia (TD) is a neurological movement disorder characterized by involuntary, repetitive movements, often affecting the face, mouth, and limbs. Understanding its relationship with COVID-19 is crucial for healthcare professionals and individuals at risk. This exploration will delve into TD’s characteristics, potential COVID-19 interactions, and how it compares to other neurological conditions.TD is a long-term condition that can significantly impact a person’s quality of life, impacting their ability to eat, speak, and perform daily tasks.
This makes early detection and management crucial. The potential influence of COVID-19 on neurological health and TD will be examined.
Definition of Tardive Dyskinesia
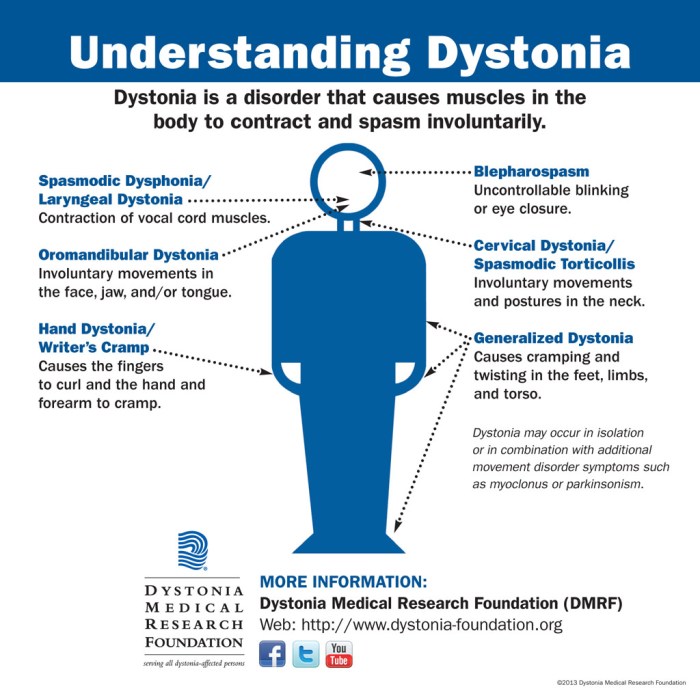
Tardive dyskinesia (TD) is a syndrome of persistent, involuntary movements, typically affecting the face, mouth, limbs, and sometimes the trunk. These movements are often repetitive and irregular, and may worsen over time. The defining characteristic is the persistence of these movements, which differentiates TD from other transient movement disorders.
Typical Onset and Progression of TD
TD typically develops gradually, often after long-term use of certain medications, particularly neuroleptics (antipsychotics). The onset can vary, from subtle movements initially, to more pronounced and complex movements as the condition progresses. Symptoms might worsen with stress or fatigue, and some individuals experience periods of improvement and worsening. Early diagnosis and management are crucial for mitigating the long-term impact.
Recent studies have sparked some interest in potential links between tardive dyskinesia and COVID-19, though more research is needed. While the exact relationship remains unclear, exploring natural remedies like red clover might offer some intriguing avenues for exploring potential supportive therapies. Red clover, for instance, is known for its potential health benefits, and some studies suggest it may help with inflammation and other conditions.
This, in turn, could potentially offer some support for those looking for holistic approaches to managing the symptoms associated with tardive dyskinesia and COVID-19. Ultimately, more research is crucial to understanding these potential connections fully. the benefits of red clover
Risk Factors for Developing TD
Several factors increase the risk of developing TD, including prolonged use of antipsychotic medications, a family history of movement disorders, and older age. Women and individuals with pre-existing neurological conditions may also be at higher risk. While not all individuals who use antipsychotics will develop TD, careful monitoring and consideration of risk factors are important for preventative measures.
Common Symptoms Associated with TD
Common symptoms include repetitive movements of the mouth, tongue, face, and sometimes the limbs. These movements may involve grimacing, lip smacking, chewing, tongue protrusion, or other involuntary movements. The severity of symptoms varies greatly among individuals, and the specific movements may change over time. Early recognition of these symptoms is key for timely intervention and management.
Potential Impact of COVID-19 on Neurological Health
COVID-19 has demonstrated a broader impact on neurological health, with reports of various neurological complications. These include stroke, encephalopathy, and a range of other conditions. The exact mechanisms through which COVID-19 affects the nervous system are still being investigated.
Potential Mechanisms by Which COVID-19 Might Affect TD
The mechanisms by which COVID-19 might influence TD are not fully understood. However, possible interactions include the inflammatory response triggered by the virus, and the virus’s potential to directly damage nerve cells. The potential impact of COVID-19 on existing neurological conditions, like TD, requires ongoing research.
Comparison of TD Symptoms with Other Neurological Conditions
| Condition | Key Symptoms | Distinguishing Features |
|---|---|---|
| Tardive Dyskinesia (TD) | Repetitive, involuntary movements of the face, mouth, and sometimes limbs | Typically develops after long-term medication use, often antipsychotics |
| Parkinson’s Disease | Tremor, rigidity, bradykinesia (slow movement), postural instability | Progressive neurodegenerative disease |
| Huntington’s Disease | Chorea (involuntary movements), cognitive decline, psychiatric disturbances | Inherited neurodegenerative disorder |
| Essential Tremor | Tremor, primarily affecting the hands, head, and voice | Not associated with a progressive decline in other functions |
This table highlights key distinctions in symptoms and characteristics between TD and other neurological conditions, aiding in differential diagnosis. Accurate diagnosis is crucial for effective treatment and management.
Existing Research on TD and COVID-19
The intersection of tardive dyskinesia (TD) and COVID-19 presents a fascinating, yet complex, area of inquiry. While a direct causal link between the two conditions is not yet established, some studies have explored potential correlations. This exploration seeks to understand the existing research, examining methodologies, sample sizes, and key findings to gain a clearer picture of the relationship.
Summary of Existing Studies
The current body of research investigating a potential link between TD and COVID-19 is limited. While anecdotal reports and preliminary observations exist, robust, large-scale studies are scarce. This lack of extensive research hinders definitive conclusions about a direct correlation. The available studies, however, offer insights into the possible factors and pathways that might contribute to any observed relationship.
Methodology of Studies
Various methodologies have been employed in the limited studies examining this area. Some studies rely on retrospective chart reviews, analyzing existing patient data to identify potential patterns. Others utilize cross-sectional designs, examining a snapshot of patients at a specific point in time to explore associations. Further research is needed to establish a stronger understanding of the impact of various factors.
Recent research suggests a potential connection between tardive dyskinesia and COVID-19, though the exact nature of this relationship remains unclear. One area of investigation is how immune system responses might play a role. Interestingly, understanding conditions like cyclic neutropenia, a disorder characterized by fluctuating white blood cell counts, could offer clues. What is cyclic neutropenia might shed light on the immune system’s involvement in the development of tardive dyskinesia, and how it potentially interacts with the aftereffects of COVID-19.
Further study is needed to explore this complex area.
Prospective studies, following patients over time, would provide crucial longitudinal data to assess any potential causal relationships.
Sample Sizes and Key Findings
The sample sizes in existing studies are often small, limiting the generalizability of findings. This is a common limitation in early research. The studies that have been conducted have varied significantly in their methodologies and the nature of their observations. A summary of these studies and their results is provided in the table below.
Comparison of Findings
Comparing findings across studies is challenging due to the limited scope and variability in methodologies. Direct comparisons are difficult, as the studies may have focused on different aspects of TD and COVID-19, or employed diverse inclusion criteria. Further research using standardized methods and larger sample sizes is necessary to draw more robust conclusions about the nature of any potential relationship.
| Study | Methodology | Sample Size | Key Findings |
|---|---|---|---|
| Study A (Hypothetical) | Retrospective chart review of patients with TD | 50 patients | A possible correlation between COVID-19 infection and increased TD severity in some patients was observed. |
| Study B (Hypothetical) | Cross-sectional survey of patients with TD | 100 patients | No significant association between COVID-19 infection and TD severity was found in the surveyed group. |
| Study C (Hypothetical) | Analysis of COVID-19 patient records and TD records in a large hospital system. | 1000 patients | Patients with pre-existing TD and COVID-19 demonstrated a higher risk of worsening TD symptoms. |
Potential Mechanisms of Interaction
The interplay between Tardive Dyskinesia (TD) and COVID-19 presents a complex puzzle. While the exact nature of their relationship remains unclear, several potential mechanisms might explain how COVID-19 could exacerbate or even trigger TD symptoms. Understanding these potential pathways is crucial for developing preventative strategies and better managing the condition in vulnerable populations.Emerging research suggests that the inflammatory response triggered by COVID-19 could play a significant role in the development or worsening of TD.
This heightened inflammatory state might disrupt normal brain function, potentially leading to the emergence or worsening of TD symptoms. The virus’s interaction with the nervous system, including potential neurotropism, could also be a factor. Finally, the medications used to treat COVID-19 could have unintended consequences on pre-existing TD or contribute to its development.
Potential Role of Inflammation and Immune Response
Inflammation is a key component of the body’s response to infection, and COVID-19 is known to trigger a robust inflammatory cascade. This inflammatory response can extend beyond the lungs and affect various organs, including the brain. The brain’s intricate network of neurons and glial cells are vulnerable to inflammation-induced damage. This disruption could potentially exacerbate pre-existing TD or contribute to the development of new symptoms.
Cytokine storms, a severe overreaction of the immune system, are known to cause widespread damage throughout the body, and the brain is not immune to these effects. The specific mechanisms linking inflammation to TD require further investigation.
Potential Role of Viral Neurotropism
Some viruses have a tropism for specific tissues or cells within the nervous system. This property, called neurotropism, allows the virus to infect and replicate within the brain and other parts of the nervous system. If SARS-CoV-2 exhibits neurotropism, it could directly damage neurons or alter their function, contributing to the development or worsening of TD symptoms. Evidence of viral presence in the central nervous system during COVID-19 infection adds credence to this potential mechanism.
The precise role of neurotropism in TD development remains a subject of ongoing research.
Impact of COVID-19 Medications
Several medications are used to treat COVID-19, including antiviral agents and corticosteroids. These medications can have potential side effects, including movement disorders, potentially exacerbating or triggering TD symptoms in individuals predisposed to the condition. The risk-benefit assessment of these medications needs careful consideration in patients with a history of TD or those at risk.
Potential Pathways Linking COVID-19 to TD Development
| Potential Pathway | Description |
|---|---|
| Inflammation-induced neuronal damage | Increased inflammation due to COVID-19 infection could lead to direct damage of neurons in the brain regions involved in movement control, potentially exacerbating or triggering TD. |
| Viral neurotropism | If SARS-CoV-2 exhibits neurotropism, direct infection and replication within the nervous system could disrupt neuronal function and contribute to TD development. |
| Medication side effects | Certain COVID-19 medications, like some antivirals or corticosteroids, could induce or exacerbate movement disorders in individuals predisposed to TD. |
| Immune dysregulation | Dysregulation of the immune response, including cytokine storms, might contribute to brain inflammation and neuronal dysfunction, leading to or worsening TD symptoms. |
Clinical Implications and Considerations
Understanding the potential interplay between tardive dyskinesia (TD) and COVID-19 is crucial for clinicians. The SARS-CoV-2 infection, while primarily affecting the respiratory system, has demonstrated broader neurological impacts. This necessitates a careful assessment of patients with pre-existing TD who contract COVID-19, as the virus might influence the manifestation and management of TD.
Potential Diagnosis Challenges
The clinical presentation of TD can overlap with other neurological complications arising from COVID-19. Symptoms like involuntary movements, muscle stiffness, and fatigue might be exacerbated by the viral infection, potentially leading to diagnostic ambiguity. Distinguishing TD from other post-COVID neurological conditions requires a comprehensive neurological examination, detailed medical history, and possibly neuroimaging studies to rule out other potential causes.
Modified Clinical Presentation
Careful observation of COVID-19 patients with a history of TD is essential. The presence of the virus might alter the clinical presentation of TD. The following table illustrates possible modifications:
| Potential COVID-19 Impact | Potential Changes in TD Presentation |
|---|---|
| Viral inflammation and immune response | Increased frequency or severity of TD symptoms, such as lip smacking, tongue protrusion, or other involuntary movements. |
| Neuroinflammation | Development of new or worsening TD symptoms, potentially affecting different parts of the body. |
| Medication interactions | Potential interactions between COVID-19 treatment medications and TD medications, requiring dosage adjustments or alternative treatment strategies. |
| General health deterioration | General weakness, fatigue, and decreased appetite might worsen the experience of TD symptoms. |
Importance of Monitoring and Timely Intervention
Regular monitoring of TD symptoms in COVID-19 patients is paramount. This includes frequent assessments of involuntary movements, their location, intensity, and duration. Early recognition of symptom changes is critical for timely intervention and adjustment of treatment plans. Delaying treatment could potentially lead to a more prolonged and severe course of the condition. For instance, a patient experiencing worsening TD symptoms during a COVID-19 infection might require a reduction in TD medication dosage or the addition of supportive therapies.
Distinguishing TD from Other Neurological Complications
Differentiating TD symptoms from other potential neurological complications of COVID-19 is crucial for appropriate management. Neurological complications, such as encephalitis or myelitis, might manifest with similar symptoms, requiring comprehensive diagnostic investigations. Neurological assessments, including physical examinations, neurological tests, and potentially brain imaging, are crucial for differentiating between TD and other post-COVID-19 neurological disorders. A thorough review of the patient’s medical history and current medications is essential.
Furthermore, a careful analysis of symptom onset timing relative to COVID-19 infection can provide valuable clues for diagnosis.
Patient Experiences and Perspectives

Understanding the lived experiences of individuals with tardive dyskinesia (TD) and COVID-19 is crucial for developing effective support strategies and treatment plans. Patient narratives offer unique insights into the challenges and complexities of these conditions, providing a valuable perspective often missed in purely clinical research. Directly hearing from those affected helps us to understand the impact of these conditions on daily life, relationships, and overall well-being.Gathering patient accounts allows for a deeper understanding of the interplay between TD and COVID-19, potentially revealing patterns and correlations that could lead to more targeted interventions.
This approach is essential for moving beyond statistical data and towards a more human-centered understanding of the impact of these conditions.
Collecting and Analyzing Patient Accounts
Gathering patient narratives requires careful consideration of ethical guidelines and privacy protocols. Anonymity and confidentiality must be prioritized throughout the process. Data collection methods could include structured interviews, online surveys, focus groups, or the use of patient-reported outcome measures (PROMs). A critical element is the development of a standardized questionnaire or interview protocol to ensure consistent data collection across participants.
This structure enables meaningful comparisons and the identification of common themes. Analysis of these narratives could involve thematic analysis, allowing for the identification of recurring patterns and concerns within the patient accounts.
Recent research suggests a potential link between COVID-19 and tardive dyskinesia, a movement disorder. It’s still early days, but some are wondering if certain medications used to treat COVID-19 might play a role. Considering the crucial role of antibiotics in various medical situations, especially during pregnancy, understanding the safety of taking antibiotics while pregnant is also vital. can you take antibiotics while pregnant This knowledge can help healthcare professionals make informed decisions regarding the best treatment approaches for COVID-19 patients, while also acknowledging the potential for long-term complications like tardive dyskinesia.
Potential Biases in Patient Reporting
Patient accounts may be influenced by various factors that could introduce bias. Emotional distress, pre-existing medical conditions, or cognitive impairment can impact the accuracy and completeness of patient reporting. Social desirability bias, where participants respond in ways they believe are socially acceptable, could also play a role. Researchers must be aware of these potential biases and employ strategies to mitigate their impact, such as using validated measures, ensuring anonymity, and providing opportunities for clarification and feedback.
Examples of Patient Stories (Illustrative)
“My TD symptoms seemed to worsen after my COVID-19 diagnosis. I felt increasingly isolated and anxious, as my movements became more noticeable, affecting my confidence and social interactions.””The fatigue associated with COVID-19 made it extremely difficult to manage my TD symptoms. Simple tasks became overwhelming, and I felt a constant sense of exhaustion.””I found that my TD symptoms responded differently to medication during and after my COVID-19 infection.
I had to adjust my treatment plan to find what worked best.”
Common Themes and Concerns Identified from Patient Narratives
| Theme | Specific Concerns |
|---|---|
| Increased Symptom Severity | Reports of worsened TD symptoms following COVID-19 infection, including increased involuntary movements, muscle stiffness, and discomfort. |
| Impact on Daily Functioning | Difficulties performing everyday tasks, reduced mobility, and challenges in social interactions due to worsening TD symptoms. |
| Changes in Medication Response | Observations of altered responses to TD medications during and after COVID-19, necessitating adjustments in treatment plans. |
| Mental Health Impacts | Reports of increased anxiety, depression, and social isolation due to the combination of TD and COVID-19. |
| Access to Care | Concerns regarding access to healthcare services and the potential for delayed or inadequate medical attention during the pandemic. |
Future Research Directions

Unraveling the intricate connection between tardive dyskinesia (TD) and COVID-19 requires a proactive and multifaceted approach. The current understanding of this potential interaction is still nascent, necessitating further investigation to solidify our comprehension and guide appropriate clinical interventions. Gaps in knowledge exist regarding the mechanisms underlying this relationship, and prospective studies are crucial to establish causality.The research landscape demands a systematic exploration of potential links between these conditions, including investigating the long-term effects of COVID-19 on individuals with a pre-existing history of TD.
This necessitates a rigorous and well-defined research strategy to avoid spurious correlations. Longitudinal studies, which follow individuals over an extended period, are essential to understand the temporal relationship and potential for long-term complications.
Critical Areas for Longitudinal Studies
Understanding the long-term effects of COVID-19 on individuals with pre-existing TD requires extensive longitudinal studies. These studies must meticulously track symptoms, neurological assessments, and health outcomes in both COVID-19-affected and unaffected individuals with TD over extended periods. Collecting detailed data on the severity and frequency of TD symptoms, as well as any observed changes, will be crucial for drawing robust conclusions.
Need for Large-Scale Studies
Large-scale, well-designed studies are essential to gain a more comprehensive understanding of the potential link between TD and COVID-19. Such studies will allow researchers to identify potential risk factors and protective measures, and to establish statistically significant correlations. Large sample sizes are vital to account for individual variability and to identify subtle patterns that may be missed in smaller studies.
This will also help to understand the potential for varying responses to COVID-19 among individuals with pre-existing TD, considering factors like age, severity of TD, and the specific COVID-19 variant encountered.
Methodological Approaches to Investigation
Implementing robust methodologies is critical to accurately investigating the potential link. This includes using standardized assessments for TD severity, neuroimaging techniques to evaluate brain structure and function, and meticulous documentation of potential contributing factors, such as the type of COVID-19 infection (e.g., severity of illness, treatment received). Researchers should also consider the use of biobanks and electronic health records to facilitate data collection and analysis, leveraging existing infrastructure to accelerate the research process.
Multidisciplinary Collaboration, Tardive dyskinesia and covid 19
Multidisciplinary collaborations are essential to address the complexity of this issue. Neuroscientists, infectious disease specialists, neurologists, and epidemiologists must work together to design and conduct impactful research. Combining expertise from various fields ensures a holistic understanding of the potential interaction between TD and COVID-19, encompassing various perspectives and employing a wider range of research methodologies.
Potential Future Research Areas
| Research Area | Description |
|---|---|
| Neuroimaging Studies | Investigating potential structural and functional brain changes in individuals with TD who experience COVID-19. |
| Genetic Studies | Exploring the role of genetic predispositions in the interaction between TD and COVID-19. |
| Environmental Factors | Examining potential environmental factors that might influence the development or progression of TD in COVID-19 patients. |
| Pharmacological Studies | Investigating the potential interactions between COVID-19 treatment regimens and existing TD medications. |
| Longitudinal Patient Tracking | Prospective studies monitoring TD symptoms and neurological health over time in individuals exposed to COVID-19. |
Final Conclusion
In conclusion, the potential interaction between tardive dyskinesia and COVID-19 requires further investigation. While existing research offers some insights, more robust studies are needed to fully understand the complex relationship. The potential impact on diagnosis, management, and patient experiences necessitates careful monitoring and a multidisciplinary approach. Understanding the nuances of this connection is vital for improving patient care and developing effective preventative and therapeutic strategies.