The functional reach test in physical therapy sets the stage for understanding a crucial assessment tool for evaluating functional mobility. This test is used to measure the distance a person can reach forward from a standing position, providing valuable insights into balance and potential risks of falls. Understanding the test’s purpose, administration, interpretation, and limitations is essential for physical therapists and their patients.
This comprehensive guide explores the functional reach test, delving into its various applications, including specific patient populations. We will discuss the necessary equipment, step-by-step procedures, and standardized measurements. Furthermore, we’ll analyze how to interpret results, identify potential limitations, and highlight safety precautions.
Introduction to the Functional Reach Test
The Functional Reach Test (FRT) is a simple, yet insightful, clinical assessment tool used in physical therapy to evaluate an individual’s ability to reach forward. It measures the maximum distance a person can reach forward while maintaining a stable stance. This test provides valuable information about postural stability and functional mobility, particularly in individuals with conditions that impact balance and movement.The FRT is valuable because it assesses a person’s ability to maintain balance during a functional movement.
This is crucial for identifying potential impairments that might affect daily activities like reaching for objects, walking, or transferring. The test’s simplicity and quick administration make it a practical tool for both initial assessments and monitoring progress during rehabilitation.
Purpose and Rationale
The FRT’s purpose is to quantitatively assess the functional mobility of an individual, focusing on the ability to maintain balance while performing a forward reach. This is particularly relevant in evaluating individuals who experience postural instability or decreased mobility due to various conditions. By understanding the individual’s functional reach, clinicians can identify areas needing improvement and tailor rehabilitation strategies accordingly.
Contexts of Utilization
The FRT is commonly used in various clinical settings. It’s frequently employed in assessing individuals with balance disorders, such as those resulting from stroke, Parkinson’s disease, multiple sclerosis, and other neurological conditions. It is also helpful in evaluating individuals with musculoskeletal conditions that affect balance and movement, like osteoarthritis and spinal injuries. Further, it is used in geriatric assessments to evaluate mobility limitations associated with aging.
Moreover, it is utilized in pre and post-operative evaluations to monitor recovery from surgical procedures affecting balance and movement.
Clinical Significance in Assessing Functional Mobility
The FRT’s clinical significance lies in its ability to provide objective data about an individual’s functional reach. This data aids in identifying potential impairments in postural stability and functional mobility, helping clinicians tailor rehabilitation strategies. A shorter functional reach distance often indicates a higher risk of falls, highlighting the importance of interventions to improve balance and mobility. Furthermore, monitoring changes in functional reach over time allows clinicians to track the effectiveness of interventions and adjust treatment plans accordingly.
Equipment and Materials Required
The FRT requires minimal equipment, making it a practical and cost-effective assessment tool.
| Item | Description | Quantity | Notes |
|---|---|---|---|
| Measuring Tape or Ruler | A flexible measuring device, marked in centimeters or inches. | 1 | Ensure accuracy in measurement. |
| Marking Point | A non-movable marker to mark the starting point of the reach. | 1 | e.g., a piece of tape or a pen. |
| Standardized Instructions | Written or verbal instructions for the test. | 1 set | Ensure clear and consistent directions. |
| Safe and Stable Surface | A flat, non-slippery surface to perform the test. | 1 | e.g., a floor or a table. |
Administration of the Functional Reach Test
The Functional Reach Test (FRT) is a simple yet valuable assessment tool in physical therapy, providing insights into a patient’s balance and forward reach capabilities. Understanding how to administer the FRT accurately is crucial for obtaining reliable and meaningful results. This section details the step-by-step procedure, standardized protocols, and essential considerations for both the tester and the patient.The FRT evaluates an individual’s ability to reach forward while maintaining balance.
This capacity is essential for everyday activities like reaching for objects or preventing falls. A reduced functional reach distance often correlates with an increased risk of falls and impaired mobility.
Step-by-Step Procedure
The FRT procedure involves a series of specific steps. First, ensure the patient is standing with feet shoulder-width apart, maintaining a stable base. Then, instruct the patient to maintain an upright posture and relaxed stance, with arms hanging naturally at their sides. The tester should stand behind the patient, positioning the reacher at a distance of 20-30cm away from the patient’s center of gravity, ensuring it is aligned with their center of gravity and at the level of their mid-chest.
The functional reach test, a simple yet insightful assessment in physical therapy, measures how far a person can reach forward while maintaining balance. While focusing on balance and mobility, it’s important to consider dietary factors that can impact overall health, including the sometimes-overlooked issue of too much fiber in cholesterol lowering diets. A balanced approach to nutrition, as well as targeted exercises, is key to optimizing results, and the functional reach test can help gauge the effectiveness of those strategies.
This distance allows for a clear and precise measurement. Next, the patient is instructed to reach forward as far as possible while maintaining their balance. The distance is measured from the marked starting position to the furthest point reached by the patient’s fingertips, in centimeters.
Standardized Procedures
Standardized procedures for the FRT are crucial for consistency and comparability of results. These include specific instructions for the patient, ensuring that they understand the test’s purpose and how to perform it correctly. Consistent positioning of the reacher and the measurement tool are also vital for accurate results. Use of a calibrated and appropriate reacher is essential to maintain the accuracy of the test.
The functional reach test, a simple yet insightful physical therapy assessment, measures balance and mobility. It’s a great tool for gauging a patient’s ability to reach and maintain their balance. For those facing challenges after breast cancer treatment, finding the right support can be crucial, and ask an expert breast cancer patient resources is a fantastic place to connect with experienced professionals and gain valuable insights.
Ultimately, the functional reach test helps therapists understand a patient’s functional capabilities, paving the way for tailored rehabilitation plans.
Positioning and Body Mechanics
Correct positioning is essential for both the tester and the patient to ensure accuracy and safety. The tester should stand behind the patient, maintaining a stable stance and ensuring their body position does not interfere with the patient’s reach. The patient should be instructed to maintain a neutral posture, relaxed and centered, to avoid undue stress or strain on their joints or muscles.
Clear instructions and support can enhance the patient’s confidence and reduce any anxiety.
Variations and Modifications
| Variation | Description | Rationale | Considerations |
|---|---|---|---|
| Modified FRT for patients with impaired mobility | The patient may use assistive devices like a walker or cane. | Adapting the test to individual needs ensures a fair and meaningful assessment. | Proper usage of assistive devices should be supervised to avoid interference or undue strain. |
| FRT in a different environment (e.g., uneven surface) | Perform the test in a simulated real-life setting, considering factors like stairs or uneven terrain. | Provides a more realistic evaluation of the patient’s balance in various situations. | Ensure the environment is safe and controlled, considering potential fall risks. |
| FRT with visual or auditory distractions | Introduce controlled distractions during the test. | Assess the patient’s ability to maintain balance under conditions mimicking real-world scenarios. | Ensure the distractions are appropriate and not overly overwhelming for the patient. |
| FRT with different starting positions | Perform the test from different starting positions (e.g., standing on one leg). | Provides a more comprehensive assessment of balance capabilities. | Consider the patient’s capabilities and adjust accordingly. |
Recording and Documentation
Accurate documentation of the FRT results is essential for clinical decision-making and tracking progress. Record the patient’s name, date, time, and any relevant demographic information. Note the specific instructions provided to the patient. Document the patient’s starting position, the reacher position, and the distance reached. Include any observed deviations from the standardized procedure.
Any assistive devices used during the test and any visible signs of discomfort or distress should be documented.
Interpretation of Functional Reach Test Results
The Functional Reach Test (FRT) provides valuable insights into a patient’s postural stability and their ability to maintain balance during everyday activities. Understanding how to interpret FRT scores is crucial for developing effective treatment plans and predicting potential falls. Accurate interpretation involves considering the test’s limitations and potential influencing factors, alongside other assessments used in physical therapy.FRT scores are interpreted by comparing the measured reach distance to established norms or the individual’s baseline scores.
A lower reach distance generally indicates a greater risk of falls and functional limitations. This interpretation requires a holistic approach, taking into account the patient’s specific clinical presentation, medical history, and other functional assessments. The FRT is not a stand-alone assessment but a piece of a larger picture.
Factors Influencing FRT Results
Several factors can influence a patient’s FRT score, impacting the interpretation of the results. These factors include:
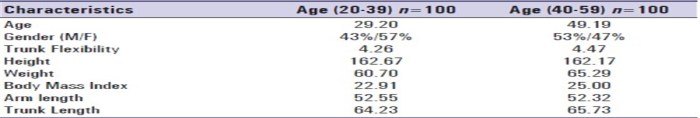
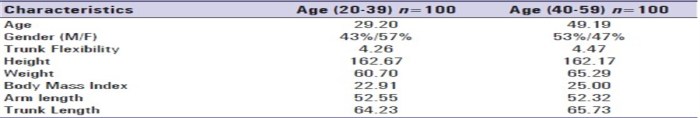
- Age and Gender: Older adults and females, generally, tend to have shorter functional reach distances compared to younger adults and males. This is a known physiological variation and should be considered when comparing scores.
- Underlying Medical Conditions: Conditions like arthritis, Parkinson’s disease, stroke, and other neurological impairments can significantly impact balance and postural stability, leading to lower FRT scores.
- Medication Effects: Certain medications can affect balance and coordination, potentially influencing the FRT results. This requires careful consideration in interpretation, especially for patients taking such medications.
- Previous Falls or Injuries: Patients with a history of falls or balance-related injuries often demonstrate lower FRT scores, reflecting a compromised ability to maintain equilibrium.
- Individual Variability: Individual variations in body composition, muscle strength, and flexibility also play a role in determining an individual’s FRT score. A patient’s baseline score and their improvements or declines over time are critical to the interpretation.
Comparison with Other Assessments, The functional reach test in physical therapy
The FRT complements other balance assessments, providing a more comprehensive picture of a patient’s functional status. Comparing FRT results with assessments like the Timed Up and Go (TUG) test, Berg Balance Scale (BBS), and the Single-Leg Stance Test can enhance the overall understanding of a patient’s balance abilities.
- TUG Test: A longer TUG time may correlate with a lower FRT score, suggesting greater difficulty with mobility and balance tasks.
- Berg Balance Scale: A lower BBS score often coincides with a lower FRT score, highlighting a significant relationship between balance confidence and reach ability.
- Single-Leg Stance Test: A shorter single-leg stance time frequently accompanies a lower FRT score, signifying a reduced ability to maintain balance in dynamic situations.
FRT Score Interpretation and Functional Limitations
The following table provides a general guideline for classifying FRT scores and their corresponding functional limitations. Remember, this is a general guideline, and individualized interpretation is crucial.
| FRT Score (cm) | Functional Limitations | Example Implications | Clinical Considerations |
|---|---|---|---|
| < 15 cm | Significant functional limitations, increased risk of falls, difficulty with daily activities. | A patient with a score below 15 cm might struggle with tasks like getting up from a chair, reaching for objects, or walking independently. | Close monitoring, increased support, and targeted interventions are necessary. |
| 15 – 20 cm | Moderate functional limitations, potential for falls, and some difficulty with daily tasks. | A patient with a score between 15 and 20 cm might experience some difficulty with balance during activities like stair climbing or navigating cluttered environments. | Balance training, gait retraining, and assistive devices might be helpful. |
| 21 – 25 cm | Mild functional limitations, less risk of falls, and minimal difficulty with daily tasks. | A patient with a score between 21 and 25 cm might have only slight balance challenges during everyday activities. | Continued monitoring and balance exercises are advisable. |
| > 25 cm | Minimal or no functional limitations, good balance, and minimal risk of falls. | A patient with a score above 25 cm likely has adequate balance and can perform daily activities with ease. | Focus on maintaining balance and preventing future issues. |
Applications and Limitations of the Functional Reach Test
The Functional Reach Test (FRT) is a valuable tool in physical therapy for assessing balance and fall risk. Understanding its specific applications, limitations, and comparison to other tests is crucial for clinicians to accurately interpret results and tailor interventions. This discussion will delve into the practical uses of the FRT across various patient populations, explore potential limitations, and examine its reliability and validity.The FRT, a simple yet informative test, provides clinicians with a quantitative measure of a patient’s ability to maintain balance during a forward reach.
This allows for a practical assessment of postural control and fall risk, particularly useful in identifying patients at risk for falls and evaluating the effectiveness of interventions. However, it is vital to understand the specific contexts in which the FRT is most appropriate and its inherent limitations.
Clinical Applications in Different Patient Populations
The FRT’s application extends to a wide range of patient populations. It’s particularly useful for individuals with balance disorders, such as those experiencing vestibular dysfunction, stroke, or Parkinson’s disease. The FRT can also be applied to older adults at risk for falls, athletes with balance deficits, and patients recovering from orthopedic surgeries. Its simplicity and quick administration make it suitable for frequent assessments within a variety of rehabilitation settings.
In geriatric populations, the FRT can identify individuals who may benefit from balance training exercises to improve stability and reduce fall risk.
Potential Limitations of the FRT
The FRT, while valuable, has certain limitations. One major limitation is its reliance on a single measurement. A single FRT score may not fully capture the complex nature of balance and postural control. External factors, such as the patient’s mood, fatigue level, or the specific day, can influence the results. The test environment itself can also affect performance.
For example, a cluttered or uneven surface could influence the results, and the test is not suitable for patients with severe cognitive impairments or visual deficits.
Reliability and Validity of the FRT
The reliability and validity of the FRT are crucial considerations for clinical use. Reliability refers to the consistency of the test, while validity refers to its ability to accurately measure what it intends to measure. Studies have shown that the FRT demonstrates good to excellent test-retest reliability, meaning that patients tend to obtain similar scores on repeated testing.
The FRT’s validity, however, is somewhat dependent on the specific population being tested and the context of the assessment.
Clinical Utility Compared to Other Balance Tests
The FRT complements other balance tests, rather than replacing them entirely. It offers a quick, simple, and portable assessment of functional reach, while other tests like the Timed Up and Go (TUG) or Berg Balance Scale (BBS) provide a more comprehensive evaluation of balance and functional mobility. The FRT can be used as a screening tool to identify individuals needing further assessment with more comprehensive balance tests.
For example, the FRT might suggest a patient requires a TUG to assess their overall mobility and functional balance.
Potential Areas for Future Research
Further research could focus on expanding the FRT’s application to different patient populations, such as those with specific neurological conditions. Investigating the impact of various environmental factors on FRT scores is another important area for research. Exploring the relationship between FRT scores and falls in diverse populations could also yield valuable insights into fall prevention strategies. Ultimately, continuing to refine the understanding of the FRT’s clinical utility and its limitations through research will enhance its application in clinical practice.
Safety Precautions and Considerations

The Functional Reach Test (FRT) is a valuable assessment tool, but proper safety precautions are crucial to ensure the well-being of the patient. Understanding potential risks and implementing mitigating strategies are paramount to a safe and accurate evaluation. This section details the necessary safety measures and considerations for administering the FRT.
The functional reach test, a simple yet insightful physical therapy assessment, measures your ability to reach forward. It’s all about how far you can comfortably extend your arm. Knowing this can help physical therapists gauge your balance and overall mobility. This ties in nicely with the concept of feeling full and satisfied after eating, which is something I’ve been exploring lately.
For example, foods high in fiber, like those listed on this great resource about foods that make you feel full , can help you feel more satiated. Ultimately, a strong sense of balance, both literally and figuratively, contributes to a more functional and active life, which is the core principle behind the functional reach test.
Safety Precautions During Administration
Careful observation and appropriate support are essential during the FRT. Ensure the patient has a stable and secure surface to perform the test. Provide adequate support to prevent falls or injuries, particularly for individuals with balance impairments. A physical therapist or trained professional should always be present during the FRT, capable of quickly intervening if necessary. Monitoring the patient’s posture and balance throughout the test is critical to identify any signs of instability or discomfort.
Potential Risks and Complications
Potential risks associated with the FRT include falls, injuries to the back or extremities, and exacerbation of existing medical conditions. Individuals with a history of falls, severe balance disorders, or recent surgeries may be at increased risk. Falls can result in fractures, sprains, or other musculoskeletal injuries. For example, a patient with a history of vertebral compression fractures might experience further pain or instability during the reach.
The FRT should be performed with caution, especially for individuals at high risk.
Minimizing Risks During the Test
Several strategies can be employed to minimize the risk of injury during the FRT. Providing a stable surface and ensuring the patient feels secure is critical. Assisting the patient with maintaining their balance during the test and offering verbal encouragement can significantly reduce the risk of falls. Proper positioning, especially in individuals with limited mobility, is vital.
The therapist should be prepared to intervene promptly if necessary. This includes having a means of immediate support and assistance readily available.
Contraindications for the Functional Reach Test
The following table Artikels potential contraindications for performing the FRT. Careful consideration of these factors is essential to ensure patient safety.
| Category | Specific Condition/Reason | Explanation | Recommendations |
|---|---|---|---|
| Neurological Conditions | Recent stroke, severe Parkinson’s disease, or uncontrolled seizures | Patients with these conditions may experience sudden balance changes or loss of coordination, increasing fall risk. | Avoid FRT; consider alternative balance assessments. |
| Musculoskeletal Conditions | Acute back pain, recent fractures, or severe arthritis | These conditions can cause pain and instability, increasing the risk of further injury. | Consult with the physician before administering; modify or avoid the test. |
| Cardiovascular Conditions | Uncontrolled hypertension or recent cardiac events | Sudden exertion during the FRT might pose a risk to cardiovascular stability. | Consult with the physician; monitor vital signs closely. |
| Cognitive Impairments | Severe cognitive deficits or confusion | Patients may have difficulty understanding instructions or maintaining balance. | Avoid FRT; consider alternative assessment methods. |
Adapting the FRT for Specific Disabilities
The FRT can be adapted for individuals with specific disabilities or conditions to ensure a safe and accurate assessment. For example, individuals with visual impairments may require verbal guidance and close supervision. Individuals with limited mobility may require assistance with positioning or support. Modifications should be made to accommodate the patient’s specific needs, always prioritizing safety. Using assistive devices, like a walker or cane, can be necessary for certain individuals to maintain stability during the test.
Clear communication and understanding of the patient’s limitations are essential for adapting the FRT.
Visual Representation of the Test: The Functional Reach Test In Physical Therapy
The Functional Reach Test (FRT) is a simple yet insightful assessment tool for evaluating a patient’s forward reach ability. Visualizing the test procedure and the patient’s posture is crucial for accurate administration and interpretation. This section provides a detailed, step-by-step guide to the FRT, highlighting key positions and observations.
Patient Setup and Positioning
Proper patient positioning is paramount for a reliable FRT. The patient stands with their feet shoulder-width apart, maintaining a comfortable and stable stance. Their arms are relaxed at their sides, and their gaze is directed forward. The patient should be positioned in a way that allows for a full, unimpeded forward reach. This is crucial for accurate measurement.
A stable surface, like a solid floor or a sturdy examination table, is needed to ensure the patient maintains balance.
Step-by-Step Demonstration of the FRT
The following steps detail the procedure for performing the FRT:
- The examiner stands facing the patient, approximately 12 inches away from the patient’s mid-line.
- The patient is instructed to stand with their feet shoulder-width apart and to maintain a relaxed posture, arms hanging loosely at their sides.
- The examiner marks a starting point on the wall, usually at the level of the patient’s mid-chest.
- The patient is instructed to extend their arm forward, maintaining a relaxed grip, as far as they comfortably can without losing their balance.
- The examiner marks the furthest point of the patient’s reach on the wall.
- The distance between the starting point and the farthest reach point is measured using a measuring tape or a ruler.
Visual Representation of Measurement
Imagine a patient standing, feet shoulder-width apart, facing a wall. A vertical line represents the patient’s midline, and a horizontal line marks the starting point at their mid-chest level. The patient extends their arm forward, touching the wall at their furthest reach. The distance between the starting point on the wall and the marked point of the patient’s reach is the functional reach measurement.
A ruler or measuring tape is used to quantify this distance.
Visual Cues to Observe During the Test
Several visual cues are essential during the FRT:
- Patient’s posture: Observe the patient’s stance and balance throughout the test. Maintaining a stable posture is crucial for accurate results.
- Arm extension: Note the range of motion of the patient’s arm during the reach. The arm should extend smoothly and without any apparent limitations. Any pain or stiffness should be noted.
- Balance: Watch for any signs of instability or swaying during the reach. This could indicate a need for additional support or modifications to the test procedure.
- Grip: Observe the patient’s grip. It should be relaxed and natural, allowing for the full range of motion.
Final Review
In conclusion, the functional reach test provides a valuable assessment tool for physical therapists. Understanding its intricacies, from administration to interpretation, empowers clinicians to tailor interventions and support patients’ functional mobility. While the test has limitations, its reliability and clinical utility make it a significant component in the overall assessment of balance and fall risk. Further research into specific applications and populations will continue to refine its use in the field of physical therapy.