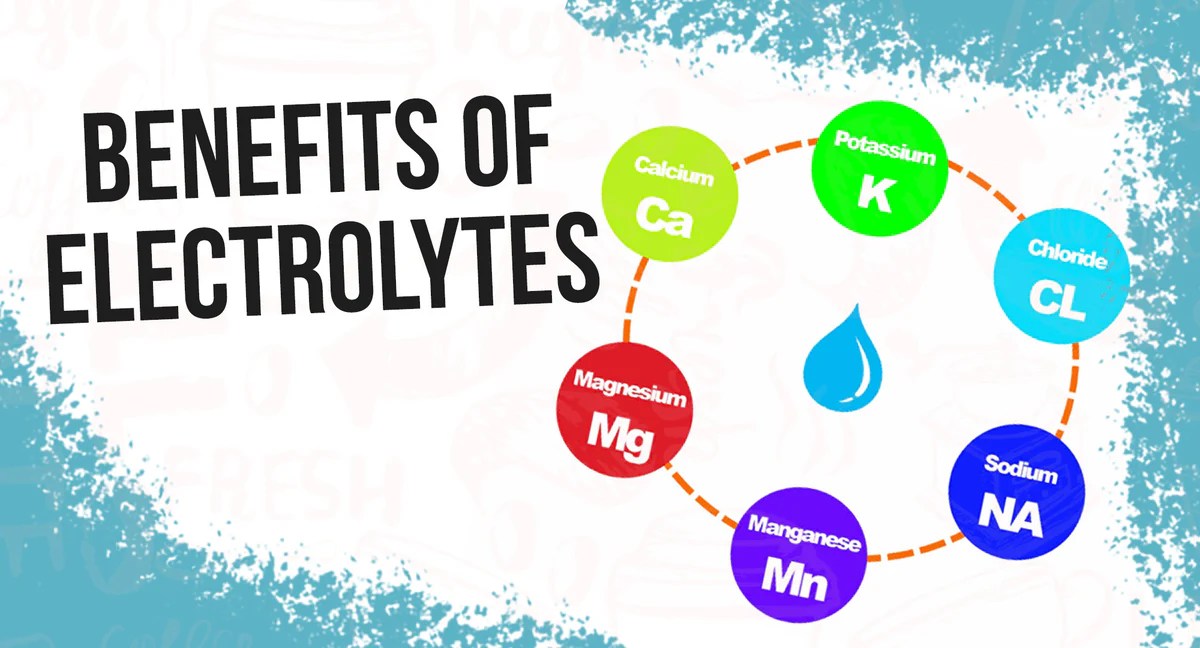
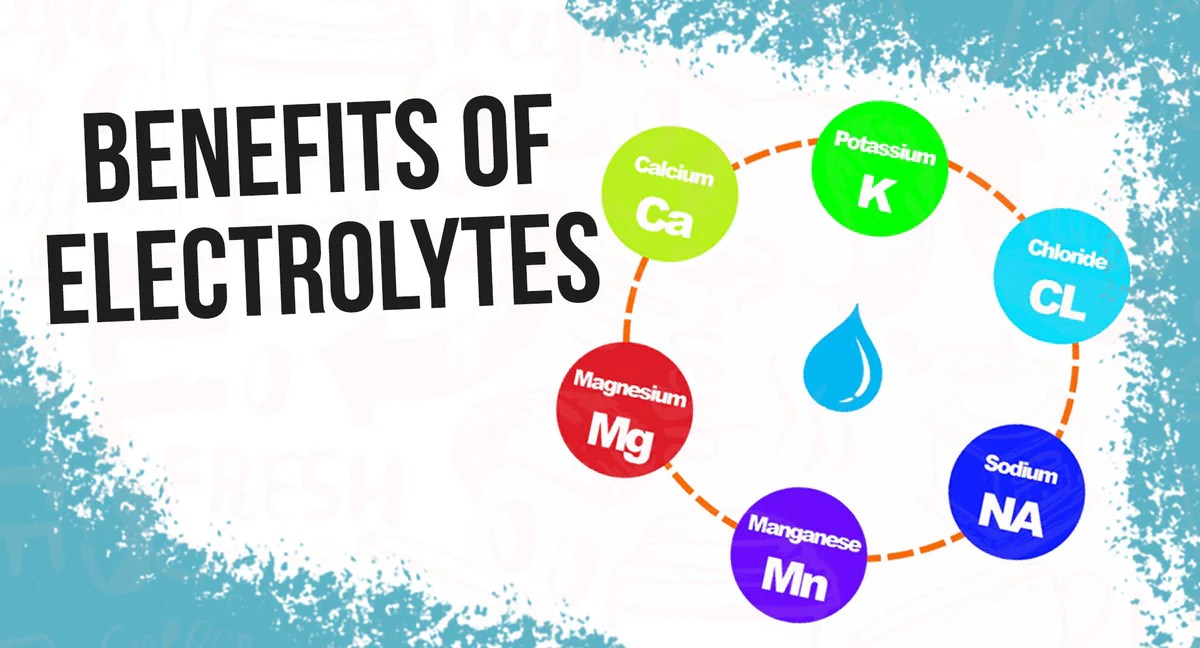
What happens when your body is low on electrolytes sets the stage for a fascinating exploration into the vital role these minerals play in our well-being. Electrolytes, essential minerals like sodium, potassium, calcium, and magnesium, are crucial for a multitude of bodily functions. From nerve impulses to muscle contractions, and from hydration to blood pressure regulation, their presence is indispensable.
When these crucial levels dip, a cascade of issues can arise, affecting everything from your energy levels to your overall health. This deep dive will explore the symptoms, causes, impacts, and management of electrolyte imbalances, equipping you with the knowledge to understand and maintain optimal electrolyte balance.
Electrolyte imbalances are more common than you might think. Diet, exercise, and even underlying health conditions can disrupt the delicate equilibrium of electrolytes in your body. Understanding the specific functions of each electrolyte and how their deficiency or excess can manifest is crucial. This article will explore the causes, symptoms, and potential impacts on various body systems, providing a comprehensive overview for better understanding.
Introduction to Electrolyte Imbalance
Electrolytes are minerals that carry an electric charge and are essential for numerous bodily functions. They are crucial for maintaining fluid balance, nerve and muscle function, and regulating various metabolic processes. Understanding electrolyte imbalances is critical for recognizing and addressing potential health concerns.The body meticulously regulates electrolyte levels through a complex interplay of mechanisms, including hormonal control, kidney function, and dietary intake.
These mechanisms work together to ensure that electrolyte concentrations remain within a narrow, healthy range. However, disruptions in these processes can lead to imbalances, impacting various physiological systems. These imbalances can manifest as a variety of symptoms, from mild discomfort to severe complications.
Definition and Role of Electrolytes
Electrolytes are minerals in the body that carry an electric charge. They are crucial for maintaining fluid balance, nerve and muscle function, and regulating various metabolic processes. Examples include sodium, potassium, calcium, magnesium, chloride, phosphate, and bicarbonate. These ions play vital roles in transmitting nerve impulses, contracting muscles, maintaining fluid balance, and regulating acid-base balance. Their precise balance is essential for optimal bodily functions.
Mechanisms of Electrolyte Regulation, What happens when your body is low on electrolytes
The body maintains electrolyte balance through a complex interplay of mechanisms, including hormonal control, kidney function, and dietary intake. The kidneys play a pivotal role in filtering blood and excreting excess electrolytes. Hormones, such as aldosterone, regulate the absorption and excretion of sodium and potassium. Dietary intake provides the necessary electrolytes for maintaining optimal levels. The intricate interplay of these factors ensures that electrolyte concentrations remain within a healthy range.
Common Causes of Electrolyte Imbalances
Electrolyte imbalances can stem from various factors, including dietary deficiencies, excessive sweating, vomiting, diarrhea, kidney disease, hormonal disorders, and certain medications. Dehydration, a common cause, can lead to electrolyte loss through excessive fluid loss. Severe vomiting or diarrhea rapidly depletes electrolytes, while kidney problems can interfere with the body’s ability to regulate electrolyte levels. Certain medications, such as diuretics, can also contribute to electrolyte imbalances.
Understanding the potential causes allows for more effective preventive and therapeutic strategies.
Electrolyte Imbalance Table
| Electrolyte | Function | Symptoms of Deficiency | Symptoms of Excess |
|---|---|---|---|
| Sodium (Na+) | Fluid balance, nerve function, muscle contraction | Headache, muscle cramps, nausea, vomiting, weakness | Fluid retention, high blood pressure, confusion, seizures |
| Potassium (K+) | Muscle function, nerve function, fluid balance | Muscle weakness, fatigue, irregular heartbeat, numbness | Muscle weakness, paralysis, irregular heartbeat, nausea |
| Calcium (Ca2+) | Bone health, nerve function, muscle contraction | Muscle cramps, bone pain, fatigue, numbness | Nausea, vomiting, constipation, kidney stones |
| Magnesium (Mg2+) | Muscle and nerve function, blood sugar control | Muscle cramps, weakness, fatigue, irregular heartbeat | Nausea, vomiting, diarrhea, weakness |
Symptoms and Signs of Electrolyte Imbalance
Electrolyte imbalances, a common occurrence, can significantly impact various bodily functions. These imbalances arise when the delicate balance of electrolytes like sodium, potassium, calcium, and magnesium in our blood is disrupted. This disruption can stem from various factors, including dietary deficiencies, excessive sweating, kidney problems, and certain medications. Understanding the symptoms associated with each electrolyte imbalance is crucial for early detection and appropriate treatment.
Sodium Imbalance
Sodium plays a critical role in maintaining fluid balance and nerve function. Low sodium levels, or hyponatremia, can lead to symptoms such as headache, nausea, vomiting, confusion, and even seizures. In contrast, high sodium levels, or hypernatremia, often result in excessive thirst, dry mouth, and, in severe cases, lethargy and altered mental status. Individual experiences with sodium imbalances can vary based on the severity and rate of change in sodium levels.
For instance, a gradual decline in sodium might cause less severe symptoms compared to a rapid decrease.
Potassium Imbalance
Potassium is vital for muscle function, nerve transmission, and heart rhythm regulation. Hypokalemia, or low potassium, may present with muscle weakness, cramps, fatigue, and in severe cases, irregular heartbeat. Hyperkalemia, high potassium, can manifest with symptoms such as muscle weakness, tingling, numbness, and potentially life-threatening cardiac arrhythmias. The rate and degree of potassium fluctuation influence symptom presentation.
For example, a slow, gradual increase in potassium levels may cause less acute symptoms than a rapid increase.
Feeling sluggish and a bit off? Low electrolytes can wreak havoc on your body, impacting everything from energy levels to skin health. Sometimes, this imbalance can manifest as hyperpigmentation on your buttocks – a darkening of the skin. Fortunately, there are ways to address this. Learning more about hyperpigmentation on buttocks what it is and how to get rid of it can help you understand the underlying causes and find effective solutions.
Understanding these issues can help you to restore balance in your body and feel better overall, because when your body has the right electrolytes, it can function optimally.
Calcium Imbalance
Calcium is essential for bone health, muscle function, and nerve transmission. Hypocalcemia, low calcium, often results in muscle cramps, spasms, tingling sensations, and, in severe cases, seizures. Hypercalcemia, high calcium, frequently leads to symptoms like nausea, vomiting, constipation, and kidney stones. The rate of calcium change influences the symptom severity; gradual changes might not be as noticeable as sudden fluctuations.
Magnesium Imbalance
Magnesium is crucial for numerous bodily functions, including muscle and nerve function, blood sugar control, and blood pressure regulation. Hypomagnesemia, low magnesium, can cause symptoms such as muscle weakness, tremors, seizures, and abnormal heart rhythms. Hypermagnesemia, high magnesium, may lead to nausea, vomiting, lethargy, and slowed heart rate. Individual reactions to magnesium imbalances can vary, with some individuals experiencing more pronounced symptoms than others.
Comparison of Electrolyte Imbalances
| Electrolyte | Symptoms (Deficiency) | Symptoms (Excess) | Impact on Body Systems |
|---|---|---|---|
| Sodium | Headache, nausea, vomiting, confusion, seizures | Excessive thirst, dry mouth, lethargy, altered mental status | Fluid balance, nerve function |
| Potassium | Muscle weakness, cramps, fatigue, irregular heartbeat | Muscle weakness, tingling, numbness, cardiac arrhythmias | Muscle function, nerve transmission, heart rhythm |
| Calcium | Muscle cramps, spasms, tingling, seizures | Nausea, vomiting, constipation, kidney stones | Bone health, muscle function, nerve transmission |
| Magnesium | Muscle weakness, tremors, seizures, abnormal heart rhythms | Nausea, vomiting, lethargy, slowed heart rate | Muscle and nerve function, blood sugar control, blood pressure |
Impact of Low Electrolytes on Body Systems

Low electrolyte levels, a common issue, can disrupt various bodily functions. These minerals, crucial for numerous processes, act like tiny messengers, facilitating everything from muscle contractions to nerve signals. When their levels dip below optimal ranges, a cascade of effects can ripple through the body, affecting how organs and systems work. Understanding these impacts is key to recognizing the importance of maintaining electrolyte balance.Electrolyte imbalances, particularly those involving sodium, potassium, calcium, and magnesium, can have far-reaching consequences.
Symptoms can vary greatly depending on the specific electrolyte deficiency and the individual’s overall health. Knowing how these imbalances affect different body systems can help diagnose and address the underlying problem effectively.
Effects on the Nervous System
The nervous system relies heavily on electrolytes to transmit signals throughout the body. Sodium and potassium are particularly important in maintaining nerve impulses. Low levels of these electrolytes can lead to a variety of neurological symptoms, ranging from mild fatigue and confusion to more severe issues like seizures and muscle spasms. Symptoms like tingling sensations, numbness, and even temporary paralysis can occur.
In extreme cases, severe electrolyte imbalances can lead to coma and death.
Impact on the Cardiovascular System
Electrolytes play a vital role in regulating heart function. Potassium, in particular, is essential for maintaining a regular heartbeat. Low potassium levels can lead to irregular heart rhythms, known as arrhythmias. These abnormalities can range from mild palpitations to potentially life-threatening conditions like ventricular fibrillation. Sodium imbalances can also affect blood pressure and volume, potentially impacting cardiovascular health.
An imbalance can lead to either elevated or dangerously low blood pressure, further stressing the cardiovascular system. Monitoring electrolyte levels is crucial for preventing complications in individuals with pre-existing cardiovascular conditions.
Effects on Muscle Function
Electrolytes are essential for muscle contraction. Potassium, calcium, and magnesium are all vital for this process. Deficiencies in these electrolytes can result in muscle weakness, cramps, and spasms. This is particularly noticeable in the extremities, with symptoms like leg cramps being a common complaint. Low magnesium levels can lead to increased muscle irritability and heightened sensitivity to stimuli, potentially triggering muscle spasms and cramps.
Dehydration, a common cause of electrolyte imbalance, often exacerbates muscle weakness and cramps.
Effects on the Digestive System
Electrolytes are also important for proper digestive function. Imbalances can lead to issues with digestion and absorption of nutrients. This can result in symptoms such as nausea, vomiting, and diarrhea. The intricate interplay of electrolytes in the digestive tract affects motility, acid secretion, and nutrient absorption. Low electrolyte levels can disrupt this delicate balance, causing digestive distress.
Table: Impact of Low Electrolytes on Body Systems
| Electrolyte | Affected Body System | Impact on System Function | Potential Complications |
|---|---|---|---|
| Potassium | Cardiovascular | Irregular heart rhythms (arrhythmias) | Heart attack, sudden cardiac death |
| Sodium | Nervous | Confusion, seizures, muscle weakness | Neurological damage |
| Calcium | Musculoskeletal | Muscle cramps, spasms, weakness | Fractures, difficulty breathing |
| Magnesium | Nervous and Muscular | Muscle spasms, tremors, seizures, confusion | Seizures, coma |
Diagnosing Low Electrolyte Levels
Identifying electrolyte imbalances is crucial for prompt and effective treatment. Accurate diagnosis hinges on a combination of clinical evaluation, including medical history, physical examination, and laboratory tests. These assessments provide valuable insights into the underlying causes and severity of the imbalance, guiding appropriate therapeutic interventions.
Diagnostic Procedures for Electrolyte Imbalance
Medical professionals employ a systematic approach to diagnose electrolyte imbalances. This involves a thorough review of the patient’s medical history, a comprehensive physical examination, and specific laboratory tests focusing on electrolyte levels in the blood. The combination of these methods provides a more complete picture of the patient’s condition and guides appropriate treatment strategies.
Blood Tests for Electrolyte Analysis
Blood tests are essential for evaluating electrolyte levels. Various types of blood tests are utilized to assess specific electrolytes, such as sodium, potassium, calcium, and magnesium. These tests measure the concentration of these minerals in the blood serum. Accurate interpretation of these results, alongside clinical context, is crucial for effective diagnosis and treatment planning.
Role of Medical History and Physical Examination
A detailed medical history plays a significant role in identifying potential causes of electrolyte imbalances. Factors such as recent illnesses, medications, dietary habits, and underlying medical conditions can all contribute to an electrolyte imbalance. The physical examination provides valuable clues, including signs such as muscle weakness, tremors, or changes in mental status, which may suggest an electrolyte imbalance.
By combining the information gathered from medical history and physical examination, healthcare providers can develop a more comprehensive understanding of the patient’s condition.
Diagnostic Table
| Diagnostic Method | Procedure | Expected Results (Normal) | Expected Results (Low) |
|---|---|---|---|
| Serum Electrolyte Panel | Measures concentrations of sodium, potassium, chloride, calcium, magnesium, and phosphate in a blood sample. | Sodium: 135-145 mEq/L Potassium: 3.5-5.0 mEq/L Chloride: 98-107 mEq/L Calcium: 8.6-10.2 mg/dL Magnesium: 1.3-2.1 mg/dL Phosphate: 2.5-4.5 mg/dL |
Sodium: Below 135 mEq/L Potassium: Below 3.5 mEq/L Chloride: Below 98 mEq/L Calcium: Below 8.6 mg/dL Magnesium: Below 1.3 mg/dL Phosphate: Below 2.5 mg/dL |
| Urine Electrolyte Analysis | Evaluates electrolyte levels in a urine sample. | Varied depending on hydration and diet, but typically reflects overall electrolyte balance. | Concentrated urine with low electrolyte levels could suggest dehydration or certain kidney conditions. |
| Urinalysis | Analysis of physical and chemical properties of urine, including specific gravity, pH, protein, and glucose levels. | Normal specific gravity, pH, and absence of protein or glucose. | Abnormal specific gravity, pH, protein or glucose could suggest underlying conditions impacting electrolyte balance. |
Treatments and Management of Electrolyte Imbalance
Electrolyte imbalances, while often subtle, can significantly impact your overall health and well-being. Proper treatment and management are crucial for restoring balance and preventing potentially serious complications. Effective strategies focus on replenishing lost electrolytes, addressing underlying causes, and maintaining a healthy lifestyle.Electrolyte imbalances are typically treated by addressing the underlying cause, such as a medical condition or medication side effect, and replenishing the lost electrolytes.
This can involve oral or intravenous rehydration, dietary adjustments, and sometimes medications. The specific treatment plan is tailored to the individual’s needs and the severity of the imbalance.
Oral or Intravenous Rehydration
Oral rehydration is a common initial approach for mild electrolyte imbalances. It involves drinking fluids containing electrolytes, such as sports drinks or electrolyte solutions. Intravenous (IV) rehydration is often necessary for severe imbalances or when oral intake is not possible. IV fluids deliver electrolytes directly into the bloodstream, quickly restoring balance. The choice between oral and IV rehydration depends on the severity of the imbalance and the patient’s ability to tolerate oral fluids.
For example, individuals with vomiting or diarrhea may benefit more from IV rehydration to quickly replenish lost fluids and electrolytes.
Medications for Electrolyte Imbalance Correction
Various medications can be used to correct specific electrolyte deficiencies or excesses. These medications, prescribed by a healthcare professional, work by either replacing the missing electrolyte or blocking its absorption or excretion. For example, potassium supplements are commonly used to treat low potassium levels (hypokalemia), while diuretics can be used to manage high sodium levels (hypernatremia) in specific cases.
Low electrolytes can wreak havoc on your body, causing everything from muscle cramps to fatigue. While some people experience vivid dreams when their electrolyte levels are off, this doesn’t necessarily mean there’s a mental health issue. The connection between electrolyte imbalance and unusual dreams is worth exploring, but it’s important to remember that are vivid dreams a sign of mental illness ?
The answer is often complex and requires a deeper understanding of both. Ultimately, if you’re concerned about your sleep patterns or general health, consulting a doctor is always the best course of action, particularly if you’re experiencing other symptoms related to electrolyte imbalances.
The appropriate medication and dosage are carefully determined based on the individual’s specific needs and underlying conditions.
Balanced Diet for Electrolyte Maintenance
A balanced diet plays a vital role in maintaining optimal electrolyte levels. A diet rich in fruits, vegetables, and whole grains provides essential electrolytes like potassium, sodium, calcium, and magnesium. For example, bananas are a good source of potassium, while leafy greens provide magnesium. Avoiding processed foods, sugary drinks, and excessive salt intake is also crucial in preventing electrolyte imbalances.
A balanced diet, coupled with regular exercise and hydration, supports overall health and electrolyte homeostasis.
Lifestyle Modifications for Prevention
Certain lifestyle modifications can significantly contribute to preventing electrolyte imbalances. Regular exercise, coupled with proper hydration, helps maintain electrolyte balance. Adequate sleep is equally important, as sleep deprivation can disrupt the body’s electrolyte regulation. For instance, athletes who engage in intense physical activity should pay particular attention to their hydration and electrolyte intake during and after exercise to prevent imbalances.
Stress management techniques can also play a role in maintaining overall electrolyte balance.
Table of Electrolyte Treatments
| Electrolyte | Treatment Method | Dosage/Frequency | Potential Side Effects |
|---|---|---|---|
| Potassium | Potassium supplements | Based on individual needs, typically 20-100 mEq daily, divided doses. | Nausea, vomiting, diarrhea, abdominal cramps, and irregular heartbeat (arrhythmias) in high doses. |
| Sodium | Oral electrolyte solutions or IV fluids | Depending on the severity and individual needs, guided by healthcare professionals. | Fluid overload, high blood pressure, and edema in cases of excessive intake. |
| Calcium | Calcium supplements | Based on individual needs, typically 500-1500 mg daily, divided doses. | Nausea, constipation, abdominal cramps, kidney stones, and interaction with other medications. |
| Magnesium | Magnesium supplements | Based on individual needs, typically 300-400 mg daily, divided doses. | Diarrhea, nausea, and abdominal cramps. Large doses may interact with other medications. |
Preventing Electrolyte Imbalances: What Happens When Your Body Is Low On Electrolytes
Maintaining optimal electrolyte levels is crucial for overall health and well-being. Electrolyte imbalances can arise from various factors, including diet, hydration, and activity levels. Proactive measures can significantly reduce the risk of these imbalances, ensuring your body functions smoothly and efficiently.Understanding the dietary components that contribute to electrolyte balance empowers you to make informed choices for a healthier you.
This includes recognizing the specific foods rich in various electrolytes and adjusting your intake accordingly. Hydration plays a pivotal role, as does regular exercise, both of which contribute to maintaining electrolyte homeostasis.
Dietary Recommendations for Optimal Electrolyte Levels
A balanced diet is key to preventing electrolyte imbalances. Focusing on a variety of foods rich in different electrolytes ensures your body receives the necessary nutrients. Prioritizing whole, unprocessed foods over highly processed options is a smart strategy.
Foods Rich in Different Electrolytes
Various foods naturally contain electrolytes. Understanding which foods are rich in specific electrolytes allows you to incorporate them into your daily meals. Here’s a look at some excellent sources:
- Potassium: Fruits like bananas, avocados, and apricots; vegetables like spinach, sweet potatoes, and broccoli; and dairy products like yogurt are excellent sources. Potassium is vital for muscle function and nerve signals.
- Sodium: Table salt (sodium chloride) is the most common source. However, it’s crucial to consume it in moderation. Processed foods, canned goods, and fast food often contain high amounts of sodium. Natural sources include seaweed, olives, and some cheeses.
- Calcium: Dairy products (milk, yogurt, cheese) are excellent sources of calcium, vital for bone health and muscle function. Leafy green vegetables, such as kale and collard greens, also contain calcium, though in smaller amounts. Fortified plant-based milks are another option.
- Magnesium: Leafy green vegetables (spinach, kale), nuts (almonds, cashews), seeds (pumpkin, sunflower), and whole grains are good sources of magnesium. Magnesium is essential for muscle and nerve function.
- Phosphorus: Meat, poultry, fish, eggs, dairy products, and legumes are rich in phosphorus. Phosphorus is crucial for bone health and energy production.
Importance of Hydration and Fluid Balance
Adequate hydration is essential for electrolyte balance. The body loses electrolytes through sweat, urine, and other bodily fluids. Replacing these lost electrolytes through proper hydration is key. Dehydration can lead to electrolyte imbalances.
Role of Regular Exercise in Electrolyte Homeostasis
Regular exercise, particularly endurance activities, can lead to electrolyte loss through sweat. Replenishing electrolytes lost through sweat is essential for preventing imbalances. The amount of electrolyte loss depends on factors like intensity and duration of exercise.
Feeling sluggish and drained? Low electrolytes can wreak havoc on your body, leading to everything from muscle cramps to headaches. Understanding the causes and potential risks is crucial, and sometimes surprising connections can be made. For example, certain risk factors for macular degeneration, like a poor diet and lack of hydration, can also play a role in electrolyte imbalances.
Macular degeneration causes risk factors can be directly impacted by electrolyte levels. So, while maintaining a healthy balance of electrolytes is important for overall well-being, it’s a reminder to take care of our bodies in a holistic manner.
Detailed List of Foods to Include and Exclude for Each Electrolyte
This table provides a more detailed overview of foods to include and exclude for each electrolyte, ensuring balanced intake:
| Electrolyte | Foods to Include | Foods to Exclude (or consume in moderation) |
|---|---|---|
| Potassium | Bananas, avocados, spinach, sweet potatoes, yogurt | Highly processed foods, many canned goods |
| Sodium | Seaweed, olives, some cheeses | Processed foods high in salt, many fast-food items |
| Calcium | Milk, yogurt, cheese, kale, collard greens | Highly processed foods, soft drinks |
| Magnesium | Leafy greens, nuts, seeds, whole grains | Highly processed foods, refined grains |
| Phosphorus | Meat, poultry, fish, eggs, dairy | Highly processed foods |
Illustrative Case Studies
Electrolyte imbalances, while often subtle, can have significant consequences on overall health. Understanding how these imbalances manifest, are diagnosed, and treated is crucial for prompt intervention and positive patient outcomes. This section presents real-life case studies to illustrate the importance of early detection and effective management strategies.Case studies provide valuable insights into the complexities of electrolyte disorders, demonstrating the diverse presentations, diagnostic challenges, and therapeutic approaches required for successful recovery.
Each example highlights the interplay between symptoms, diagnostic tests, and treatment plans.
A Case of Dehydration-Induced Hyponatremia
Dehydration, particularly in individuals participating in prolonged physical activity or those with underlying health conditions, can lead to hyponatremia, a condition characterized by low sodium levels in the blood. This can manifest in a variety of symptoms, including headache, nausea, confusion, and even seizures.A 25-year-old marathon runner experienced severe headache and confusion during the final 10 kilometers of a marathon.
Symptoms escalated rapidly. The runner reported consuming large quantities of water during the race. Initial assessment revealed low sodium levels. Diagnosis was confirmed by blood tests that showed a markedly low serum sodium concentration. Treatment involved intravenous saline solution to gradually restore sodium levels.
The runner was monitored closely for any signs of neurological complications. The patient recovered fully after 2 days of intensive hydration and electrolyte replacement.
Importance of Early Detection in Hypokalemia
Hypokalemia, or low potassium levels, can have subtle onset, potentially leading to delayed diagnosis. Early detection and prompt treatment are vital to prevent serious complications.A 60-year-old woman with a history of heart failure presented with fatigue and muscle weakness. These symptoms were initially attributed to her underlying condition. However, blood tests revealed dangerously low potassium levels. Early intervention with potassium supplements and careful monitoring prevented potentially fatal cardiac arrhythmias.
This case illustrates how careful attention to symptoms, even in individuals with existing medical conditions, can be crucial for early diagnosis and appropriate treatment of electrolyte imbalances.
The Diagnostic and Treatment Process for Hypercalcemia
Hypercalcemia, characterized by elevated calcium levels, can arise from various causes, including certain cancers or hyperparathyroidism. Diagnosing the underlying cause is essential for effective treatment.A 65-year-old man experienced bone pain and fatigue. Blood tests revealed abnormally high calcium levels. Further investigations, including imaging studies and parathyroid hormone levels, determined the cause as parathyroid adenoma. Treatment involved a combination of medications to lower calcium levels and address the underlying cause.
The patient experienced symptom resolution and gradual normalization of calcium levels over several weeks under close monitoring.
Final Summary
In conclusion, maintaining proper electrolyte balance is vital for overall health and well-being. Understanding the symptoms, causes, and potential impacts of electrolyte imbalances empowers individuals to take proactive steps towards maintaining optimal levels. A balanced diet, adequate hydration, and mindful lifestyle choices can contribute significantly to preventing these imbalances. By arming yourself with the knowledge presented in this article, you’re better prepared to recognize the signs and seek appropriate medical attention when necessary.