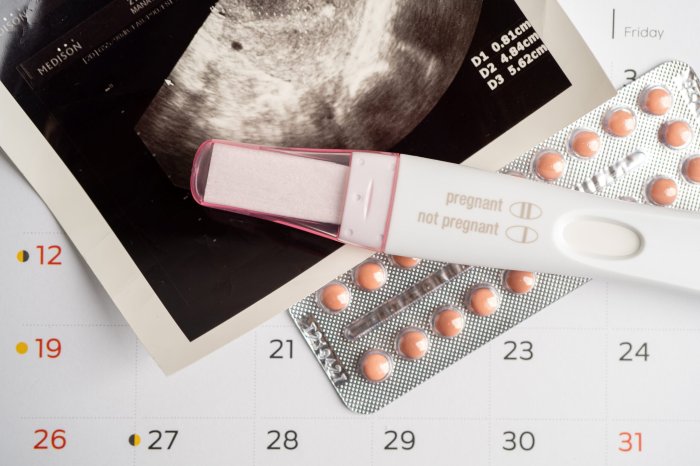
When to take a pregnancy test if you have PCOS sets the stage for understanding the unique challenges and opportunities in trying to conceive. Navigating irregular cycles and symptoms can make timing a pregnancy test crucial. This guide dives deep into understanding PCOS, its impact on ovulation, and how to effectively predict and interpret those critical signs.
This exploration delves into the complexities of PCOS and fertility, explaining how irregular periods, ovulation patterns, and early pregnancy symptoms can intertwine. We’ll also explore practical methods for tracking ovulation, deciphering symptoms, and understanding when to seek professional guidance for a clearer picture of your reproductive health.
Understanding PCOS and Fertility
Polycystic ovary syndrome (PCOS) is a hormonal disorder that affects women of reproductive age. It’s characterized by an imbalance in reproductive hormones, which can disrupt the normal functioning of the ovaries and menstrual cycle. This hormonal disruption significantly impacts ovulation, the process of releasing an egg from the ovary, making it harder to conceive. Understanding the connection between PCOS and fertility is crucial for women seeking to conceive.PCOS is a complex condition that often manifests with irregular menstrual cycles, and this irregularity can make it challenging to predict when ovulation occurs.
Figuring out when to take a pregnancy test if you have PCOS can be tricky, as irregular cycles can make it harder to pinpoint ovulation. While symptoms like spotting or changes in your period are common, it’s important to consider other factors. For example, understanding the causes and symptoms of a cherry angioma, a common skin condition, might not seem directly related, but learning more about these types of benign vascular tumors from cherry angioma symptoms causes diagnosis treatment can broaden your perspective on how to interpret your body’s signals.
Ultimately, consulting with your doctor is key to determining the best time to test, especially if you’re experiencing any unusual symptoms. This is still crucial for accurately pinpointing pregnancy when dealing with PCOS.
The hormonal fluctuations associated with PCOS can lead to a variety of symptoms that can impact a woman’s overall well-being, which may also influence when a pregnancy test is taken.
Impact on Ovulation
PCOS frequently results in infrequent or absent ovulation. This means that the ovaries may not release an egg regularly, or not at all. Without ovulation, fertilization cannot occur, which directly affects the chances of getting pregnant. A lack of regular ovulation can manifest as unpredictable and irregular menstrual cycles. The timing of ovulation is crucial for successful conception, and the unpredictability associated with PCOS makes it more difficult to determine the optimal time to try for pregnancy.
Menstrual Cycle Irregularities
Women with PCOS often experience irregular menstrual cycles. These irregularities can vary from infrequent periods to prolonged or absent menstruation. This irregularity in the menstrual cycle makes it harder to predict ovulation and thus, the ideal time to conceive. Some women with PCOS may experience periods that are very light, or very heavy, with prolonged bleeding. In some cases, the cycle might last for several weeks or months between periods.
Affecting Likelihood of Conception
The irregular ovulation patterns characteristic of PCOS significantly decrease the chances of getting pregnant. Without regular ovulation, there’s no egg available for fertilization. This reduced likelihood of conception is often a concern for women diagnosed with PCOS who are trying to conceive. Many women with PCOS conceive naturally, but often take longer to get pregnant than women without the condition.
They may need to explore different fertility treatments or strategies to improve their chances of pregnancy.
Figuring out when to take a pregnancy test if you have PCOS can be tricky. Many women with PCOS experience irregular cycles, making it hard to pinpoint ovulation. Sometimes, a tingling sensation in your head scalp might pop up, and if you’re wondering about the cause, check out this helpful article on tingling sensation in head scalp.
But, if you’re hoping to catch a possible pregnancy, testing around the time you’d expect your period, even if it’s irregular, is often a good starting point. This will give you the most accurate results.
Common Symptoms and Their Potential Impact on Ovulation
| Symptom | Description | Potential Impact on Ovulation |
|---|---|---|
| Irregular or absent periods | Menstrual cycles that are unpredictable in length and frequency. May be very light or very heavy, or may be absent for several weeks or months. | Directly affects ovulation predictability, making it difficult to determine the optimal time for conception. |
| Weight gain or difficulty losing weight | Increased body weight, particularly around the midsection. Can be challenging to manage due to hormonal imbalances. | Weight gain is often linked to insulin resistance, which can further disrupt ovulation patterns. |
| Acne | Skin breakouts, especially on the face, chest, and back. | Hormonal imbalances can contribute to increased oil production and acne. |
| Hirsutism (excess hair growth) | Unwanted hair growth on the face, chest, back, or abdomen. | Androgen imbalances often cause increased hair growth, which is linked to ovulation irregularity. |
| Hair loss | Thinning hair or baldness. | Androgen imbalances can cause hair loss, which is often associated with ovulation problems. |
Factors Affecting Test Timing
Knowing when to take a pregnancy test is crucial for accurate results, especially for women with PCOS. Irregular cycles, a hallmark of PCOS, can significantly affect the timing of ovulation and the optimal window for detecting pregnancy. Understanding these factors can help you interpret results more effectively and avoid unnecessary stress or disappointment.Understanding your unique cycle, even with PCOS, can greatly enhance your chances of accurate pregnancy test results.
This involves recognizing the impact of your hormonal fluctuations on the timing of ovulation. By learning to predict ovulation, you can effectively time your pregnancy test for optimal accuracy.
Irregular Periods and Test Timing
Irregular periods are a common characteristic of PCOS. These cycles can vary significantly in length and predictability, making it challenging to pinpoint the ideal time to take a pregnancy test. Without a regular cycle, it becomes difficult to follow the typical “two-week wait” rule that works well for women with regular periods.
Understanding Your Menstrual Cycle
Understanding your menstrual cycle, even with PCOS, can provide valuable insight into when you’re most likely to ovulate. Paying attention to the length of your cycle, the timing of your period, and any accompanying symptoms can offer clues. While a regular cycle can be a helpful guideline, women with PCOS often have varying cycle lengths, making it important to track these factors consistently.
Regular tracking can help you identify patterns and predict your ovulation window.
Ovulation and the LH Surge
Ovulation, the release of an egg from the ovary, is triggered by a surge in luteinizing hormone (LH). This surge typically occurs 24 to 48 hours before ovulation. Monitoring LH levels, either through ovulation predictor kits or blood tests, can help you pinpoint the precise time of ovulation. The LH surge is a key indicator of impending ovulation, providing a timeframe for accurately anticipating the fertile window.
Comparing and Contrasting Cycles, When to take a pregnancy test if you have pcos
Typical menstrual cycles often follow a predictable pattern with a relatively consistent ovulation time. In contrast, women with PCOS often experience unpredictable cycles, characterized by prolonged anovulatory cycles (cycles without ovulation). This irregularity in ovulation makes precise timing more difficult. In a typical cycle, ovulation usually occurs around day 14 of a 28-day cycle. With PCOS, this timing can fluctuate significantly.
Ovulation Tracking Methods for PCOS
Several methods can help women with PCOS track ovulation, including:
- Basal Body Temperature (BBT) Tracking: Taking your temperature first thing in the morning before any activity provides insight into ovulation. A slight increase in temperature usually signifies ovulation. Consistent tracking can help identify patterns, even with irregular cycles. Recordings should be taken with precision and regularity.
- Ovulation Predictor Kits (OPKs): OPKs measure LH levels in urine. A surge in LH usually indicates ovulation is imminent. These kits can be particularly helpful in identifying the fertile window, but may not be as reliable for those with extremely irregular cycles.
- Cervical Mucus Monitoring: Changes in cervical mucus can also signal ovulation. Monitoring for changes in consistency and amount can be helpful in predicting ovulation. However, this method can be subjective and may not be as reliable for all women with PCOS.
By employing these methods, women with PCOS can gain a better understanding of their cycle and potentially increase their chances of conceiving. Remember, consistency is key when tracking your cycle.
Interpreting Symptoms and Timing
Navigating the potential overlap between PCOS symptoms and early pregnancy signs can be tricky. Understanding how to differentiate these symptoms and when to seek professional guidance is crucial for making informed decisions about your health and well-being. This section focuses on interpreting potential early pregnancy symptoms, highlighting the importance of medical consultation, and clarifying the typical timeframe for a positive pregnancy test result.Interpreting early pregnancy symptoms, particularly when you have PCOS, requires careful attention and a good understanding of your body’s unique signals.
It’s essential to distinguish between symptoms that might indicate pregnancy and those that are typical PCOS manifestations. This section will help you understand the subtle differences and when to seek medical advice.
Potential Early Pregnancy Symptoms Mimicking PCOS Symptoms
Early pregnancy symptoms can sometimes mimic existing PCOS symptoms, making accurate self-diagnosis challenging. This overlap can lead to confusion and delay in seeking appropriate medical care. Recognizing these similarities is key to timely and informed decision-making.
- Fatigue: Both PCOS and early pregnancy can cause fatigue. Pregnancy-related fatigue often increases gradually, while PCOS fatigue might fluctuate with hormonal changes. If fatigue is persistent and worsening, consult a healthcare professional.
- Mood Swings: Hormonal fluctuations are common in both conditions. Pregnancy-related mood changes can be more pronounced, while PCOS mood swings may correlate with fluctuating hormone levels. Monitoring any significant changes in mood and consulting with a doctor is recommended.
- Breast Tenderness: Breast tenderness can be a symptom of both conditions. In pregnancy, this tenderness is often more pronounced, while in PCOS, it might be related to hormonal imbalances. Seeking professional guidance for persistent breast tenderness is important.
- Increased Urination: Frequent urination is a common pregnancy symptom. In PCOS, this symptom might be related to other hormonal imbalances. Tracking your urination frequency and reporting it to your healthcare provider is crucial.
Importance of Consulting a Healthcare Professional
Seeking medical advice is vital for accurate diagnosis and management of any potential health concern. It is impossible to definitively determine if symptoms are related to pregnancy or PCOS without a professional evaluation.
“Medical professionals can provide tailored advice and support based on your specific situation and medical history.”
A healthcare professional can differentiate between PCOS symptoms and early pregnancy symptoms by taking a detailed medical history, conducting a physical examination, and potentially ordering relevant diagnostic tests. This personalized approach is crucial for ensuring appropriate treatment and management.
False Negative Results and Timing
A false negative pregnancy test result can occur if the test is taken too early. The hCG hormone, which is detected by pregnancy tests, rises rapidly after implantation. Taking a test before sufficient hCG has accumulated in the urine may yield a false negative result.
“The typical timeframe for a positive pregnancy test result after ovulation is approximately 10-14 days after conception.”
This timeframe is not a hard and fast rule, as individual circumstances can affect hormone levels and test sensitivity. Consulting a doctor can help clarify the optimal timing for testing based on your specific situation.
Typical Timeframe for a Positive Pregnancy Test
The typical timeframe for a positive pregnancy test result after ovulation is around 10-14 days post-conception. This is based on the average time it takes for the hCG hormone to reach detectable levels in the urine. However, this timeframe can vary depending on individual factors.
Potential Symptoms, Causes, and Medical Guidance
| Symptom | Possible Cause (PCOS or Pregnancy) | Advice on Seeking Medical Guidance |
|---|---|---|
| Fatigue | PCOS, Pregnancy | Consult a healthcare professional if fatigue is persistent and worsening. |
| Mood Swings | PCOS, Pregnancy | Monitor significant changes in mood and consult with a doctor. |
| Breast Tenderness | PCOS, Pregnancy | Seek professional guidance for persistent breast tenderness. |
| Increased Urination | PCOS, Pregnancy | Track urination frequency and report it to your healthcare provider. |
| Missed Period | PCOS, Pregnancy | A missed period can be a sign of pregnancy or PCOS-related irregularities. Consult a doctor for proper diagnosis and guidance. |
Medical Advice and Professional Guidance
Navigating the complexities of PCOS and fertility can feel overwhelming. Understanding your specific situation and making informed decisions requires expert guidance. This section focuses on the crucial role of medical professionals in managing PCOS and supporting your journey toward pregnancy.
Importance of Consulting a Doctor
Accurate diagnosis and personalized treatment plans are essential for effectively managing PCOS and optimizing fertility. A healthcare provider can assess your specific situation, conduct necessary tests, and tailor a management strategy that addresses your unique needs.
| Reason | Importance |
|---|---|
| Early Diagnosis | Early detection allows for timely intervention and management of potential complications, such as insulin resistance, metabolic syndrome, and cardiovascular issues. |
| Personalized Treatment | Individualized plans address the specific symptoms and health factors related to your PCOS. |
| Monitoring Progress | Regular check-ups enable the healthcare provider to track your response to treatment and make necessary adjustments. |
| Reduced Risk | Regular check-ups and preventative measures help reduce the risk of long-term health issues. |
Working with a Healthcare Provider
Managing PCOS and pregnancy requires a collaborative effort between you and your healthcare provider. They will be instrumental in monitoring your overall health, adjusting treatments as needed, and guiding you through the process.
- Regular check-ups are crucial to track your hormone levels, monitor blood sugar, and address any emerging concerns.
- Addressing nutritional needs and lifestyle modifications are key aspects of management, and your provider can guide you on appropriate dietary changes and exercise plans.
- Monitoring the effectiveness of treatment is essential. Adjustments to medication or lifestyle strategies may be necessary as your body responds.
Fertility Specialist Consultation
If you are trying to conceive, consulting a fertility specialist can be invaluable. They possess specialized knowledge and experience in addressing fertility challenges, particularly those related to PCOS.
- Fertility specialists can provide tailored strategies to improve egg quality and ovulation.
- They can suggest specific treatments, such as ovulation induction medications, to increase the chances of successful conception.
- Specialized knowledge allows them to effectively assess and address potential underlying factors that might hinder conception.
Role of Blood Tests
Blood tests play a critical role in confirming pregnancy and monitoring PCOS. They can measure hormone levels, assess overall health, and evaluate the effectiveness of treatments.
- Blood tests help identify and monitor hormone imbalances, such as elevated androgens or irregular progesterone levels, that can affect fertility.
- They are essential in monitoring blood sugar levels to ensure they are within a healthy range.
- Monitoring thyroid function through blood tests is important, as thyroid issues can exacerbate PCOS symptoms and affect fertility.
- Blood tests can also confirm pregnancy by detecting the presence of human chorionic gonadotropin (hCG).
Different Medical Professional Approaches
Different medical professionals may adopt varied approaches to discussing pregnancy with PCOS. Some may focus on general health management, while others may prioritize fertility support. It’s important to communicate your goals and preferences to ensure you receive the appropriate guidance and support.
- General practitioners (GPs) often provide initial assessments and basic management strategies.
- Endocrinologists, specializing in hormone disorders, can offer specialized insights into hormone regulation and treatment options.
- Obstetricians and gynecologists (OB-GYNs) often focus on reproductive health and pregnancy-related concerns.
- Fertility specialists provide specialized care for improving fertility and managing pregnancy complications in women with PCOS.
Common Misconceptions and Concerns

Navigating the world of PCOS and fertility can be challenging, often riddled with misconceptions and anxieties. Understanding these common myths can empower you to make informed decisions and focus on strategies that truly support your journey toward pregnancy. This section aims to debunk common myths, highlighting the specific hurdles women with PCOS face and emphasizing the importance of proactive management.Many women with PCOS experience a unique set of challenges when trying to conceive.
These challenges, coupled with societal pressures and sometimes conflicting medical advice, can lead to feelings of frustration and uncertainty. By understanding the nuances of PCOS and fertility, and recognizing the common misconceptions, you can equip yourself with the knowledge needed to navigate this process effectively and confidently.
Common Myths Surrounding Pregnancy Testing and PCOS
Common misconceptions about pregnancy testing and PCOS can significantly impact a woman’s approach to fertility. These misunderstandings can lead to unnecessary stress and delay in seeking appropriate medical guidance. Clearing up these myths allows for a more focused and effective strategy.
- A woman with PCOS cannot get pregnant naturally.
While PCOS can affect ovulation and make natural conception more challenging, it doesn’t mean pregnancy is impossible. Many women with PCOS conceive naturally, often with lifestyle adjustments and sometimes with the help of fertility treatments. A balanced diet, regular exercise, and stress management can significantly improve the chances of natural conception.
Wondering when to take a pregnancy test if you have PCOS? It’s tricky since PCOS can sometimes cause irregular cycles, making it hard to pinpoint ovulation. You might want to start testing around the time you’d expect your period, or consider using ovulation predictor kits. If you’re experiencing painful symptoms like frequent urination, though, it’s important to check for a bladder infection.
Fortunately, there are ways to self-treat a bladder infection, like drinking plenty of fluids and using over-the-counter remedies. how can i selftreat a bladder infection However, remember that this information is for general knowledge only and doesn’t replace professional medical advice. For accurate guidance on when to take a pregnancy test with PCOS, always consult a doctor.
- PCOS always leads to severe fertility problems.
The impact of PCOS on fertility varies significantly from woman to woman. While some women experience significant difficulty conceiving, others may only experience mild disruptions to their menstrual cycles. Individual responses to PCOS differ, and early intervention and management can significantly improve the chances of successful conception. For example, a woman with PCOS might experience irregular cycles but still ovulate occasionally, allowing for natural pregnancy.
- Taking a pregnancy test early will reveal accurate results.
Early pregnancy tests often have a low accuracy rate. It is important to follow the manufacturer’s instructions for accurate results. The accuracy of home pregnancy tests increases as the pregnancy progresses and the hormone levels in the body rise. For example, a test taken too early might show a negative result even if a pregnancy is developing.
Potential Challenges Faced by Women with PCOS
Women with PCOS often face several obstacles when trying to conceive. These challenges can stem from hormonal imbalances, insulin resistance, and lifestyle factors.
- Irregular or absent ovulation.
The irregular or absent ovulation associated with PCOS can make it difficult for the egg to be released, preventing fertilization. This can be a significant hurdle in achieving pregnancy naturally.
- Insulin resistance.
Insulin resistance, a common feature of PCOS, can further exacerbate the problems with ovulation. High insulin levels can disrupt the delicate hormonal balance needed for a regular menstrual cycle and ovulation. Managing insulin resistance is crucial for optimizing fertility outcomes.
Importance of Managing PCOS to Optimize Chances of a Healthy Pregnancy
Managing PCOS effectively is essential for optimizing chances of a healthy pregnancy. This involves addressing the underlying hormonal imbalances, insulin resistance, and lifestyle factors.
- Maintaining a healthy weight.
Maintaining a healthy weight can significantly improve insulin sensitivity and regulate ovulation cycles. This can improve chances of natural conception.
- Adopting a balanced diet and exercise routine.
A balanced diet rich in fruits, vegetables, and whole grains, combined with regular exercise, can help manage insulin resistance and promote overall well-being. Regular exercise can help regulate ovulation and improve metabolic health.
Long-Term Implications of PCOS on Fertility
The long-term implications of PCOS on fertility are significant. Women with PCOS may experience an increased risk of developing other health complications.
- Increased risk of gestational diabetes and preeclampsia.
Women with PCOS have an increased risk of gestational diabetes and preeclampsia during pregnancy. These conditions can lead to complications for both the mother and the baby.
| Common Misconception | Accurate Information |
|---|---|
| Women with PCOS cannot get pregnant. | PCOS can affect ovulation but doesn’t always prevent pregnancy. Lifestyle changes and medical intervention can be helpful. |
| Early pregnancy tests always reveal accurate results. | Home pregnancy tests are accurate after a certain time in pregnancy. Follow manufacturer instructions. |
| PCOS automatically leads to severe fertility issues. | The impact of PCOS on fertility varies greatly between women. Some may conceive naturally while others may require medical assistance. |
Resources and Support
Navigating PCOS and fertility concerns can feel isolating. However, you’re not alone. A wealth of resources and supportive communities exist to help you navigate this journey. Knowing where to turn for help can make a significant difference in your well-being and confidence as you explore options.Finding the right information and support is crucial. This section Artikels reliable online resources, the value of support groups, and how to connect with healthcare professionals who specialize in PCOS and fertility.
Reliable Online Resources
A plethora of online resources offer valuable information about PCOS and fertility. These resources can provide comprehensive details about the condition, treatment options, and support groups. They can also help you understand the emotional and physical challenges you may face.
- National Institutes of Health (NIH): The NIH provides a wealth of information on PCOS and reproductive health, including research findings and educational materials. They are a trusted source for reliable data.
- Mayo Clinic: This renowned medical institution offers comprehensive articles and resources on various medical conditions, including PCOS and its impact on fertility.
- American Society for Reproductive Medicine (ASRM): The ASRM is a professional organization dedicated to reproductive health. Their website provides evidence-based information on fertility treatments and reproductive technologies.
- Organizations dedicated to PCOS awareness: Many non-profit organizations focus specifically on PCOS. These organizations often provide detailed information, support groups, and advocacy efforts to raise awareness about the condition and improve treatment options.
Support Groups and Online Forums
Connecting with others who share similar experiences can be incredibly helpful. Support groups and online forums offer a safe space to share stories, ask questions, and receive encouragement from individuals who understand the challenges you’re facing.
- Online forums: Dedicated forums for women with PCOS often provide a platform for sharing experiences, asking questions, and receiving support from a community of peers.
- Support groups (in-person and online): In-person support groups provide opportunities for face-to-face interaction, fostering a stronger sense of community and connection. Online groups offer similar benefits, but with greater flexibility and accessibility.
- Importance of community: Sharing experiences with others who understand the unique challenges associated with PCOS can provide invaluable emotional support and practical advice.
Healthcare Provider Support
Your healthcare provider plays a vital role in your PCOS journey. Finding a knowledgeable and supportive healthcare provider is essential for managing your condition and pursuing fertility goals.
- Finding a specialist: Look for providers who have experience in treating women with PCOS. They may be endocrinologists, gynecologists, or fertility specialists. Consider asking for recommendations from other women with PCOS or from your primary care physician.
- Communication is key: Open and honest communication with your healthcare provider is crucial. Discuss your concerns, questions, and goals to ensure you receive the best possible care.
- Building a strong relationship: Developing a strong relationship with your healthcare provider can help you feel comfortable discussing your concerns and receiving personalized support.
Finding a Knowledgeable Healthcare Provider
Finding a healthcare provider specializing in PCOS and fertility requires some effort and research. Consider these strategies to identify the right professional for your needs.
- Recommendations: Ask for recommendations from other women with PCOS or your primary care physician.
- Online research: Use online search tools to find providers in your area who specialize in PCOS or fertility.
- Review websites: Look for reviews and testimonials from previous patients to gauge the provider’s experience and communication style.
“Understanding the nuances of PCOS and its impact on fertility requires a specialized approach. A healthcare provider knowledgeable about PCOS can provide tailored support and guidance, helping women navigate their reproductive health journey.”Dr. Emily Carter, Reproductive Endocrinologist
Closing Summary: When To Take A Pregnancy Test If You Have Pcos
In conclusion, taking a pregnancy test when you have PCOS requires a nuanced approach, blending self-awareness, symptom tracking, and professional consultation. By understanding your unique cycle, recognizing potential symptoms, and seeking expert advice, you can navigate the journey of trying to conceive with PCOS with greater confidence and clarity. This knowledge empowers you to make informed decisions and feel more in control of your reproductive health.