Menopause fatty liver disease risk is a growing concern for women as they transition through this life stage. Hormonal shifts during menopause can significantly impact liver health, potentially increasing the likelihood of developing fatty liver disease. This comprehensive guide explores the underlying mechanisms, risk factors, diagnostic methods, and management strategies associated with this condition. We’ll delve into the role of hormones, diet, lifestyle, and genetics in increasing the risk, and examine potential long-term health implications.
This article provides a thorough overview of the complex interplay between menopause, hormonal changes, and the development of fatty liver disease. Understanding the specific risk factors and potential consequences is crucial for women experiencing this transition. We’ll also discuss preventative measures and recommendations to minimize the risk and promote overall well-being.
Introduction to Menopause and Fatty Liver Disease
Menopause, the cessation of menstruation, marks a significant transition in a woman’s life, accompanied by profound hormonal shifts. These hormonal changes, particularly the decrease in estrogen, can impact various bodily functions, potentially increasing the risk of developing certain health conditions. One such condition is fatty liver disease, a prevalent issue with potentially serious long-term consequences. This discussion explores the link between these two critical health aspects.The decrease in estrogen levels during menopause can lead to a cascade of metabolic changes.
Estrogen plays a crucial role in regulating metabolism and glucose control. Its decline can disrupt this delicate balance, potentially contributing to insulin resistance, a condition where the body’s cells don’t respond effectively to insulin. This, in turn, can lead to an accumulation of fat in the liver, a hallmark of fatty liver disease. The interplay between hormonal shifts and metabolic changes during menopause is a complex area of research.
Hormonal Changes During Menopause, Menopause fatty liver disease risk
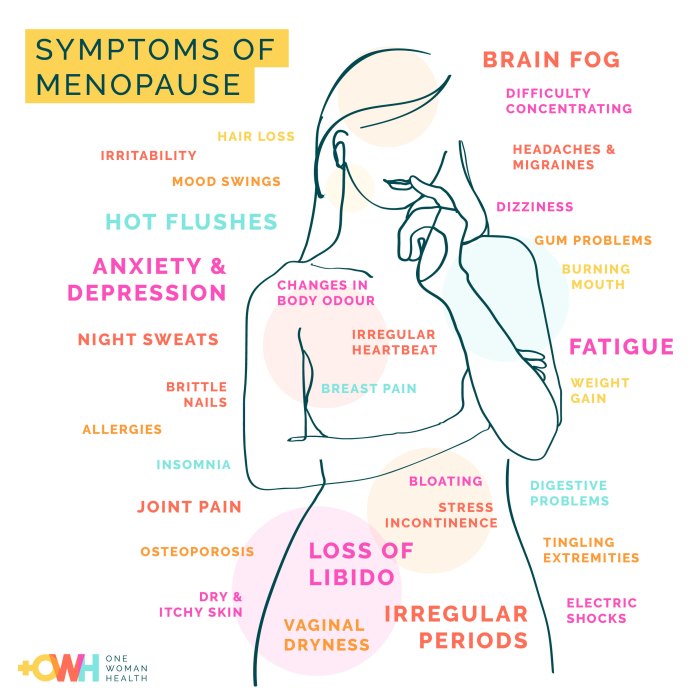
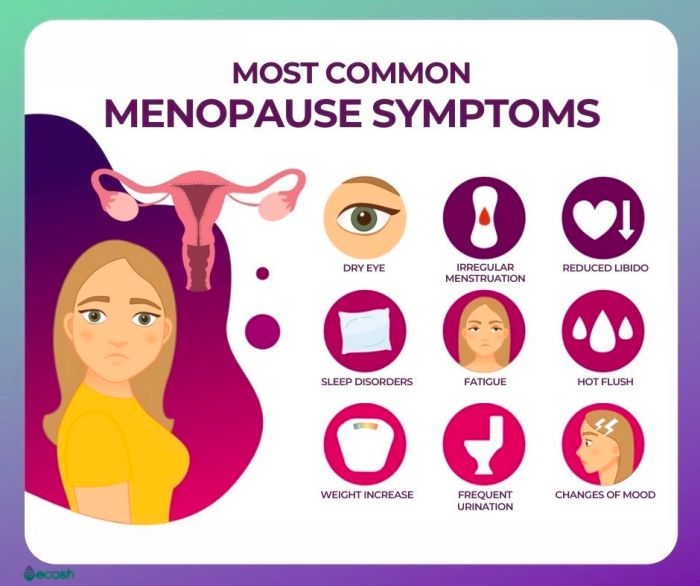
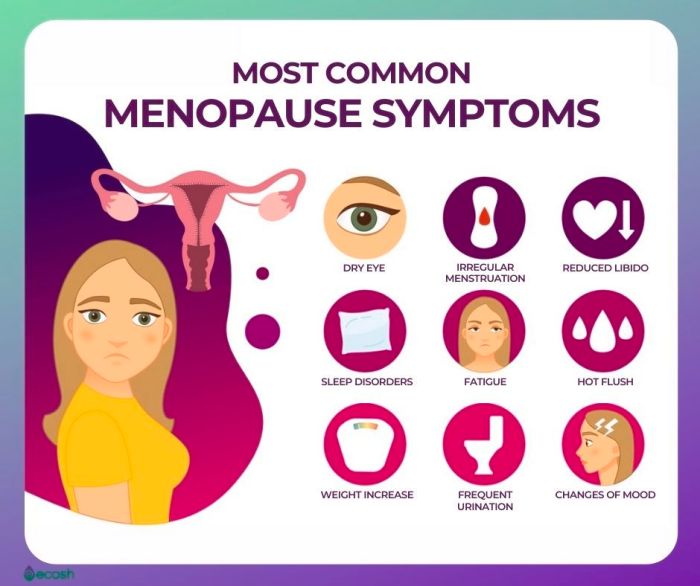
Menopause is characterized by a significant reduction in estrogen and progesterone levels. This decline affects various bodily functions, influencing metabolism, fat distribution, and insulin sensitivity. The loss of estrogen’s protective effects can create a metabolic environment more conducive to the development of fatty liver disease. The reduction in these hormones often leads to an increase in abdominal fat, a known risk factor for metabolic syndrome, which includes insulin resistance and an elevated risk of fatty liver disease.
Mechanisms Linking Menopause and Fatty Liver Disease
The reduction in estrogen levels during menopause can disrupt the delicate balance of metabolism, particularly glucose regulation. This disruption can contribute to insulin resistance, where the body’s cells don’t respond effectively to insulin. As a result, the body may produce more insulin to compensate, further increasing the risk of fat accumulation in the liver. This accumulation of fat within liver cells can lead to inflammation and potentially serious complications.
General Characteristics of Fatty Liver Disease
Fatty liver disease, or hepatic steatosis, is characterized by the accumulation of fat within the liver cells. This buildup can progress to non-alcoholic steatohepatitis (NASH), a more severe form of the disease, potentially leading to cirrhosis and liver failure if left untreated. The accumulation of fat in the liver may not cause noticeable symptoms in its early stages, making it a silent threat.
Prevalence of Fatty Liver Disease in Menopausal Women
Studies suggest a potential link between the increased prevalence of fatty liver disease in menopausal women and the hormonal changes associated with this life stage. However, more research is needed to fully understand the extent of this association. Precise prevalence rates are difficult to pin down due to the complexities in diagnosing and monitoring the condition. It is crucial to recognize that the prevalence is likely higher compared to pre-menopausal women, but the precise figure varies based on factors like ethnicity, lifestyle, and other health conditions.
Potential Contributing Factors to Fatty Liver Disease Risk in Menopausal Women
| Category | Potential Contributing Factors |
|---|---|
| Diet | High intake of processed foods, sugary drinks, and saturated fats. Lack of fruits and vegetables in the diet. |
| Lifestyle | Sedentary lifestyle, lack of physical activity, smoking, and excessive alcohol consumption. |
| Genetics | Family history of fatty liver disease, obesity, or other metabolic disorders. |
| Other Medical Conditions | Polycystic ovary syndrome (PCOS), type 2 diabetes, and high blood pressure. |
| Medications | Certain medications can potentially contribute to liver damage. |
The table above highlights potential contributing factors that may increase the risk of fatty liver disease in menopausal women. Addressing these factors through lifestyle modifications and medical interventions can be crucial in mitigating the risk.
Risk Factors Associated with Menopause Fatty Liver Disease
Navigating the hormonal shifts of menopause can bring about various health concerns, including an increased risk of fatty liver disease. Understanding the contributing factors is crucial for proactive management and prevention. This section delves into the potential dietary, lifestyle, genetic, and activity-related risk factors impacting menopausal women.The transition to menopause is often accompanied by changes in metabolism, body composition, and hormonal balance.
These shifts can create an environment conducive to the development of fatty liver disease, a condition where fat accumulates in the liver. Identifying these risk factors is key to empowering women to make informed choices about their health during this life stage.
Dietary Factors Linked to Increased Risk
Dietary habits play a significant role in the development of fatty liver disease. A diet high in saturated and unhealthy fats, processed foods, and excessive sugar intake can contribute to fat accumulation in the liver. These dietary choices can exacerbate existing metabolic issues and hormonal imbalances common during menopause. Furthermore, inadequate intake of fruits, vegetables, and whole grains can also negatively influence liver health.
Lifestyle Factors Influencing Risk
Beyond diet, lifestyle choices also influence the risk of fatty liver disease in menopausal women. A sedentary lifestyle, characterized by limited physical activity, can disrupt metabolic processes, potentially contributing to fat buildup in the liver. Stress levels and sleep quality can also impact metabolic function, potentially increasing the risk of developing the condition. Insufficient sleep and chronic stress can negatively affect hormone regulation, which is crucial for overall health and can potentially affect the liver.
Impact of Physical Activity Types
The type and intensity of physical activity can influence the risk of fatty liver disease. Aerobic exercise, such as brisk walking, jogging, or cycling, can improve insulin sensitivity and help regulate blood sugar levels. Resistance training, which builds muscle mass, can also contribute to better metabolic health, indirectly reducing the risk of fatty liver disease. A combination of aerobic and resistance training is often recommended for optimal results.
Consistent physical activity can help maintain a healthy weight and reduce visceral fat, which is often associated with an increased risk of fatty liver disease.
Role of Genetics in Predisposition
Genetic factors can also play a role in a woman’s predisposition to fatty liver disease during menopause. A family history of the condition or other metabolic disorders may increase the risk. Inherited genetic variations can affect how the body processes fats and sugars, making some individuals more susceptible to fat accumulation in the liver.
Contrasting Dietary Habits of Women with and without Fatty Liver Disease
| Dietary Habit | Women with Fatty Liver Disease | Women without Fatty Liver Disease |
|---|---|---|
| Saturated and Trans Fats Consumption | High intake of processed foods, fried foods, and red meat. | Moderate intake of healthy fats from sources like avocados, nuts, and olive oil. Emphasis on lean protein sources. |
| Sugar Consumption | High consumption of sugary drinks, desserts, and processed foods. | Limited intake of sugary foods and drinks, focusing on whole fruits and natural sweeteners. |
| Fiber Intake | Low intake of fruits, vegetables, and whole grains. | High intake of fruits, vegetables, and whole grains, providing ample fiber. |
| Portion Sizes | Larger portion sizes and frequent overeating. | Appropriate portion sizes and mindful eating habits. |
| Hydration | Insufficient water intake. | Adequate water intake throughout the day. |
Hormonal Influences During Menopause and Fatty Liver Disease Risk
Menopause marks a significant shift in a woman’s hormonal landscape, and this transition can have profound effects on various bodily functions, including liver health. Understanding the interplay between fluctuating hormones and the development of fatty liver disease is crucial for developing effective preventative strategies. This section will delve into the specific hormonal changes associated with menopause and their impact on liver function, highlighting the role of estrogen, insulin, and cortisol in the risk equation.The hormonal shifts during menopause directly influence metabolic processes within the liver.
While menopause brings a host of changes, one concern is the increased risk of fatty liver disease. This isn’t the only health risk associated with hormonal shifts, though. It’s important to remember that, unlike certain infections, HIV transmission through casual contact is extremely rare, and the risk is significantly lower than often perceived. This is further discussed in a comprehensive resource about hiv transmission casual contact hiv risk.
However, it’s crucial to stay informed about all health risks and adopt healthy lifestyle choices to mitigate potential complications, including those related to menopause and fatty liver disease.
This includes changes in how the liver processes fats, sugars, and other nutrients. These changes can increase the risk of accumulating fat within the liver, potentially leading to fatty liver disease. The intricate relationship between hormonal fluctuations and liver function is a critical area of research, as early intervention can mitigate the risk and severity of fatty liver disease.
Estrogen’s Role in Liver Function
Estrogen plays a multifaceted role in maintaining liver health. It helps regulate lipid metabolism, reducing the accumulation of fat in the liver. During menopause, declining estrogen levels disrupt this delicate balance. Reduced estrogen levels can impair the liver’s ability to clear fat from the bloodstream, leading to a buildup of triglycerides within liver cells. This accumulation is a key factor in the development of non-alcoholic fatty liver disease (NAFLD).
Furthermore, estrogen influences insulin sensitivity, and decreased levels may contribute to insulin resistance, further exacerbating the risk of fatty liver disease.
Impact of Other Hormones
Beyond estrogen, other hormones contribute to the complex interplay influencing liver health during menopause. Insulin resistance is a significant factor. Decreased estrogen levels can negatively impact insulin sensitivity, potentially leading to elevated blood sugar levels. This, in turn, can overload the liver with glucose, which is then converted to fat. Elevated levels of cortisol, often associated with stress, can also increase the risk of fatty liver disease.
Cortisol can interfere with insulin sensitivity and promote fat storage in the liver.
So, I’ve been reading up on menopause and the increased risk of fatty liver disease, which is definitely something to keep an eye on. It got me thinking about how different health conditions can intertwine, and how managing one can impact others. For instance, if you’re living with a pacemaker, living with a pacemaker can bring its own set of challenges and considerations regarding diet and lifestyle, which in turn could subtly influence your risk of developing fatty liver disease during menopause.
All this highlights how important a holistic approach to health is, especially as we navigate different life stages.
Correlation Between Hormonal Levels and Fatty Liver Disease Severity
The following table provides a general overview of the potential correlation between specific hormonal levels and fatty liver disease severity in menopausal women. It’s crucial to remember that this is a simplified representation, and individual responses vary significantly. Further research is needed to establish precise correlations and develop tailored interventions.
| Hormone | Decreased Levels (during menopause) | Potential Impact on Fatty Liver Disease |
|---|---|---|
| Estrogen | Reduced estrogen levels | Impaired fat clearance, increased triglyceride accumulation, potential for insulin resistance |
| Insulin | Reduced insulin sensitivity | Increased glucose levels, greater fat production and storage in the liver |
| Cortisol | Elevated cortisol levels | Impaired insulin sensitivity, promotion of fat storage in the liver, potential for inflammation |
Diagnostic Methods and Management Strategies
Navigating the complexities of fatty liver disease, especially in menopausal women, requires a multifaceted approach. Accurate diagnosis is the first step, followed by a tailored management strategy that considers the unique hormonal and lifestyle factors at play. Understanding the diagnostic tools and management options empowers women to proactively address this potential health concern.Early detection and intervention are crucial for managing fatty liver disease, particularly in the context of menopause.
Effective strategies involve a combination of diagnostic methods, lifestyle modifications, and, in some cases, medical interventions. This section will explore the various approaches used to diagnose and manage fatty liver disease in menopausal women, focusing on prevention and mitigating potential health risks.
Diagnostic Methods for Fatty Liver Disease
Diagnosis of fatty liver disease often involves a combination of assessments to evaluate liver function and identify the underlying cause. These methods provide a comprehensive picture of liver health and potential issues.
- Physical Examination: A thorough physical examination, including a review of symptoms and medical history, is an initial step. This may reveal signs like tenderness in the upper right abdomen, which could suggest liver inflammation or other related conditions. Physical exams also assess overall health and identify associated risk factors, such as obesity or diabetes.
- Blood Tests: Blood tests are fundamental to assess liver function. These tests measure various liver enzymes (like AST and ALT), bilirubin levels, and other markers. Elevated levels of these enzymes can indicate liver inflammation or damage, a key indicator of fatty liver disease. Other blood tests might assess for underlying conditions such as diabetes or high cholesterol, which are frequently linked to the development of fatty liver disease.
- Imaging Techniques: Ultrasound, CT scan, or MRI scans are often employed to visualize the liver and identify any structural abnormalities. Ultrasound is a common, non-invasive technique that uses sound waves to create images of the liver, providing insights into its size, texture, and presence of fatty deposits. These imaging techniques can help differentiate between fatty liver disease and other liver conditions, like cirrhosis.
- Liver Biopsy: A liver biopsy, a procedure involving a small tissue sample, is considered the gold standard for confirming the diagnosis and assessing the severity of fatty liver disease. It provides a direct view of the liver tissue, allowing for the precise identification of fat accumulation and potential inflammation. However, it’s an invasive procedure, and the need for a biopsy is usually determined based on the results of other diagnostic tests and the clinical picture.
Assessment of Liver Health
Assessing liver health involves evaluating various factors beyond just blood tests and imaging. A holistic approach considers the individual’s overall health and lifestyle, including their dietary habits, exercise routine, and underlying medical conditions.
- Dietary Habits: A detailed assessment of dietary habits is vital. A diet high in processed foods, saturated fats, and sugars contributes to fatty liver development. Dietary patterns are crucial for identifying potential risk factors, and nutritional counseling plays a critical role in promoting healthier eating habits.
- Exercise and Physical Activity: Physical activity levels significantly impact liver health. Regular exercise aids in weight management and improves insulin sensitivity, both of which are crucial for reducing fatty liver disease risk. Assessing the individual’s activity level and incorporating strategies to increase physical activity are key steps.
- Underlying Medical Conditions: The presence of underlying medical conditions like diabetes, obesity, or high cholesterol plays a crucial role in assessing liver health. Managing these conditions is often a crucial part of preventing and treating fatty liver disease. Recognizing the interplay between these factors is essential for tailoring effective management strategies.
Management Strategies for Fatty Liver Disease in Menopausal Women
Effective management of fatty liver disease in menopausal women requires a comprehensive approach, combining lifestyle modifications and potentially medical interventions. The strategies should consider the unique hormonal changes and potential risk factors associated with menopause.
- Lifestyle Modifications: Weight loss, a balanced diet, regular exercise, and stress management are crucial for mitigating the risk factors of fatty liver disease in menopausal women. These modifications are vital to support the body’s natural ability to metabolize fats and maintain liver health. Lifestyle changes can significantly impact the progression of the disease.
Treatment Options Comparison
| Treatment Option | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Dietary Modifications | Focus on a balanced diet low in processed foods, saturated fats, and sugars, with an emphasis on fruits, vegetables, and lean proteins. | High | Requires commitment and self-discipline; may require professional guidance. |
| Regular Exercise | Engaging in regular physical activity to promote weight management and improve insulin sensitivity. | High | May lead to muscle soreness initially; requires consistent effort. |
| Medications (e.g., Metformin) | Prescription medications may be used to address underlying conditions like diabetes and improve insulin sensitivity. | Moderate to High, depending on the condition | Potential side effects include gastrointestinal issues. |
| Bariatric Surgery (in severe cases) | Surgical procedures may be considered for significant weight loss in individuals with severe obesity and fatty liver disease. | High, but invasive | Potential surgical risks and long-term complications. |
Long-Term Health Implications
Menopausal women with fatty liver disease face a range of potential long-term health implications. This condition, if left untreated or inadequately managed, can lead to serious complications that impact overall well-being and quality of life. Understanding these implications is crucial for both women and healthcare professionals to proactively address this growing health concern.The progression of fatty liver disease, particularly in menopausal women, is complex and can vary significantly depending on factors like the severity of the initial condition, adherence to treatment plans, and the presence of other underlying health issues.
This necessitates a comprehensive understanding of the potential long-term consequences and the importance of regular monitoring and appropriate interventions.
Potential for Liver Cirrhosis
Fatty liver disease, if chronic, can lead to liver cirrhosis, a serious condition characterized by the replacement of healthy liver tissue with scar tissue. This scarring impairs the liver’s ability to perform its vital functions, including filtering toxins from the blood, producing essential proteins, and regulating blood sugar levels. Cirrhosis can lead to a cascade of complications, including liver failure, which can be life-threatening.
The risk of developing cirrhosis is heightened in menopausal women with fatty liver disease due to hormonal changes and other contributing factors.
Increased Risk of Other Liver Diseases
Beyond cirrhosis, fatty liver disease can increase the risk of other liver-related conditions. These include liver cancer, which is a significant concern given the potential for chronic inflammation and cellular damage associated with fatty liver disease. The combination of hormonal shifts during menopause and the presence of fatty liver disease can create a synergistic effect, potentially accelerating the development of these conditions.
Did you know that menopause can increase your risk of fatty liver disease? It’s a tricky one, and it’s important to consider the other health concerns that can arise with aging. For instance, weakening bones and the risk of fractures are also common as we age. Understanding how to manage osteoporosis fractures treatment and prevention, like proper nutrition and exercise, can help you build strong bones.
This knowledge, in turn, can help maintain a healthy lifestyle to reduce the risk of developing fatty liver disease during and after menopause. osteoporosis fractures treatment and prevention is key to overall wellness.
Impact on Overall Health and Well-being
The long-term implications of fatty liver disease extend beyond the liver itself. The chronic inflammation and metabolic disturbances associated with the condition can impact various organ systems, potentially contributing to cardiovascular problems, diabetes, and other metabolic disorders. Furthermore, the emotional and psychological well-being of women with fatty liver disease can be significantly affected due to the potential for fatigue, pain, and reduced quality of life.
Progression of Fatty Liver Disease in Menopausal Women
| Stage | Description | Potential Complications |
|---|---|---|
| Early Stage (Steatosis) | Fat accumulation in the liver cells. Often asymptomatic or with mild symptoms like fatigue or mild discomfort. | Progression to more severe stages if not addressed. |
| Nonalcoholic Steatohepatitis (NASH) | Inflammation and scarring (fibrosis) alongside fat accumulation. Symptoms may include fatigue, abdominal pain, and jaundice. | Increased risk of cirrhosis, liver failure, and liver cancer. |
| Cirrhosis | Extensive scarring replaces healthy liver tissue. Significant impairment of liver function. Symptoms can range from mild discomfort to severe complications like ascites and encephalopathy. | Potentially life-threatening complications. |
The progression of fatty liver disease is not uniform. Some women may remain in the early stages for years, while others may experience a more rapid progression. Regular medical checkups and lifestyle modifications are crucial for monitoring and managing the condition.
Preventive Measures and Recommendations
Navigating menopause can be challenging, and understanding the increased risk of fatty liver disease is crucial. Fortunately, proactive steps can significantly reduce this risk. Adopting a healthy lifestyle, coupled with regular checkups, empowers women to take control of their health during this transition.Healthy habits are key to mitigating the risk of fatty liver disease, especially during menopause. By focusing on a balanced diet, regular exercise, and consistent medical monitoring, women can significantly lower their chances of developing this condition.
This proactive approach allows for early detection and intervention, which can lead to better long-term health outcomes.
Dietary Strategies for Risk Reduction
A balanced diet plays a pivotal role in preventing fatty liver disease. Choosing nutrient-rich foods and limiting processed foods, sugary drinks, and excessive saturated fats are essential.
- Prioritize whole foods:
- Limit processed foods and sugary drinks:
- Moderate healthy fats:
Focus on fruits, vegetables, lean proteins, and whole grains. These foods provide essential vitamins, minerals, and fiber, which are vital for overall health and support healthy liver function. Examples include colorful fruits like berries and citrus, leafy greens, lean meats like chicken breast or fish, and whole-wheat bread or brown rice.
Processed foods are often high in unhealthy fats, sodium, and added sugars, which can contribute to liver fat buildup. Sugary drinks, such as sodas and juices, should also be limited. Instead of sugary drinks, opt for water, unsweetened tea, or low-fat milk.
Unsaturated fats, found in avocados, nuts, and olive oil, are beneficial for heart health and can help reduce liver fat. However, portion control is essential to avoid excess calorie intake.
Exercise and Physical Activity
Regular physical activity is crucial for overall health and can help prevent fatty liver disease. Moderate-intensity exercise, combined with strength training, can significantly reduce liver fat.
- Incorporate regular exercise:
- Strength training is essential:
- Stay active throughout the day:
Aim for at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking, swimming, or cycling. Combine this with strength training exercises two or more times a week to build muscle mass, which can also contribute to better metabolic health.
Strength training exercises, such as weightlifting or bodyweight exercises, help build muscle mass. Muscle mass plays a role in metabolism and can aid in reducing liver fat.
Incorporate movement into daily routines, such as taking the stairs instead of the elevator or parking further away from your destination. Small, consistent efforts can add up to significant health benefits.
Importance of Regular Medical Checkups
Regular medical checkups and screenings are vital for early detection of fatty liver disease. These checkups allow for proactive interventions and management strategies, improving long-term health outcomes.
- Schedule routine checkups:
- Discuss risk factors with your doctor:
- Attend recommended screenings:
Maintain regular appointments with your doctor for checkups, including blood tests to monitor liver function and other relevant health indicators. This proactive approach enables early detection of potential issues and allows for prompt intervention.
Openly discuss your risk factors with your healthcare provider. This will enable them to tailor recommendations to your specific needs and circumstances.
Follow your doctor’s recommendations for screenings, such as liver function tests, to monitor liver health and detect any potential issues early.
Actionable Steps for Risk Reduction
Implementing these steps can help women lower their risk of developing fatty liver disease during menopause.
- Consult your healthcare provider:
- Maintain a balanced diet:
- Engage in regular physical activity:
- Prioritize regular medical checkups and screenings:
Discuss your risk factors and lifestyle with your doctor to create a personalized plan for risk reduction.
Focus on nutrient-rich foods, limit processed foods and sugary drinks, and moderate healthy fats.
Aim for at least 150 minutes of moderate-intensity aerobic activity per week and incorporate strength training.
Follow your doctor’s recommendations for routine checkups and screenings to monitor your health and detect potential issues early.
End of Discussion: Menopause Fatty Liver Disease Risk
In conclusion, menopause fatty liver disease risk is a multifaceted issue demanding attention. Understanding the hormonal influences, lifestyle factors, and potential long-term health consequences is vital for women navigating this life stage. By implementing preventive measures and maintaining a healthy lifestyle, women can significantly reduce their risk. Remember, proactive health management is key. Regular check-ups and open communication with healthcare providers are essential for early detection and effective management.