Skin boils picture gallery sets the stage for a comprehensive visual guide to understanding these common skin conditions. This resource will provide clear images and descriptions of skin boils at various stages, helping you identify them accurately. We’ll explore different types, potential causes, and even treatment options. Learn how to distinguish skin boils from similar conditions and what preventative measures you can take to minimize their occurrence.
The gallery presents a collection of images illustrating various appearances of skin boils, from small, red bumps to more advanced, pus-filled lesions. Each image is accompanied by detailed descriptions, helping you differentiate between different stages of boil development and identify potential causes. This visual approach will enhance your understanding and enable you to recognize these conditions promptly.
Introduction to Skin Boils
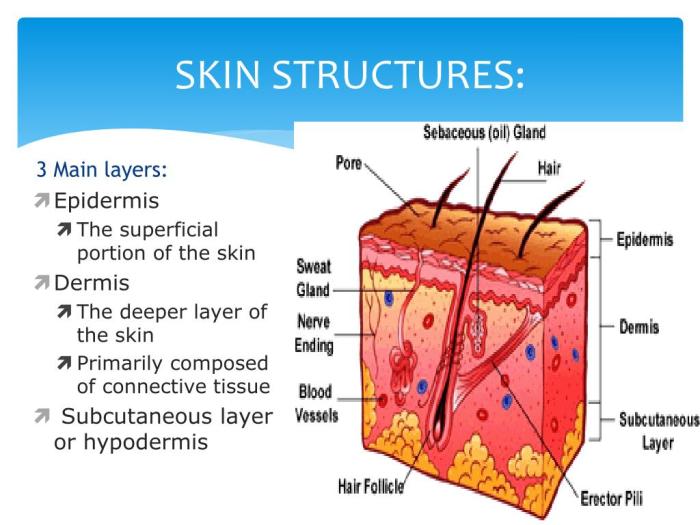
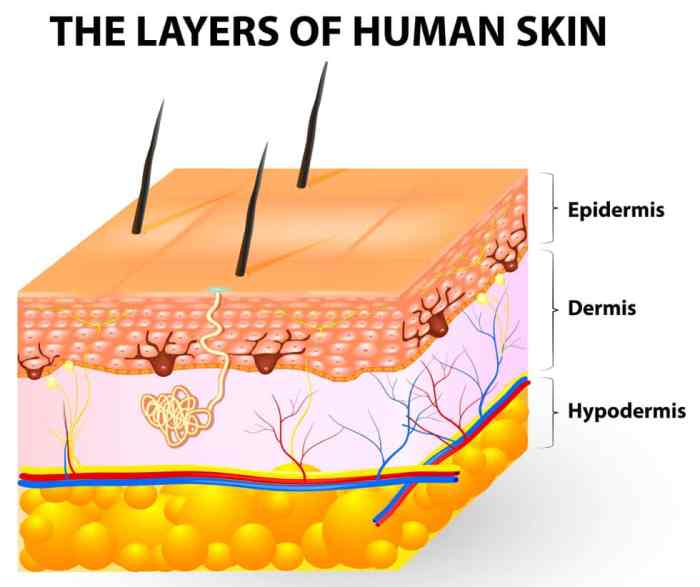
Skin boils, also known as furuncles, are common skin infections that typically present as painful, pus-filled bumps. They are caused by bacterial infections, most frequently Staphylococcus aureus, and often develop in areas with hair follicles. Understanding the causes, symptoms, and types of skin boils is crucial for early recognition and appropriate treatment. Prompt attention to boils can prevent complications and ensure a smoother recovery.Skin boils arise when bacteria, primarily Staphylococcus aureus, infect hair follicles or oil glands in the skin.
Factors contributing to boil formation include poor hygiene, friction or irritation, cuts or abrasions, and weakened immune systems. The bacteria multiply rapidly, causing inflammation and the formation of a pus-filled lesion. Maintaining good hygiene practices, avoiding excessive friction, and treating any cuts or abrasions promptly can significantly reduce the risk of developing skin boils.
Common Causes of Skin Boils
Several factors can contribute to the development of skin boils. Poor hygiene, especially in areas with excessive moisture or friction, can create an environment conducive to bacterial growth. Friction or irritation from clothing, sports equipment, or other sources can damage the skin, leading to an opening for bacterial invasion. Cuts or abrasions, even small ones, provide entry points for bacteria to penetrate the skin.
Weakened immune systems can make individuals more susceptible to skin infections, including boils.
Typical Symptoms of Skin Boils
The characteristic symptoms of a skin boil include a localized, painful, red swelling. The area surrounding the boil may be warm to the touch, and the affected area may be tender to the pressure. A boil usually starts as a small, tender bump that gradually enlarges and becomes increasingly painful. A white or yellow pus-filled head may develop, indicating the presence of infection.
In some cases, fever and malaise may accompany the boil.
Types of Skin Boils
While the term “skin boil” often refers to a furuncle, there are other related skin infections. These infections can present with similar symptoms but may differ in appearance and location.
Classification of Skin Boils
| Boil Type | Typical Appearance | Common Location |
|---|---|---|
| Furuncle (Skin Boil) | A localized, red, painful swelling containing pus. | Face, neck, back, buttocks, legs. |
| Carbuncle | A cluster of interconnected boils, often larger and deeper than a furuncle. Multiple boils in close proximity, with significant inflammation. | Neck, back, buttocks. |
| Hidradenitis Suppurativa | Multiple, painful, pus-filled boils, often occurring in areas with apocrine sweat glands. Deep inflammation, with chronic recurring nature. | Armpits, groin, buttocks. |
A carbuncle, for example, is a cluster of interconnected boils, characterized by significant inflammation and pain. Hidradenitis suppurativa is a chronic condition marked by recurring boils in areas with apocrine sweat glands, often requiring prolonged treatment.
Visual Identification of Skin Boils
Identifying skin boils accurately is crucial for proper treatment and preventing complications. Knowing the different stages of boil development and the various appearances they can take can significantly aid in self-diagnosis and prompt medical intervention if needed. This section delves into the visual characteristics of boils, helping you recognize potential problems early on.Visual identification is a critical step in managing skin boils effectively.
By understanding the typical progression of a boil and the variations in its appearance, you can assess the severity and guide your approach to care.
Different Stages of Boil Development
Understanding the stages of a boil’s development is essential for appropriate management. This progression, from initial inflammation to eventual healing, reveals critical information about the boil’s nature and the potential need for professional medical attention.
| Stage | Description | Image Description |
|---|---|---|
| Early Stage (Inflammation) | The skin around the affected area appears red, swollen, and tender. A small, hard bump may be noticeable, often resembling a pimple. | Imagine a small, raised, red area of skin, slightly swollen and noticeably warmer than the surrounding skin. |
| Maturation Stage (Pus Formation) | The boil continues to enlarge and become more inflamed. A white or yellowish head, containing pus, begins to form in the center. The area around the boil remains painful and swollen. | Visualize a larger, more prominent red bump, with a noticeable, small, white or yellowish center. The area around the bump will be significantly warmer and tender to the touch. |
| Maturation/Suppuration Stage | The boil continues to enlarge and the white or yellowish head, filled with pus, becomes more prominent. The surrounding skin remains inflamed and painful. | Envision a noticeable, larger, and even more prominent red bump. The white or yellowish center containing pus is clearly visible and more significant than in previous stages. The surrounding skin shows increased redness and swelling. |
| Resolution Stage (Healing) | The boil’s head may rupture or be drained. The area will gradually decrease in size and inflammation. The surrounding skin begins to heal. | Imagine a boil with a diminished size and reduced redness. The central area may show signs of drainage, and the surrounding inflammation is subsiding. The skin around the boil is beginning to return to normal. |
Visual Characteristics of Skin Boils
Boils can vary in appearance, size, and location. Recognizing these variations helps in determining the severity and appropriate course of action.
- Small, Red, and Tender: These boils are often in the early stages. The affected area appears as a small, raised red spot that feels warm and tender to the touch. This stage typically precedes pus formation.
- Pus-Filled: As the boil matures, a white or yellowish, pus-filled head often develops. This is a clear indication that the boil has progressed beyond the initial inflammatory stage.
- Inflamed: The surrounding skin around the boil will often show signs of inflammation. This includes redness, swelling, and tenderness. The inflammation typically increases as the boil develops.
Distinguishing Characteristics of Different Types of Skin Boils
Different types of boils may exhibit slightly different characteristics, though these are usually subtle differences. The distinguishing features can help to determine the type of boil and guide appropriate treatment.
| Image Description | Description | Potential Cause | Treatment |
|---|---|---|---|
| A small, superficial boil, often resembling a pimple, with minimal surrounding redness. | Superficial boil, often appearing similar to a pimple, with limited surrounding redness. | Bacterial infection, often caused by Staphylococcus aureus. | Gentle cleaning and warm compresses. If it doesn’t improve or shows signs of spreading, consult a doctor. |
| A larger, deeper boil with a well-defined, pus-filled head. | Deep boil, featuring a noticeable pus-filled head. | Bacterial infection, likely caused by Staphylococcus aureus. | Possible need for incision and drainage, depending on size and location. Follow your doctor’s recommendations. |
Comparison with Similar Skin Conditions

Skin boils, while often easily identifiable, can sometimes be confused with other skin infections. Understanding the key differences in appearance and symptoms is crucial for accurate diagnosis and appropriate treatment. Differentiating boils from similar conditions like carbuncles and folliculitis is vital to prevent misdiagnosis and ensure effective care.Differentiating skin conditions requires careful observation of both the physical presentation and accompanying symptoms.
This comparison will highlight the distinguishing characteristics of boils, carbuncles, and folliculitis, providing practical methods for accurate identification.
Comparison of Skin Boils with Other Conditions
Accurate diagnosis relies on recognizing the unique characteristics of each condition. Boils, carbuncles, and folliculitis, while sharing some superficial similarities, present distinct differences in appearance and progression. Understanding these differences is crucial for appropriate medical intervention.
| Characteristic | Skin Boil | Carbuncle | Folliculitis |
|---|---|---|---|
| Appearance | A localized, pus-filled bump, typically round or oval, ranging from a few millimeters to 2-3 centimeters in diameter. Often red and inflamed. | Larger, deeper, and more extensive infection involving multiple hair follicles. Characterized by a cluster of boils that may merge, creating a larger, inflamed area. | Small, red, inflamed bumps or papules that appear around hair follicles. May be accompanied by small pustules (pus-filled blisters). Often appears as a rash. |
| Size | Generally smaller, typically under 2-3 cm in diameter. | Larger, potentially several centimeters in diameter. | Very small, typically less than 1 cm in diameter. |
| Symptoms | Localized pain, tenderness, swelling, redness, and sometimes warmth. Pus may be visible if the boil is opened. | Severe pain, swelling, redness, and warmth extending over a larger area. Multiple boils may be present, and the affected area might be hard and painful. | Mild to moderate itching, burning, or discomfort. Possible redness and small, inflamed bumps around hair follicles. |
| Location | Can occur anywhere on the skin, but common locations include the face, neck, back, and buttocks. | Commonly found on the back of the neck, the back, or the buttocks. | Can occur anywhere on the body where hair follicles are present. Areas of friction are often affected. |
| Duration | Typically resolves within 1-3 weeks with proper care. | Usually takes longer to heal than a boil, potentially needing several weeks or more. | May resolve in a few days to several weeks depending on the severity. |
Differentiating Methods
Accurate identification of skin conditions requires a multi-faceted approach. Beyond visual inspection, consulting a healthcare professional for diagnosis and treatment is paramount. Physical examination, patient history, and potentially laboratory tests (e.g., culture) are often necessary to differentiate between these conditions.Careful observation of the lesion’s size, location, appearance, and duration, coupled with the patient’s reported symptoms, is essential in the initial assessment.
Ever wondered what skin boils look like? A quick search for “skin boils picture gallery” can be surprisingly helpful in identifying these pesky little infections. But, have you considered that sometimes body aches might be linked to allergies? For example, can allergies cause body aches ? While a picture gallery can help you visualize potential boils, remember to always consult a doctor for proper diagnosis and treatment.
So, if you’re looking for a visual guide, a “skin boils picture gallery” is a good starting point.
The presence of multiple boils or a larger, more extensive area of inflammation strongly suggests a carbuncle.
Ever wondered what skin boils look like? A quick search for “skin boils picture gallery” can be helpful for visual identification. However, if you’re experiencing persistent muscle and joint pain, it could be related to an underlying condition like thyroid disease. Learning more about the connection between these symptoms and thyroid issues can be really beneficial, and resources like this one on muscle and joint pain with thyroid disease can provide valuable insights.
Ultimately, a picture gallery can help you identify the potential cause of skin boils, but a doctor’s visit is always best for a proper diagnosis.
Treatment and Management
Dealing with a skin boil can be frustrating, but understanding the appropriate treatment and management strategies is key to healing effectively and preventing complications. Prompt and targeted intervention can minimize discomfort and promote faster recovery. This section will Artikel common treatment options, home remedies, and when professional medical attention is crucial.
Ever wondered what skin boils look like? A quick search for “skin boils picture gallery” can be a good starting point, but it’s important to remember that visual resources are only part of the story. Understanding the underlying causes and potential connections to cellular aging, like in the cellular aging cancer study , could offer a more complete picture.
Ultimately, a picture gallery can help identify potential issues, but it’s not a substitute for a professional diagnosis.
Common Treatment Options
Various treatment methods are available for managing skin boils, ranging from simple home remedies to more involved professional interventions. Choosing the right approach depends on the severity and location of the boil, as well as individual factors. Effective treatment often involves a combination of approaches.
- Hot Compresses: Applying warm, moist compresses to the affected area can help soften the boil and promote drainage. This facilitates the natural process of healing. The warmth encourages blood flow to the area, aiding in the body’s ability to fight infection.
- Antibiotics: In cases of infected boils, antibiotics may be prescribed to combat the bacteria causing the infection. Oral antibiotics are often effective in treating the underlying infection and preventing further spread. The type and dosage of antibiotics depend on the specific bacteria and the severity of the infection.
- Incision and Drainage: A healthcare professional may need to surgically incise and drain the boil, especially if it is large, deep, or painful. This procedure helps to release pus and other accumulated material, alleviating pressure and promoting healing. Proper aseptic techniques are essential to prevent further infection.
Home Remedies for Managing Skin Boils
While home remedies can sometimes alleviate symptoms and support the healing process, they should not replace professional medical advice, especially for more severe or persistent boils. Consult a doctor before relying solely on home remedies.
- Gentle Cleansing: Keeping the affected area clean is crucial to prevent further infection. Gently wash the area with mild soap and water to remove any debris or bacteria. Avoid scrubbing vigorously, as this could irritate the skin and potentially worsen the condition.
- Avoid Squeezing or Popping: Resist the urge to squeeze or pop the boil. This can spread the infection to surrounding tissues and increase the risk of scarring. If the boil is causing significant pain or discomfort, consult a healthcare professional.
- Over-the-Counter Pain Relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage pain and discomfort associated with the boil. Follow the recommended dosage instructions carefully.
When Professional Medical Attention is Necessary
Certain situations require immediate medical attention for skin boils. Ignoring these signs can lead to serious complications.
- Signs of Severe Infection: Symptoms such as increasing redness, swelling, intense pain, fever, or pus drainage that is foul-smelling should prompt immediate medical attention. These symptoms may indicate a spreading infection.
- Boils that Don’t Respond to Home Care: If a boil does not improve or shows signs of worsening after a few days of home care, a doctor’s evaluation is crucial. This could indicate a more serious underlying issue requiring professional intervention.
- Boils in Sensitive Areas: Boils located in areas like the face, groin, or joints require careful monitoring and professional management to prevent complications and scarring.
Treatment Options Table
| Treatment Option | Description |
|---|---|
| Hot Compress | Applying warm, moist compresses to the affected area to soften the boil and promote drainage. |
| Antibiotics | Oral antibiotics prescribed to combat bacteria causing the infection. |
| Incision and Drainage | Surgical procedure to release pus and other accumulated material, alleviating pressure and promoting healing. |
Prevention and Care
Skin boils, while often treatable, can be frustrating and uncomfortable. Preventing their recurrence involves a multifaceted approach that combines good hygiene, mindful lifestyle choices, and proper wound care. Understanding these factors can significantly reduce the risk of developing boils and help ensure a speedy recovery.Maintaining a proactive approach to hygiene and overall well-being is crucial in preventing boils.
This includes understanding the various contributing factors, from minor irritations to underlying health conditions, and the role they play in boil development. A preventive strategy empowers individuals to take control of their skin health and reduce the chance of future outbreaks.
Preventive Measures to Reduce Boil Risk
Preventing boils requires a comprehensive approach encompassing both lifestyle choices and diligent hygiene practices. A strong immune system, proper hydration, and a balanced diet are essential for overall well-being, reducing the body’s susceptibility to infections that can lead to boils.
- Maintaining Good Hygiene: Regular cleansing of the skin, particularly in areas prone to friction or moisture buildup, is essential. This includes showering or bathing daily, and thoroughly cleaning any cuts, scrapes, or abrasions. Use mild, fragrance-free soaps and avoid harsh scrubbing. Frequent handwashing is vital, especially after touching potentially contaminated surfaces.
- Avoiding Tight-Fitting Clothing: Restricting blood flow and causing friction can increase the risk of skin irritation. Wearing loose-fitting, breathable clothing, particularly in hot and humid environments, is recommended.
- Treating Minor Skin Irritations Promptly: Any minor cuts, scrapes, or abrasions should be cleaned thoroughly and covered with a sterile bandage to prevent infection. Early intervention minimizes the risk of a minor irritation developing into a more serious boil.
Proper Hygiene Practices for Minimizing Boil Development
A consistent routine of proper hygiene practices plays a vital role in reducing the risk of boil formation. This includes daily skin cleansing, avoiding tight clothing, and promptly treating any minor skin irritations.
- Regular Skin Cleansing: Daily showering or bathing, using gentle cleansers, and avoiding harsh scrubbing is important. This helps remove dirt, debris, and bacteria that can contribute to boil development.
- Avoiding Tight-Fitting Clothing: Clothing that restricts blood flow, particularly in areas prone to sweating or friction, can increase the risk of skin irritation and subsequent boil formation. Opt for loose-fitting, breathable fabrics.
- Managing Moisture: Maintaining good skin hygiene, especially in areas prone to moisture buildup, can prevent the growth of bacteria and the subsequent formation of boils.
Wound Care for Preventing Infection
Proper wound care is crucial for preventing infection and minimizing scarring. Cleaning, covering, and monitoring the wound are essential steps in the process.
- Cleaning the Wound: Use clean water and mild soap to gently cleanse the wound. Avoid harsh scrubbing, which can damage the skin.
- Applying a Sterile Dressing: Cover the wound with a sterile bandage to protect it from further contamination and promote healing.
- Monitoring for Signs of Infection: Watch for signs of infection, such as increased pain, swelling, redness, or pus. Seek medical attention if these symptoms develop.
Diet and Lifestyle for Boil Prevention
A balanced diet and healthy lifestyle can contribute significantly to overall well-being, strengthening the immune system and reducing the risk of boil formation.
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains provides essential nutrients to support a healthy immune system. Adequate protein intake is also important for tissue repair.
- Regular Exercise: Physical activity boosts the immune system and promotes overall health.
- Adequate Hydration: Drinking plenty of water helps maintain healthy skin and bodily functions.
Proper Wound Care Techniques to Prevent Infection and Scarring
Proper wound care minimizes the risk of infection and promotes optimal healing. Techniques include cleaning, dressing, and monitoring the wound.
- Gentle Cleansing: Use mild soap and clean water to gently cleanse the wound. Avoid harsh scrubbing.
- Appropriate Dressing: Use sterile dressings to cover the wound and protect it from contamination. Change dressings regularly.
- Monitoring for Infection: Regularly monitor the wound for signs of infection. If any concerns arise, seek medical attention.
Potential Complications
Untreated skin boils can lead to a range of complications, from localized infections to systemic issues. Understanding these potential problems is crucial for timely intervention and preventing severe outcomes. Prompt medical attention is vital for managing complications effectively and preventing long-term health impacts.Complications from untreated skin boils can vary in severity, from localized discomfort to life-threatening conditions. The severity of these complications often depends on several factors, including the location of the boil, the individual’s overall health, and the presence of underlying conditions.
It’s essential to recognize the warning signs of escalating issues and seek appropriate medical care promptly.
Serious Infection, Skin boils picture gallery
Untreated boils can spread infection beyond the initial site. Bacteria from the boil can enter the bloodstream, leading to a systemic infection known as bacteremia. This condition can cause fever, chills, and other serious symptoms, requiring prompt medical attention and potentially intravenous antibiotics. Examples of such infections include cellulitis, which spreads into the surrounding tissue, and even more severe cases like sepsis, a life-threatening response to infection.
Abscess Formation
A boil can develop into a deep abscess, a collection of pus that can cause significant pain and swelling. This can lead to skin damage and scarring if not treated properly. A spreading abscess can necessitate surgical drainage to prevent further tissue damage and systemic infection. This often involves lancing the boil to release the pus, followed by appropriate wound care.
Scarring
While boils typically heal without lasting scarring, deep or persistent boils can result in noticeable scars. The extent of scarring depends on the severity and duration of the boil. Scarring can be minimized by proper treatment and care, including keeping the affected area clean and protected. Early medical intervention is often crucial in reducing the risk of severe scarring.
Lymphadenitis
If the infection spreads to nearby lymph nodes, it can cause lymphadenitis, characterized by swollen and painful lymph nodes. This can be a sign of a more extensive infection, requiring prompt medical evaluation. The affected lymph nodes may become warm to the touch and tender to the press. Antibiotics and sometimes surgical drainage may be required.
Risk Factors for Severe Complications
Certain factors increase the risk of severe boil complications. These include a weakened immune system, underlying health conditions, such as diabetes or autoimmune diseases, and certain medications that can compromise the body’s immune response. Additionally, the location of the boil plays a role, with boils on the face or neck posing a higher risk of spreading infection. Individuals with these risk factors should be especially vigilant about monitoring their boil and seeking medical attention if symptoms worsen.
Signs of Infection Worsening
Several signs indicate a boil is becoming infected. These include increased pain, swelling, redness, warmth, and fever. The area surrounding the boil may also show signs of redness and inflammation. Pus or a foul odor from the boil are further indicators that the infection is worsening. Any increase in these symptoms should prompt a visit to a healthcare provider.
Managing Complications
Managing boil complications involves a combination of medical treatments and self-care. Early diagnosis and treatment are essential for preventing severe outcomes. Medical professionals may prescribe antibiotics to combat infection, surgical drainage to remove pus, and pain relievers to manage discomfort. Proper wound care and hygiene practices are crucial for healing and preventing further complications. Following prescribed medication and maintaining good hygiene will greatly assist in the healing process.
Summary: Skin Boils Picture Gallery
In conclusion, this skin boils picture gallery provides a valuable resource for recognizing and understanding skin boils. By examining the images and descriptions, you can develop a clearer picture of the various stages, types, and potential complications. This knowledge empowers you to seek appropriate medical care and take preventative steps to manage skin boils effectively. Remember, accurate identification is crucial for proper treatment and management.
Early intervention often leads to better outcomes.