Whats a bowel perforation – What’s a bowel perforation? It’s a serious medical condition where a hole develops in the wall of the intestines. This can happen spontaneously, due to trauma, or various underlying conditions like inflammatory bowel disease. Understanding the causes, symptoms, and treatments is crucial for anyone seeking knowledge about this potentially life-threatening issue. This in-depth look explores the intricacies of bowel perforations, from their varied types to the surgical interventions employed for repair.
This comprehensive guide covers the definition, types, causes, symptoms, diagnosis, treatment options, potential complications, and preventive measures related to bowel perforations. We’ll explore the anatomy involved, comparing and contrasting different types of perforations, and examining the potential impact on a patient’s long-term well-being.
Definition and Overview

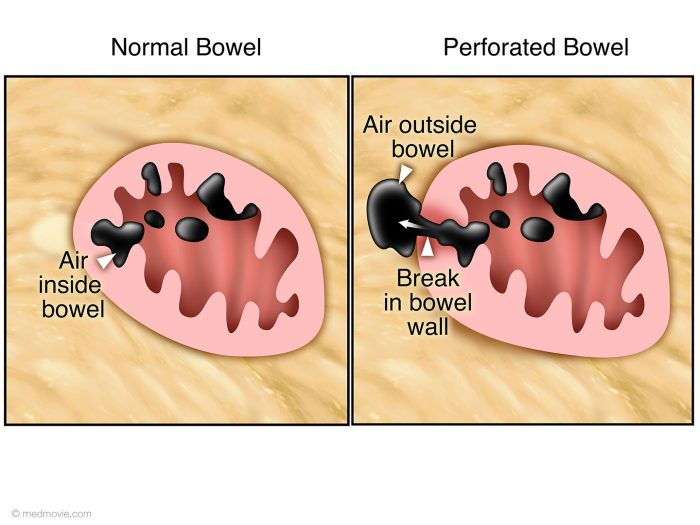
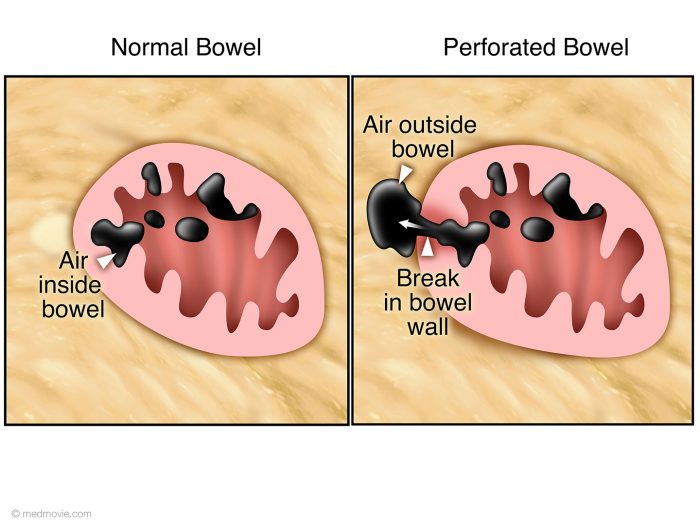
A bowel perforation is a serious medical condition characterized by a hole or tear in the wall of the intestines. This disruption allows the contents of the intestines, which are typically sterile, to leak into the abdominal cavity, potentially causing a life-threatening infection called peritonitis. Understanding the various types, causes, and locations of bowel perforations is crucial for prompt diagnosis and treatment.
Types of Bowel Perforations
Bowel perforations can be categorized based on their cause. Spontaneous perforations occur without an apparent external force, while traumatic perforations are a direct result of injury. These distinctions are important in determining the underlying cause and guiding treatment strategies.
Causes of Bowel Perforations
A range of factors can lead to bowel perforations. Inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis, can cause chronic inflammation that weakens the bowel wall, increasing the risk of perforation. Trauma, including blunt force injuries or penetrating wounds, is another significant cause, especially in accident-prone populations. Foreign bodies, like sharp objects or swallowed objects, can also create a perforation if they penetrate the bowel wall.
Other less common causes include certain infections, tumors, or even certain medications.
Anatomical Locations of Bowel Perforations
Bowel perforations can occur in various locations along the gastrointestinal tract. The small intestine, particularly the ileum, is a frequent site due to its relatively thin wall. The large intestine, including the colon and rectum, can also be affected. The specific location can provide clues to the underlying cause and influence treatment approaches.
A bowel perforation is a pretty serious condition where a hole forms in your intestines. It can lead to some pretty nasty complications, and knowing the first signs of the flu can actually help you identify potential issues with your gut health. Symptoms like fever and muscle aches, similar to those in what are the first signs of the flu , could be a sign of a more serious problem.
It’s crucial to see a doctor if you experience persistent abdominal pain or other concerning symptoms, as early diagnosis and treatment are key for a successful outcome.
Comparison of Bowel Perforation Types
| Type | Cause | Location | Symptoms |
|---|---|---|---|
| Spontaneous | Inflammatory bowel disease (Crohn’s disease, ulcerative colitis), ischemia (reduced blood flow), certain infections, tumors, or medications. | Small intestine (especially ileum), large intestine (colon). Often associated with areas of pre-existing weakness or inflammation. | Abdominal pain (often sudden and severe), fever, nausea, vomiting, tenderness in the abdomen, and signs of peritonitis (like rigid abdomen, rapid pulse, low blood pressure). |
| Traumatic | Blunt or penetrating abdominal trauma (e.g., car accidents, stab wounds, gunshot wounds), or foreign bodies. | Any location along the gastrointestinal tract, depending on the nature and location of the injury. | Symptoms can range from mild to severe and often mimic other conditions. Expect the same general symptoms as spontaneous perforations, but with added symptoms associated with the cause of trauma. |
Symptoms and Diagnosis: Whats A Bowel Perforation
A bowel perforation, a serious medical emergency, can present with a range of symptoms. Prompt recognition and diagnosis are crucial for effective treatment. Early intervention can significantly improve outcomes and minimize complications.Recognizing the subtle signs and distinguishing them from other abdominal conditions is vital for timely diagnosis. Misdiagnosis can delay treatment, potentially worsening the condition. A thorough physical examination and appropriate diagnostic tests are essential for accurate identification.
Common Symptoms of Bowel Perforation
The symptoms of bowel perforation can vary depending on the location and size of the perforation, as well as the individual’s overall health. Common symptoms include severe abdominal pain, often described as sharp, stabbing, or cramping, that may radiate to the back or shoulders. This pain is frequently accompanied by tenderness to the touch in the affected area.
Nausea and vomiting are also common, and fever may develop as the body responds to the infection. In some cases, patients may experience signs of shock, such as low blood pressure and rapid heart rate.
Potential Signs Confused with Other Conditions
Several conditions can mimic the symptoms of bowel perforation, making diagnosis challenging. For instance, appendicitis, gallstones, or even a simple stomach ache can present with similar abdominal pain and tenderness. Accurate diagnosis hinges on a thorough evaluation, considering the patient’s medical history, physical examination findings, and results of diagnostic tests. Careful consideration of the possible differential diagnoses is essential to avoid misdiagnosis.
Physical Examination Findings in Suspected Cases
During a physical examination, the healthcare professional will assess the patient’s vital signs, including temperature, pulse, and blood pressure. They will also examine the abdomen for signs of peritonitis, a condition characterized by inflammation of the lining of the abdominal cavity. Signs of peritonitis include localized tenderness, rigidity (stiffness) of the abdominal muscles, and rebound tenderness (pain when pressure is released).
Distended abdomen, guarding, and diminished bowel sounds may also be observed. The presence of these symptoms and signs, along with the patient’s history, helps the physician to suspect a possible bowel perforation.
Diagnostic Tests for Bowel Perforation
Several diagnostic tests are employed to confirm a bowel perforation. These tests help to visualize the affected area and identify the presence of free air or fluid under the diaphragm. These tests can aid in the accurate identification and characterization of the perforation.
Diagnostic Procedures and Expected Findings
| Procedure | Expected Findings in Bowel Perforation |
|---|---|
| Abdominal X-ray | Presence of free air under the diaphragm (pneumoperitoneum), which indicates a perforation. Additionally, distention of the bowel, and localized soft tissue swelling might be observed. |
| CT Scan | CT scans provide detailed images of the abdomen and pelvis. A bowel perforation is characterized by the presence of free air or fluid in the peritoneal cavity, as well as evidence of inflammation or fluid collections around the affected area. The CT scan can help determine the size, location, and extent of the perforation. |
| Ultrasound | Ultrasound can be used to assess the abdomen and pelvis, but it is less sensitive than X-ray or CT scan for detecting free air in the abdomen. It can be used as a preliminary test to evaluate for other conditions, but is not typically the first-line diagnostic test for bowel perforation. |
Treatment and Management
Treating a bowel perforation requires immediate and decisive action. Prompt diagnosis and appropriate intervention are crucial to minimize complications and maximize patient outcomes. The goal is to control the infection, repair the damaged bowel, and support the body’s healing process. This involves a multifaceted approach that combines initial stabilization, surgical repair, and meticulous post-operative care.
Initial Treatment Approaches
Initial management focuses on stabilizing the patient and preventing further complications. This includes administering intravenous fluids to maintain hydration and blood pressure, and administering antibiotics to combat infection. Pain management is also essential to ensure patient comfort and facilitate further treatment. Oxygen therapy may be required to support adequate oxygenation.
Surgical Interventions
Surgical intervention is typically necessary to repair the perforation. The specific surgical approach depends on several factors, including the location and extent of the perforation, the patient’s overall health, and the experience of the surgical team. The primary goal is to close the hole and restore the integrity of the bowel.
Post-Operative Care and Management
Post-operative care is critical for patient recovery. This involves monitoring vital signs, managing pain, and preventing complications like infection and blood clots. Nutritional support, possibly through intravenous feeding or a specialized diet, may be necessary. Close monitoring for any signs of complications is crucial.
Types of Surgical Procedures
Various surgical techniques are employed to repair bowel perforations. The choice of procedure depends on the specific circumstances of each case. Open surgery, or laparotomy, involves a large incision in the abdomen. Minimally invasive techniques, like laparoscopy, use smaller incisions and specialized instruments. The selection process often considers factors such as the patient’s general condition and the surgeon’s expertise.
Table of Surgical Approaches
| Surgical Approach | Description | Advantages | Disadvantages |
|---|---|---|---|
| Laparotomy | A large incision is made in the abdominal wall to directly access and repair the perforation. This allows for a more extensive view and manipulation of the affected area. | Provides excellent visualization and access for complex repairs. Allows for more extensive exploration and potential repair of associated problems. | Larger incision, increased risk of infection, longer recovery time, and more significant scarring. |
| Laparoscopy | Smaller incisions are made in the abdominal wall, and specialized instruments are used to visualize and repair the perforation. This technique uses a camera and small instruments inserted through these incisions. | Smaller incisions, less pain, faster recovery, reduced scarring, and less risk of infection compared to laparotomy. | Limited visualization and manipulation capabilities compared to laparotomy, may not be suitable for complex or extensive repairs, and requires specialized training and equipment. |
Complications and Prognosis
A bowel perforation, while serious, doesn’t automatically doom a patient. Understanding the potential complications and the factors influencing recovery is crucial for both patients and medical professionals. The prognosis hinges on swift diagnosis, effective treatment, and the individual’s overall health. The long-term effects can vary widely, depending on the severity of the perforation and the effectiveness of the interventions.The path to recovery is often complex, filled with potential hurdles.
This section will delve into the possible complications, highlighting the factors that can impact a patient’s journey and the long-term outlook. This knowledge empowers both patients and healthcare providers to navigate the challenges of bowel perforation with a clearer understanding of the potential outcomes.
Potential Complications from Bowel Perforation
Bowel perforations, if not promptly addressed, can lead to a cascade of complications. These range from localized infections to life-threatening systemic issues. The severity of these complications often depends on the location of the perforation, the size of the opening, and the body’s ability to mount an effective defense against infection.
Factors Influencing Prognosis
Several factors significantly influence the prognosis of bowel perforation. These factors encompass the patient’s overall health, the extent of the damage, the timeliness of diagnosis and treatment, and the individual’s response to medical interventions. A patient with pre-existing conditions like diabetes or weakened immunity may face a more challenging recovery. Likewise, the location of the perforation and the presence of accompanying injuries can also affect the prognosis.
A delay in seeking medical attention can increase the risk of complications and negatively impact the outcome.
Long-Term Consequences of Bowel Perforations
The long-term consequences of bowel perforations can be significant. These may include chronic abdominal pain, adhesions, and a heightened risk of future complications. Patients might experience persistent discomfort or digestive issues that impact their quality of life. Furthermore, the need for repeated surgeries or ongoing medical management can lead to a reduced ability to perform daily activities.
It’s crucial to understand that the severity of long-term consequences varies greatly depending on the individual and the nature of the perforation.
A bowel perforation is a serious medical condition where a hole develops in the bowel wall. This can lead to a whole host of complications, and it’s important to get prompt medical attention if you suspect something like this. While on the topic of food sensitivities, it’s important to consider if something like almond extract is safe for those with tree nut allergies, as it can sometimes contain trace amounts of nuts.
To learn more about the safety of almond extract for those with tree nut allergies, check out this informative article: is almond extract safe for a tree nut allergy. Ultimately, understanding the risks and precautions associated with bowel perforations is crucial for overall health.
Post-Surgical Complications, Whats a bowel perforation
Surgical repair is a common treatment for bowel perforations. However, even successful surgery can be followed by a range of complications.
A bowel perforation is a hole in the bowel, which can be quite serious. It often leads to complications, like infection. Interestingly, dehydration can mimic some of the symptoms of a bowel perforation, especially in the elderly. For instance, confusion and decreased urine output, common signs of dehydration in the elderly, can sometimes be mistaken for symptoms of a bowel perforation.
Learning to recognize the specific symptoms of dehydration in the elderly is crucial for proper diagnosis and treatment. If you suspect a bowel perforation, seek medical attention immediately. symptoms of dehydration in elderly can be tricky to differentiate from other conditions.
- Infection: Post-operative infections are a significant concern. These infections can range from localized abscesses to more serious systemic infections. Prompt identification and treatment of infections are vital to prevent further complications.
- Abscess Formation: Abscesses, localized collections of pus, can develop at the surgical site or in surrounding tissues. These can require drainage procedures to resolve.
- Wound Dehiscence: The surgical incision may separate, a condition known as wound dehiscence. This can lead to further infection and potentially require additional surgical intervention.
- Adhesions: Scar tissue formation, or adhesions, can develop between the intestines or between the intestines and surrounding organs. These adhesions can cause blockages and require further surgery.
- Bleeding: Bleeding at the surgical site can occur, requiring intervention to control the bleeding and prevent further complications.
- Nerve Damage: In some cases, surgical procedures can cause damage to nerves in the abdominal area, potentially resulting in pain or other sensory issues.
- Fistula Formation: An abnormal connection between the bowel and other organs or tissues, known as a fistula, can develop post-surgery. These fistulas can lead to complications like leakage of bowel contents and infections.
Prognosis and Recovery
The prognosis for patients with bowel perforations is often tied to the speed of diagnosis, the extent of the damage, and the overall health of the patient. Successful outcomes are highly dependent on swift medical intervention and the patient’s ability to recover from the surgical procedure.
Prevention
Bowel perforations, while often a serious complication, aren’t always inevitable. Understanding the risk factors and taking proactive steps can significantly reduce the likelihood of this happening. By recognizing potential triggers and adopting preventative measures, individuals can lower their risk and maintain better digestive health.Taking a proactive approach to preventing bowel perforations involves recognizing potential risk factors and employing strategies to mitigate those risks.
This includes lifestyle modifications, appropriate medical interventions, and close monitoring for individuals in high-risk groups.
Risk Factors Associated with Bowel Perforations
Various factors contribute to the increased risk of bowel perforations. Understanding these factors is crucial for implementing preventive measures. Conditions like inflammatory bowel disease (IBD), diverticulitis, and certain cancers can weaken the bowel wall, making it more susceptible to perforation. Previous abdominal surgeries, particularly those involving the bowel, can also increase the risk. Additionally, certain medications and underlying medical conditions, such as severe malnutrition or blood clotting disorders, can increase the vulnerability of the bowel.
Preventive Measures for Reducing Bowel Perforation Risk
Implementing preventive measures can effectively reduce the chance of developing a bowel perforation. Maintaining a healthy lifestyle plays a significant role in reducing the risk. This includes a balanced diet rich in fiber, which promotes regular bowel movements and helps prevent constipation. Regular exercise also contributes to overall health and improves bowel function. Avoiding excessive alcohol consumption and maintaining a healthy weight are crucial steps to take.
Strategies to Minimize Bowel Perforations in High-Risk Populations
Specific strategies are essential for minimizing the occurrence of bowel perforations in high-risk populations. For individuals with conditions like diverticulitis or IBD, regular medical check-ups, adherence to prescribed medications, and prompt treatment of flare-ups are paramount. Close monitoring of symptoms, especially abdominal pain, fever, or changes in bowel habits, is critical. This proactive approach allows for early intervention and minimizes the risk of complications.
In cases of pre-existing abdominal conditions, surgeons may recommend prophylactic procedures to reduce the risk of perforation.
Lifestyle Modifications to Lower the Risk of Bowel Perforations
Adopting certain lifestyle modifications can contribute significantly to lowering the risk of bowel perforation. A balanced diet rich in fruits, vegetables, and whole grains is crucial for promoting digestive health. Adequate hydration is also important for maintaining bowel regularity. Managing stress effectively through relaxation techniques and mindfulness can contribute to overall well-being and may indirectly affect bowel health.
Maintaining a healthy weight through regular exercise and a balanced diet is vital. This can reduce the strain on the digestive system and promote overall health.
Preventative Measures for Different At-Risk Populations
| At-Risk Population | Preventive Measures |
|---|---|
| Individuals with Inflammatory Bowel Disease (IBD) | Regular medical check-ups, adherence to prescribed medications, prompt treatment of flare-ups, close monitoring of symptoms. |
| Patients with Diverticulitis | Dietary adjustments focusing on high-fiber foods, regular hydration, and maintaining a healthy weight. Prompt treatment of acute episodes. |
| Individuals with a History of Abdominal Surgery | Following post-operative instructions carefully, attending follow-up appointments, and reporting any unusual symptoms. |
| Individuals with Malnutrition | Addressing underlying nutritional deficiencies, ensuring adequate caloric intake, and consulting a registered dietitian. |
| Patients with Blood Clotting Disorders | Regular medical check-ups, close monitoring of blood clotting factors, and adhering to prescribed medications. |
Summary
In conclusion, bowel perforations represent a critical medical concern demanding prompt attention and comprehensive care. Understanding the various aspects of this condition, from the initial symptoms to the potential complications and preventive strategies, is essential for both patients and healthcare professionals. The information presented here aims to provide a clear understanding of bowel perforations, empowering individuals to make informed decisions about their health and well-being.