Treating ear infections in adults is a crucial aspect of healthcare. This guide delves into the various types, causes, and symptoms of ear infections in adults, offering a detailed overview of diagnosis, treatment options, and preventive measures. Understanding the unique needs of different adult populations, like pregnant women or the elderly, is also emphasized.
From common symptoms like pain and discharge to potential complications like hearing loss, this guide will equip you with the knowledge to navigate this health concern effectively. We’ll explore the diagnostic process, examining various tests and techniques, and compare the effectiveness of different treatment methods, including the use of antibiotics. Ultimately, we’ll equip you with the tools to manage and prevent adult ear infections, ensuring optimal health.
Introduction to Adult Ear Infections
Adult ear infections, also known as otitis media, are inflammations of the middle ear. While often associated with childhood, adults can also experience these infections, albeit with different presentations and potential causes. Understanding the nuances of adult ear infections is crucial for prompt diagnosis and effective treatment.
Types of Adult Ear Infections
Ear infections in adults can manifest in various forms, each with its own characteristics. The most common types include acute otitis media (AOM), chronic otitis media with effusion (OME), and otitis externa (swimmer’s ear). Acute otitis media is characterized by a sudden onset of infection, while chronic otitis media with effusion involves persistent fluid buildup in the middle ear.
Otitis externa, on the other hand, affects the outer ear canal and is often caused by bacterial or fungal infections.
Causes of Adult Ear Infections
Various factors can contribute to adult ear infections. Common causes include bacterial or viral infections, which may spread from other parts of the body, such as the nose or throat. Ear infections can also be a complication of upper respiratory tract infections like the common cold or the flu. Furthermore, impacted earwax, foreign bodies lodged in the ear canal, and certain medical conditions can also predispose individuals to ear infections.
Symptoms of Adult Ear Infections
The symptoms of adult ear infections can vary in severity. Common symptoms include ear pain, which can range from mild discomfort to severe throbbing. Other potential symptoms include hearing loss, a feeling of fullness or pressure in the ear, tinnitus (ringing in the ears), fever, and a discharge from the ear. It is important to note that not all individuals experience all these symptoms, and the specific symptoms and their severity may vary based on the underlying cause and the individual’s overall health.
Risk Factors for Adult Ear Infections
Several risk factors can increase the likelihood of developing an ear infection in adults. These include a history of frequent ear infections, weakened immune systems, certain medical conditions like diabetes or immune deficiencies, exposure to environmental irritants, and a history of smoking. Furthermore, individuals with nasal or sinus problems are also more susceptible to ear infections. Specific professions or hobbies that expose individuals to excessive moisture or irritants in the ear canal can also increase risk.
Treating ear infections in adults can be tricky, sometimes involving antibiotics or other medications. It’s important to remember that certain conditions, like some types of seizures, can mimic ear infection symptoms. For example, atonic seizures, which involve a sudden loss of muscle tone, can sometimes be mistaken for ear infections, especially if they affect the head and neck muscles.
Understanding the different types of seizures, like what are atonic seizures , is crucial for accurate diagnosis and effective treatment. This highlights the importance of proper medical evaluation for any unexplained symptoms.
- Frequent Ear Infections: A history of recurrent ear infections in the past can increase the likelihood of experiencing them again. This could be due to anatomical predisposition or other underlying conditions.
- Weakened Immune Systems: Individuals with weakened immune systems, due to illnesses or medications, are more susceptible to infections, including ear infections.
- Medical Conditions: Certain medical conditions, such as diabetes or immune deficiencies, can compromise the body’s ability to fight off infections, increasing the risk of ear infections.
- Exposure to Irritants: Exposure to environmental irritants, like water or chemicals, can increase the risk of ear infections. For instance, prolonged exposure to moisture in the ear canal, such as in swimming or other water-based activities, can increase the likelihood of developing otitis externa.
- Smoking: Smoking can weaken the immune system and damage the respiratory system, potentially increasing the risk of ear infections.
Diagnosis and Evaluation
Pinpointing the cause of ear discomfort and pain in adults requires a systematic approach. A thorough history, including details about the onset, duration, and characteristics of the pain, is crucial. This information helps differentiate between various potential causes, including ear infections, allergies, or foreign bodies. A careful physical examination, combined with specific diagnostic tests, allows healthcare professionals to accurately identify the problem and develop an appropriate treatment plan.The diagnostic process for adult ear infections involves a combination of subjective and objective assessments.
Subjective data, gathered from patient interviews, includes symptom details and medical history. Objective data, obtained through physical examinations and tests, provides tangible evidence of the condition. The combination of these data points contributes to an accurate diagnosis.
Diagnostic Process for Adult Ear Infections
The diagnostic process for ear infections in adults usually starts with a detailed patient history. This involves asking questions about the onset of symptoms, their duration, associated symptoms, and any contributing factors. Questions may include the location and severity of pain, the presence of discharge, and any recent exposure to potential irritants. The medical history of the patient also provides valuable information, including previous ear infections, allergies, and other relevant medical conditions.
This information helps to narrow down the potential causes and guide further evaluation.
Diagnostic Tests for Adult Ear Infections
Several diagnostic tests are employed to confirm or rule out an ear infection in adults. These tests aim to assess the condition of the middle ear and surrounding structures.
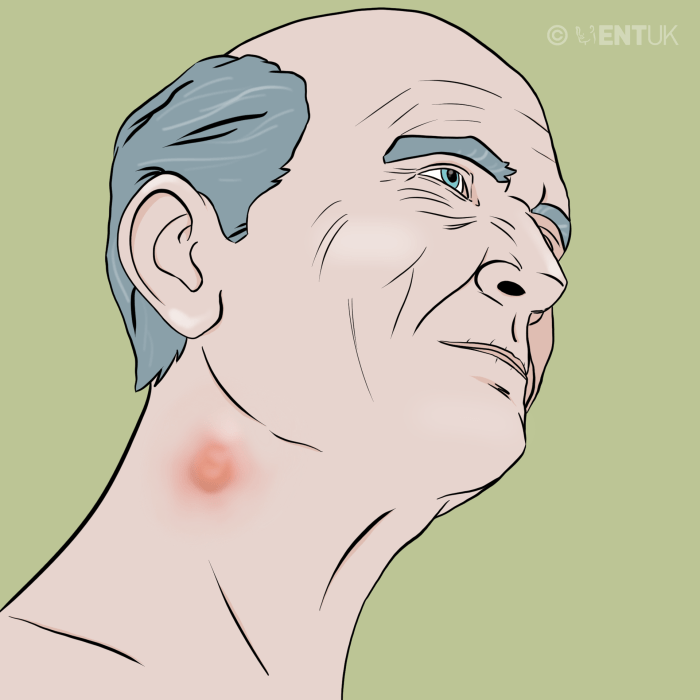
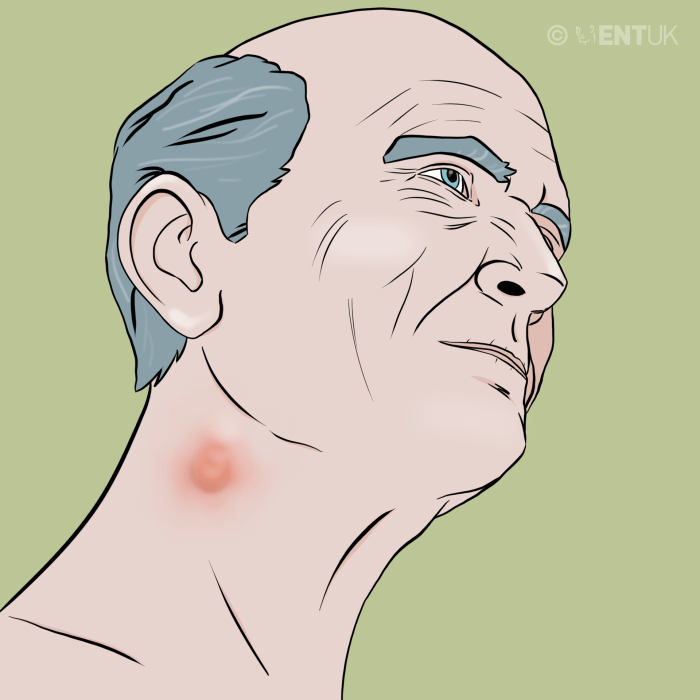
Treating ear infections in adults can be tricky, often requiring a combination of rest and medication. Understanding the different types of skin lesions, like those pictured and discussed in detail at types of skin lesion pictures causes and treatment , can actually provide valuable insight into the underlying causes of some ear infections. This is because certain skin conditions can manifest in similar ways to ear infections, and a proper diagnosis requires a thorough evaluation by a healthcare professional.
Ultimately, remember that self-treating ear infections can be dangerous, so it’s always best to seek medical advice.
- Otoscopic Examination: A crucial initial step, otoscopic examination involves using an otoscope to visually inspect the external ear canal and tympanic membrane (eardrum). This allows the healthcare professional to identify signs such as redness, swelling, fluid buildup behind the eardrum, or perforation of the eardrum. This simple procedure often reveals key clues about the presence and nature of an ear infection.
- Tympanometry: This test measures the mobility of the eardrum in response to air pressure changes. An abnormal tympanogram can indicate fluid in the middle ear, a common finding in ear infections. The test provides an objective measure of eardrum function and helps distinguish between different causes of ear discomfort. Variations in the tympanogram can reflect different degrees of middle ear dysfunction.
- Acoustic Reflex Testing: This procedure assesses the response of the middle ear muscles to sound. Reduced or absent acoustic reflexes can be a sign of inflammation or fluid in the middle ear. It provides a physiological response related to the ear’s functioning in relation to sound stimuli. This can be particularly useful in identifying subtle signs of infection.
- Imaging Studies (e.g., CT or MRI): In some cases, imaging studies like computed tomography (CT) or magnetic resonance imaging (MRI) may be necessary to evaluate the structures of the inner ear or identify complications like mastoiditis (infection of the bone behind the ear). These are typically reserved for more complex cases where the diagnosis remains unclear after other tests. Imaging can provide detailed images of the inner ear and surrounding tissues.
Comparing Diagnostic Methods
| Diagnostic Method | Accuracy | Effectiveness | Limitations |
|---|---|---|---|
| Otoscopic Examination | High | Simple, quick, and inexpensive | Subjective interpretation; may not detect subtle issues |
| Tympanometry | Moderate to High | Objective measure of eardrum function | May not always distinguish between different types of middle ear problems |
| Acoustic Reflex Testing | Moderate | Provides physiological response to sound | Can be affected by other conditions; requires specialized equipment |
| Imaging Studies | High | Detailed view of the inner ear and surrounding tissues | More invasive; higher cost; potential exposure to radiation |
Patient Interview Questions
A thorough interview with the patient can provide valuable clues for diagnosis. The questions below can guide the process.
- Detailed description of the ear pain: This includes location, intensity, and duration.
- Presence of ear discharge: If present, the color, consistency, and amount should be noted.
- Associated symptoms: Such as fever, headache, or dizziness should be recorded.
- Medical history: Previous ear infections, allergies, and other relevant medical conditions.
- Recent exposure to potential irritants: Such as loud noises or water.
Treatment Options
Treating adult ear infections often involves a multifaceted approach tailored to the specific type and severity of the infection. The goal is to alleviate pain, reduce inflammation, and eliminate the causative pathogens. This often involves a combination of medications, lifestyle adjustments, and, in some cases, surgical intervention.Effective treatment hinges on accurate diagnosis and a thorough understanding of the infection’s underlying cause.
Different types of ear infections may respond differently to various treatments, highlighting the importance of personalized care.
Medication Options
A common approach to treating ear infections involves medications that target the infection’s causative agents. These may include antibiotics, anti-inflammatory drugs, and pain relievers. The selection and dosage of these medications depend on the specific diagnosis and the patient’s overall health.
- Antibiotics: Antibiotics are typically prescribed when bacterial infection is suspected or confirmed. They work by killing or inhibiting the growth of bacteria. However, the overuse of antibiotics can lead to antibiotic resistance, a significant public health concern. Therefore, their use is carefully considered by healthcare professionals. Appropriate antibiotic selection is crucial for effective treatment and minimizing the risk of resistance.
- Pain Relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and discomfort associated with ear infections. These medications are often used in conjunction with other treatments to manage symptoms. Careful consideration of potential side effects and interaction with other medications is essential. Following recommended dosages is paramount.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help reduce inflammation in the ear. This can help alleviate pain and pressure associated with the infection. It’s important to be aware of potential side effects and contraindications before taking these medications. Consult a doctor before using these medications.
Effectiveness of Different Treatments
The effectiveness of a treatment approach depends on several factors, including the type of infection, the severity of the symptoms, and the individual’s overall health. Some infections respond well to conservative treatment, while others may require more aggressive intervention.
Treating ear infections in adults can be tricky, sometimes requiring antibiotics. While dealing with the discomfort, you might also find yourself needing a soothing solution for other skin irritations. A great option for a rash, like those sometimes accompanying ear infections, is calamine lotion for rash calamine lotion for rash. This can help calm the itch and inflammation, allowing you to focus on your ear infection recovery.
- Bacterial Infections: Bacterial ear infections typically respond well to antibiotic therapy when administered correctly. However, delayed or inadequate treatment can lead to complications like hearing loss or mastoiditis. Prompt and appropriate antibiotic use is critical.
- Viral Infections: Viral ear infections often resolve on their own without specific treatment. Symptomatic relief through pain relievers and rest is usually sufficient. The focus is on managing symptoms and supporting the body’s natural healing processes. Antibiotics are generally not effective against viral infections.
Antibiotic Use
“Antibiotics should be used judiciously and only when bacterial infection is confirmed or strongly suspected.”
The use of antibiotics in treating ear infections is a critical consideration. Their overuse can contribute to the development of antibiotic-resistant bacteria, making future infections harder to treat. Careful diagnosis and consideration of the potential benefits and drawbacks of antibiotic use are essential.
Common Medications and Dosage
| Medication | Dosage (Typical) | Potential Side Effects |
|---|---|---|
| Amoxicillin | 500 mg orally three times a day for 7-10 days | Nausea, diarrhea, allergic reactions |
| Ibuprofen | 200-400 mg every 4-6 hours as needed | Stomach upset, kidney problems (in high doses or with pre-existing conditions) |
| Acetaminophen | 325-650 mg every 4-6 hours as needed | Liver damage with high doses or prolonged use |
Note: This table provides general information. Specific dosages and treatment plans should always be determined by a healthcare professional based on individual patient needs. Consult your doctor for personalized advice.
Management and Prevention
Managing adult ear infections effectively involves a multi-faceted approach that goes beyond simply treating the symptoms. A crucial aspect is understanding the specific cause of the infection, whether bacterial, viral, or fungal, to tailor the management strategy appropriately. This often necessitates a consultation with a healthcare professional for accurate diagnosis and personalized recommendations.Effective management often involves a combination of medical interventions, lifestyle adjustments, and home remedies.
This approach aims to reduce discomfort, promote healing, and prevent potential complications. The choice of treatment, whether medication or alternative methods, should be made in consultation with a medical professional.
Strategies for Managing Adult Ear Infections
Effective management of ear infections involves a combination of strategies, including medication, lifestyle adjustments, and home remedies. It is essential to consult with a healthcare provider to determine the best course of action. The specific treatment will depend on the cause and severity of the infection.
Home Remedies and Lifestyle Changes
Several home remedies and lifestyle changes can aid in managing adult ear infections. However, it is crucial to emphasize that these should be used in conjunction with professional medical advice, not as a replacement.
- Avoiding Irritants: Reducing exposure to irritants like smoke, dust, and excessive noise can help minimize inflammation and discomfort. For example, individuals working in noisy environments may need to wear earplugs to prevent further irritation.
- Maintaining Hydration: Staying well-hydrated is essential for overall health and can also aid in reducing inflammation. Drinking plenty of fluids helps to thin mucus and promote healing.
- Applying Warm Compresses: Applying warm compresses to the affected ear can help relieve pain and discomfort. A warm, damp cloth placed gently on the outside of the ear for a few minutes can provide some relief.
- Avoiding Swimming and Water Activities: If an infection is present, avoiding activities that introduce water into the ear canal is important. This prevents further irritation and infection.
Importance of Follow-up Care
Following up with a healthcare professional after treatment is critical for monitoring the healing process and ensuring the infection is completely resolved. Regular check-ups allow for the identification of any potential complications or recurrence. This is particularly important for individuals with chronic ear infections or underlying health conditions. Regular check-ups help ensure the infection is completely resolved, and preventative measures can be put in place to avoid recurrence.
Preventing Adult Ear Infections
Proactive measures can significantly reduce the risk of developing ear infections. Prevention involves a combination of lifestyle changes and good hygiene practices.
- Practicing Good Hygiene: Maintaining good hygiene practices, such as washing hands frequently, can help prevent the spread of infections. This is especially crucial when dealing with children or other individuals who may be more susceptible to infections.
- Avoiding Irritants: As mentioned before, minimizing exposure to irritants such as smoke, dust, and excessive noise can reduce the risk of inflammation and infection.
- Proper Ear Cleaning: Cleaning the outer ear with a soft cloth or cotton ball can remove excess wax and debris. However, avoid inserting objects into the ear canal, as this can cause damage and potentially introduce infection.
- Avoiding Water in the Ear Canal: Taking precautions to avoid water entering the ear canal, especially during swimming or bathing, can help prevent infections.
Preventative Measures for Adults
The following preventative measures can help adults reduce the risk of ear infections. These measures, when combined with good hygiene, can significantly reduce the likelihood of infection.
- Regular Check-ups: Scheduling regular check-ups with a healthcare provider is important to address any potential ear problems promptly.
- Avoiding Irritants: Minimizing exposure to irritants like dust, smoke, and loud noises can help prevent ear inflammation.
- Proper Ear Care: Cleaning the outer ear carefully and avoiding the use of cotton swabs or other objects to clean the ear canal.
- Safe Water Activities: Taking necessary precautions to avoid water entering the ear canal during swimming, showering, or bathing.
Complications and Long-Term Effects: Treating Ear Infections In Adults

Untreated or inadequately treated ear infections in adults can lead to a range of complications, impacting hearing and overall health. Understanding these potential consequences is crucial for timely diagnosis and effective management. Prompt medical attention and adherence to treatment plans are vital in preventing serious long-term effects.
Potential Complications of Untreated Ear Infections
Untreated or inadequately treated ear infections can progress to more serious conditions. These complications can range from localized issues to systemic problems, highlighting the importance of seeking professional medical care.
- Mastoiditis: An infection that spreads from the middle ear to the mastoid bone behind the ear. This can result in pain, swelling, and potentially, serious complications if left untreated. For example, a patient with a chronic ear infection that fails to respond to antibiotics may develop mastoiditis, requiring surgical intervention.
- Facial Nerve Paralysis: Inflammation or infection around the facial nerve can lead to temporary or permanent facial weakness or paralysis. This complication can occur if the infection extends to nearby tissues and structures. A severe case of acute otitis media might involve facial nerve involvement, especially in cases of chronic otitis media.
- Cholesteatoma: A benign but potentially destructive growth that can form in the middle ear. This can lead to ongoing ear infections, hearing loss, and even damage to the surrounding structures. This is often a long-term complication of recurrent ear infections, especially in cases of chronic otitis media.
- Meningitis: In rare but severe cases, an infection can spread from the middle ear to the meninges, the membranes surrounding the brain and spinal cord. This can result in meningitis, a life-threatening condition requiring immediate medical attention. This is a particularly serious complication that can occur with a neglected infection that reaches the meninges.
Long-Term Effects on Hearing
Chronic ear infections, even if initially treated, can lead to permanent hearing loss. The damage to the delicate structures of the middle ear, such as the eardrum and ossicles, can impair sound transmission.
- Conductive Hearing Loss: Damage to the structures in the middle ear, preventing sound waves from reaching the inner ear effectively. This can lead to difficulty hearing certain sounds, particularly quieter ones. For instance, if the eardrum is perforated due to repeated infections, conductive hearing loss can result.
- Sensorineural Hearing Loss: Damage to the inner ear or auditory nerve, affecting the ability to perceive sound. This type of hearing loss is often permanent. A prolonged period of untreated otitis media could potentially cause sensorineural hearing loss, impacting the delicate inner ear structures.
Severity and Potential Complications
The severity of the infection can directly impact the likelihood and type of complications.
| Severity Level | Description | Potential Complications |
|---|---|---|
| Mild | Localized infection, mild pain, minimal discomfort. | Rare complications; prompt treatment usually prevents issues. |
| Moderate | Moderate pain, swelling, possible fever. | Mastoiditis, facial nerve involvement, possible hearing loss. |
| Severe | High fever, intense pain, difficulty swallowing. | Mastoiditis, facial nerve paralysis, meningitis, hearing loss. |
Severity and associated complications should be carefully assessed by a medical professional. This table provides a general overview; individual experiences may vary.
Special Considerations and Populations
Treating ear infections in adults requires careful consideration of individual patient factors, particularly for specific populations. Age, medical history, lifestyle, and pre-existing conditions can significantly impact treatment strategies and outcomes. Understanding these variations is crucial for tailoring care to meet the unique needs of each patient and maximizing their recovery.
Pregnant Women
Pregnant women face unique challenges during ear infection treatment. Certain medications may not be suitable for use during pregnancy due to potential risks to the developing fetus. Consultations with both the obstetrician and the otolaryngologist are essential for safe and effective management. The use of topical ear drops, while generally safe, should still be carefully considered in the context of pregnancy.
Alternatives like oral antibiotics, when appropriate, are preferred to minimize risks.
Elderly Adults, Treating ear infections in adults
Elderly adults often have co-existing medical conditions that can influence treatment decisions. Their immune systems may be compromised, potentially leading to more severe or prolonged infections. Careful consideration of medication dosages and potential drug interactions is vital. For example, some medications used to treat ear infections might interact with other medications the elderly patient is already taking.
Therefore, close monitoring and potential adjustments to treatment protocols are necessary.
Immunocompromised Individuals
Immunocompromised individuals, including those with weakened immune systems due to conditions like HIV/AIDS or undergoing chemotherapy, are at a higher risk of developing severe ear infections. Their bodies may struggle to fight off infections effectively. Treatment protocols need to be tailored to address the weakened immune response. Longer durations of antibiotics or different antibiotic choices may be required.
Careful monitoring and aggressive management are crucial to prevent complications.
Patient-Specific Factors
Individual patient factors play a significant role in treatment planning. A comprehensive medical history, including allergies, previous reactions to medications, and lifestyle choices, must be taken into account. Dietary habits, for instance, can influence the severity and duration of the infection. A detailed understanding of the patient’s overall health picture is essential to develop a personalized treatment plan.
Summary Table of Treatment Approaches
| Population | Key Considerations | Treatment Adjustments |
|---|---|---|
| Pregnant Women | Potential risks to fetus; avoiding certain medications | Prioritize oral antibiotics over topical drops; close collaboration with obstetrician |
| Elderly Adults | Co-existing medical conditions; potential immune compromise | Careful medication selection; lower dosages; close monitoring for interactions |
| Immunocompromised Individuals | Weakened immune response; higher risk of severe infection | Longer antibiotic durations; different antibiotic choices; aggressive management |
| General Patient Factors | Comprehensive medical history, allergies, lifestyle | Personalized treatment plan; adjustments based on individual needs |
Illustrative Case Studies

Understanding adult ear infections requires a nuanced approach, as symptoms and responses to treatment can vary significantly. This section will delve into case studies to illustrate the complexities of diagnosing and managing these conditions, emphasizing the importance of personalized care.Case studies provide a framework for understanding the clinical presentation, diagnostic process, and treatment decisions for ear infections in adults.
They highlight the critical role of patient history, physical examination findings, and diagnostic tests in determining the appropriate course of action. These examples showcase how different factors influence the management of adult ear infections, highlighting the importance of individualized treatment plans.
Case Study 1: Chronic Otitis Media
A 45-year-old female presented with a persistent, dull ache in her right ear, accompanied by a feeling of fullness and occasional mild tinnitus (ringing in the ear). She reported a history of recurrent ear infections, treated with antibiotics in the past, but with limited success. She also noted a mild conductive hearing loss in the affected ear.The diagnostic process began with a comprehensive history taking, which included inquiries about past medical history, medications, and any recent illnesses.
A physical examination revealed a slightly bulging tympanic membrane (eardrum) in the right ear, and a mild swelling of the surrounding tissues. Otoscopic examination revealed signs of chronic inflammation. This was followed by an audiogram to evaluate hearing levels and a tympanometry to assess middle ear pressure. The audiogram revealed a moderate conductive hearing loss. Tympanometry showed reduced compliance, suggesting a possible effusion in the middle ear.
A CT scan of the temporal bone was performed to rule out any structural abnormalities or complications. The imaging results were unremarkable.Given the patient’s history of recurrent infections and the findings from the diagnostic tests, a diagnosis of chronic otitis media with effusion was made. Treatment focused on addressing the underlying inflammation and reducing the risk of further complications.
The patient was prescribed a course of oral antibiotics, along with a decongestant. She was also instructed on the use of ear drops containing a steroid to reduce inflammation and pain. Regular follow-up appointments were scheduled to monitor the progress and adjust the treatment plan as needed.The patient experienced a significant reduction in symptoms after several weeks of treatment.
Her hearing improved, and the feeling of fullness and pain subsided. This case highlights the importance of comprehensive diagnostic evaluation, considering the patient’s history, and tailoring treatment to address the underlying cause of the chronic ear infection.
Case Study 2: Acute Otitis Externa
A 62-year-old male presented with severe pain, redness, and swelling in the external ear canal. He reported a history of swimming in chlorinated pools recently. The pain was described as sharp and throbbing, increasing with movement of the affected ear. He also reported difficulty hearing and slight fever.The diagnostic process was relatively straightforward in this case. A visual examination of the external ear canal was performed, revealing signs of inflammation and swelling.
Otoscopic examination revealed redness and swelling in the external ear canal. The physician also assessed the patient’s overall health and vital signs.Given the patient’s symptoms and physical examination findings, a diagnosis of acute otitis externa (swimmer’s ear) was made. Treatment involved administering topical ear drops containing antibiotics and corticosteroids to address the infection and reduce inflammation. Pain management was crucial and included over-the-counter pain relievers.
The patient was instructed to keep the affected ear dry and avoid further exposure to water.The patient responded well to the treatment, and the pain and swelling subsided within a few days. He was advised to continue using the ear drops as prescribed and to follow up with the physician for any lingering symptoms. This case underscores the importance of prompt diagnosis and treatment, particularly when dealing with painful and potentially debilitating conditions like acute otitis externa.
Final Thoughts
In conclusion, treating ear infections in adults requires a multifaceted approach, encompassing understanding the diverse causes, symptoms, and diagnostic methods. This guide has highlighted the importance of personalized treatment plans, considering individual patient factors. We’ve explored treatment options, preventive strategies, and potential complications to provide a complete picture. Remember, seeking timely medical attention is key to effective management and minimizing long-term effects.