Macular telangiectasia type two (MT2) is a chronic eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. This guide delves into the intricacies of MT2, exploring its characteristics, causes, diagnosis, management strategies, and the impact it has on patients’ lives. We’ll cover everything from the early stages to the latest research, providing a thorough understanding of this complex condition.
This detailed overview of macular telangiectasia type two will cover its key characteristics, the typical age of onset, prevalence, and common risk factors. We’ll also discuss the impact of MT2 on daily activities and quality of life, alongside a detailed summary of its key features in a table. Understanding the pathophysiology, including vascular abnormalities, cellular and molecular processes, will also be explored, and will contrast this with other macular diseases.
Macular Telangiectasia Type 2: A Detailed Overview: Macular Telangiectasia Type Two
Macular telangiectasia type 2 (MT2) is a chronic, progressive eye disease that affects the macula, the central part of the retina responsible for sharp, central vision. Understanding this condition is crucial for early detection and appropriate management, enabling individuals to maintain their quality of life. It’s important to remember that while MT2 can impact vision, proactive measures and ongoing care can help individuals cope effectively.
Defining Macular Telangiectasia Type 2
Macular telangiectasia type 2 (MT2) is characterized by the abnormal dilation and widening of small blood vessels (telangiectasia) within the macula. This process leads to fluid leakage and damage to the delicate tissues of the macula. The resulting changes can significantly impact vision acuity, especially the ability to see fine details. The progressive nature of the disease can lead to gradual vision loss over time.
Key Characteristics and Visual Features
MT2 typically presents with a characteristic appearance of dilated blood vessels in the macula, visible through an ophthalmoscopic examination. Patients may experience gradual blurring or distortion of central vision, which can progress to a loss of central vision. Individuals might notice difficulty reading, recognizing faces, or driving. Other visual features include metamorphopsia, where straight lines appear wavy or distorted, and scotomas, or blind spots in the central vision field.
Age of Onset and Prevalence
The typical age of onset for MT2 is often between the ages of 50 and 70, although it can occur in younger individuals. Prevalence data shows that the condition affects a portion of the aging population, though specific figures vary depending on the population studied. Factors like genetics and environmental influences play a role in the development of MT2.
Risk Factors
Several factors may increase the risk of developing MT2. These include a family history of the condition, as well as certain genetic predispositions. Exposure to certain environmental factors, such as smoking and prolonged sun exposure, may also play a role. Moreover, individuals with a history of certain medical conditions, such as diabetes or high blood pressure, may be at a higher risk.
Impact on Daily Activities and Quality of Life
MT2 can significantly impact daily activities and quality of life. Difficulties with reading, driving, recognizing faces, and performing other tasks requiring sharp central vision are common. The gradual progression of vision loss can lead to frustration, anxiety, and depression. It is crucial for individuals with MT2 to seek support and adapt to their changing vision needs to maintain a positive quality of life.
Summary of Key Features
| Feature | Description |
|---|---|
| Definition | Abnormal dilation and widening of small blood vessels in the macula. |
| Visual Features | Gradual blurring, distortion, loss of central vision; metamorphopsia, scotomas. |
| Age of Onset | Typically between 50 and 70 years, although can occur in younger individuals. |
| Prevalence | Affects a portion of the aging population, figures vary. |
| Risk Factors | Family history, genetic predisposition, environmental factors (smoking, sun exposure), medical conditions (diabetes, high blood pressure). |
| Impact on Daily Life | Difficulties with reading, driving, recognizing faces, and other tasks requiring sharp central vision; potential for frustration, anxiety, depression. |
Pathophysiology and Underlying Mechanisms
Macular telangiectasia type 2 (MT2) is a complex retinal disorder characterized by abnormal blood vessel growth in the macula, the central part of the retina responsible for sharp, central vision. Understanding the pathophysiological mechanisms behind MT2 is crucial for developing effective treatment strategies and improving the lives of affected individuals. This exploration delves into the known mechanisms driving MT2, highlighting the role of vascular abnormalities, cellular and molecular processes, and comparisons with other macular diseases.The development of MT2 is a multi-faceted process involving intricate interactions between genetic predisposition, environmental factors, and the delicate balance within the retina.
Vascular abnormalities play a pivotal role in the progression of MT2, often leading to the characteristic dilated and tortuous blood vessels that are a hallmark of the disease. Understanding the cellular and molecular processes involved in this abnormal vessel formation is vital for developing therapies that target these processes.
Vascular Abnormalities in MT2
The hallmark of MT2 is the presence of abnormal, dilated blood vessels in the macula. These vascular abnormalities are not simply a passive consequence of the disease; rather, they are actively involved in the disease’s progression. The underlying mechanisms driving these vascular changes are complex and not fully understood. However, research suggests that an imbalance in growth factors and signaling pathways, such as vascular endothelial growth factor (VEGF) and its receptors, may contribute significantly to the aberrant blood vessel growth.
The dysregulation of these pathways likely leads to increased permeability and fragility of the vessels, potentially causing leakage of fluid and blood components.
Cellular and Molecular Processes in MT2
The cellular and molecular processes contributing to MT2 are not fully elucidated, but some key aspects are emerging. For example, the involvement of inflammatory cells, such as macrophages and T cells, in the pathogenesis of MT2 is gaining attention. The precise mechanisms by which these cells contribute to the disease are not yet clear, but their presence suggests a role for inflammation in the progression of the disorder.
Moreover, alterations in the extracellular matrix, the structural support network of the retina, may also contribute to the development and progression of MT2. These changes can disrupt the delicate balance within the retina, potentially impacting the structural integrity and function of the macula.
Comparison with Other Macular Diseases
Comparing the pathophysiology of MT2 with other macular diseases, such as age-related macular degeneration (AMD), provides valuable insights. While both diseases affect the macula, the underlying mechanisms differ significantly. AMD, for instance, is primarily characterized by the accumulation of drusen, deposits under the retina, and subsequent retinal pigment epithelium (RPE) damage. In contrast, MT2 is characterized by abnormal blood vessel formation and related complications.
Further research is necessary to fully understand the nuanced differences and overlaps between these conditions.
Stages of MT2 Development
| Stage | Description | Visual Features |
|---|---|---|
| Early | Initial development of small, subtle vascular changes in the macula. | Mild blurring or distortion of central vision; possible asymptomatic phase. |
| Intermediate | Increased dilation and tortuosity of the vessels, potentially with mild leakage. | Progressive blurring and distortion of central vision; possible reduction in visual acuity. |
| Late | Significant dilation and tortuosity of the vessels; increased leakage and potential scarring. | Severe blurring and distortion of central vision; significant reduction in visual acuity; potential for vision loss. |
Diagnosis and Evaluation
Diagnosing macular telangiectasia type 2 (MT2) relies on a combination of clinical examination and specialized imaging techniques. Accurate diagnosis is crucial for appropriate management and to distinguish MT2 from other macular conditions with similar presentations. Early detection and intervention can potentially slow disease progression and preserve vision.Ophthalmic examinations and imaging play a critical role in identifying the characteristic vascular changes associated with MT2.
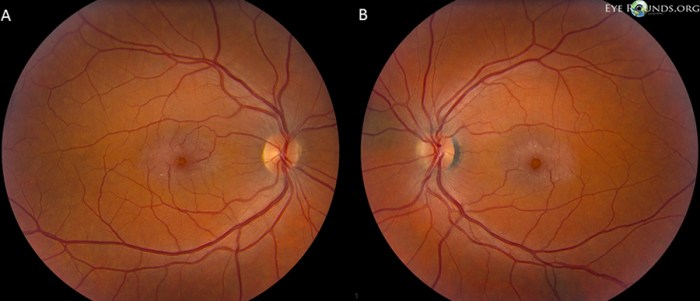
A detailed eye examination, including visual acuity testing, slit-lamp biomicroscopy, and fundus examination, is essential to assess the overall health of the retina and identify any abnormalities.
Common Diagnostic Methods for MT2, Macular telangiectasia type two
Comprehensive ophthalmic examinations are fundamental in identifying MT2. These evaluations encompass various procedures to meticulously assess the eye’s structure and function. Visual acuity testing determines the clarity of vision, providing an initial measure of potential visual impairment. Slit-lamp biomicroscopy allows for a detailed inspection of the anterior segment of the eye, including the cornea, lens, and anterior chamber, which, while not directly related to MT2, helps rule out other conditions.
The fundus examination, a crucial component of the eye exam, enables visualization of the retina, choroid, and optic nerve. During the fundus examination, characteristic findings in MT2, such as dilated, tortuous vessels in the macula, can be observed.
Role of Ophthalmic Examinations in Detecting MT2
Ophthalmic examinations are crucial for detecting the characteristic signs of MT2. Visual acuity testing, although not specific to MT2, serves as an initial indicator of visual function and potential impairment. The slit-lamp biomicroscopy allows for evaluation of the anterior segment of the eye, enabling the ophthalmologist to assess the general health of the eye and rule out other anterior segment pathologies.
The fundus examination is particularly important for MT2 detection, as it allows direct visualization of the retina and the presence of characteristic dilated and tortuous vessels within the macula.
Importance of Imaging Techniques in Diagnosing MT2
Specialized imaging techniques play a critical role in confirming the diagnosis of MT2 and evaluating its extent. These techniques provide detailed images of the retina, revealing subtle vascular changes that might not be apparent during a standard ophthalmic examination. Furthermore, they can aid in monitoring disease progression and assessing the effectiveness of treatment.
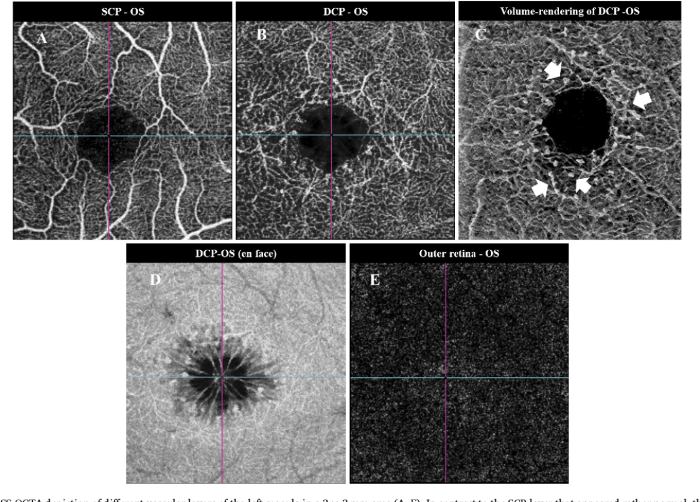
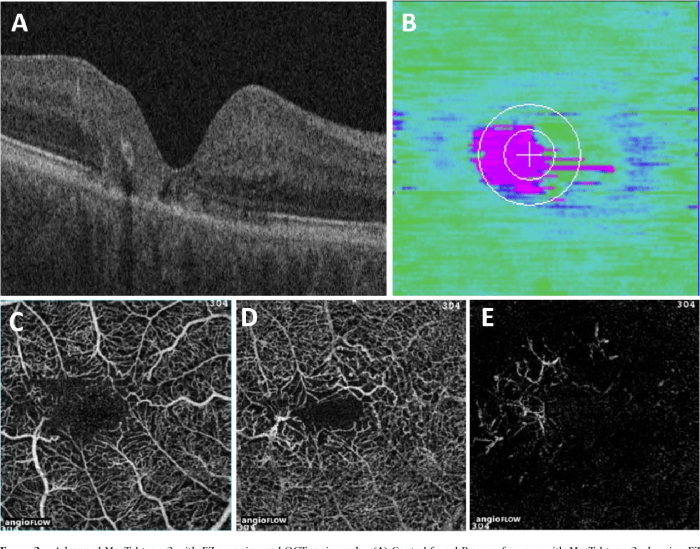
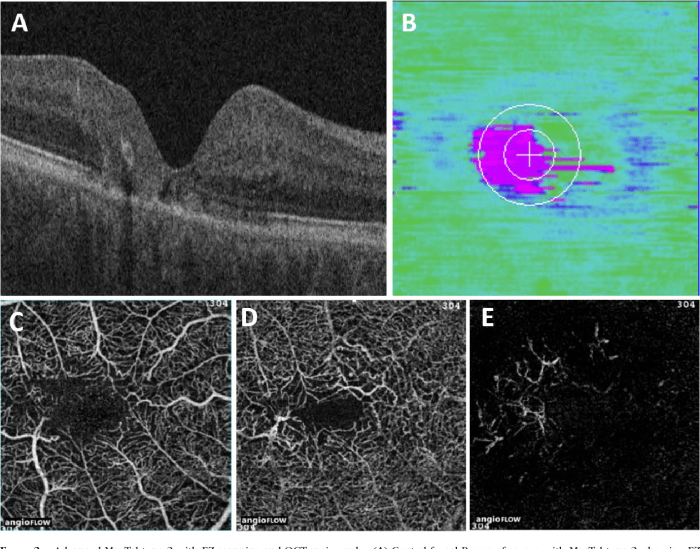
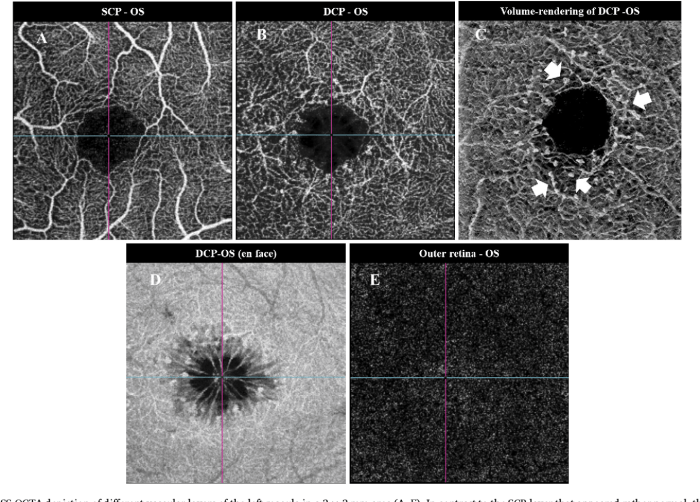
Use of Fluorescein Angiography and Optical Coherence Tomography in the Diagnosis of MT2
Fluorescein angiography (FA) and optical coherence tomography (OCT) are two key imaging techniques used in the diagnosis of MT2. FA, using a fluorescent dye, visualizes the retinal and choroidal vasculature, highlighting the dilated, tortuous vessels and leakage characteristic of MT2. OCT, a non-invasive technique, provides high-resolution cross-sectional images of the retina, allowing for detailed evaluation of retinal thickness and the presence of any macular edema or other structural changes associated with MT2.
Diagnostic Tests and Their Findings in MT2
| Test | Findings in MT2 |
|---|---|
| Visual Acuity | Potential reduction in central vision, often variable. |
| Slit-lamp Biomicroscopy | Normal findings, unless co-existing anterior segment pathology is present. |
| Fundus Examination | Dilated, tortuous, and sometimes hemorrhagic vessels within the macula. |
| Fluorescein Angiography (FA) | Demonstrates leakage and increased permeability of vessels in the macula, often appearing as areas of pooling dye. |
| Optical Coherence Tomography (OCT) | May reveal macular edema or thinning of the retinal layers, particularly in the areas of telangiectasia. Changes in retinal nerve fiber layer (RNFL) thickness may also be present. |
Management and Treatment Strategies
Unfortunately, there’s no cure for macular telangiectasia type 2 (MT2). Current management focuses on slowing disease progression and preserving vision. This involves a multifaceted approach combining medical interventions, supportive care, and lifestyle adjustments. The goal is to minimize the impact of the disease on daily life and maintain the best possible visual function.Preserving vision in MT2 is a complex undertaking, necessitating a personalized approach tailored to the individual patient’s unique characteristics and the stage of disease progression.
Treatment strategies aim to reduce the growth of abnormal blood vessels, prevent further damage to the macula, and maintain existing visual acuity.
Available Treatment Options for MT2
Current treatment options for MT2 primarily focus on slowing the progression of the disease rather than reversing it. The most commonly used treatment approaches are aimed at reducing the inflammation and vascular leakage associated with the condition. These include anti-VEGF therapies and other targeted interventions. Each approach has its own advantages and limitations, making personalized decisions crucial.
Role of Supportive Care in Managing MT2
Supportive care plays a vital role in managing MT2, complementing medical interventions. This includes comprehensive eye care, regular monitoring, and lifestyle adjustments to mitigate risk factors and maintain overall health. Eye exams are essential to track disease progression and adjust treatment plans accordingly. Proper nutrition, regular exercise, and stress management are also crucial for overall well-being and may indirectly influence disease progression.
A holistic approach that integrates medical interventions with supportive care is vital for optimizing outcomes.
Rationale Behind Different Treatment Approaches
The rationale behind different treatment approaches for MT2 stems from understanding the underlying pathophysiology. The abnormal blood vessels in MT2 contribute to inflammation and leakage, leading to macular damage. Treatments like anti-VEGF therapies aim to reduce this leakage and inflammation. The efficacy of different treatments can vary depending on the individual’s response to the therapy and the stage of the disease.
Potential Efficacy of Different Treatments in Slowing Disease Progression
Studies have shown that anti-VEGF therapies, in some cases, can slow the progression of MT2. The effectiveness of these treatments, however, varies greatly between individuals. Factors such as the stage of the disease, the extent of macular involvement, and the individual’s response to treatment all contribute to the outcome. Regular monitoring and adjustments to treatment plans are necessary to optimize the benefits.
Comparison of Treatment Options
| Treatment | Effectiveness | Side Effects |
|---|---|---|
| Anti-VEGF Therapy (e.g., ranibizumab, aflibercept) | Potentially slows progression, improves visual acuity in some cases. | Potential for retinal detachment, intraocular pressure changes, and eye infections. Individual responses vary. |
| Laser Photocoagulation | May reduce leakage and inflammation in certain areas, but less effective overall. | Potential for retinal scarring and further vision loss if not performed appropriately. |
| Supportive Care (nutrition, exercise, stress management) | While not a direct treatment, may contribute to overall health and potentially slow progression by reducing risk factors. | No direct side effects related to the care itself, but adherence to a healthy lifestyle may be challenging. |
Visual Outcomes and Prognosis
Macular telangiectasia type 2 (MT2) is a progressive disease that significantly impacts vision. Understanding the typical visual outcomes, the factors influencing prognosis, and strategies for managing visual decline is crucial for patients and healthcare providers. This section will delve into the complexities of visual prognosis in MT2, providing insights into the long-term impact and the role of regular monitoring.Visual outcomes in MT2 are characterized by a gradual decline in central vision.
The severity of this decline varies greatly among individuals, influenced by a number of factors. This variability underscores the importance of personalized management strategies tailored to each patient’s specific condition.
Typical Visual Outcomes
The hallmark of MT2 is the progressive development of abnormal blood vessels in the macula, the central part of the retina responsible for sharp, detailed vision. This vascular abnormality leads to a gradual loss of central vision, often described as blurry or distorted central vision. Patients may experience difficulty with tasks requiring fine detail, such as reading, driving, and recognizing faces.
The rate of visual decline is not uniform; some individuals experience a rapid deterioration, while others have a slower progression.
Factors Influencing Visual Prognosis
Several factors play a role in predicting the visual outcome of MT2. Age at diagnosis, the extent of macular involvement, the presence of other eye conditions, and the individual’s overall health all contribute to the variability in visual prognosis. For example, an earlier diagnosis often allows for more proactive management and potentially slows the rate of visual decline.
Furthermore, individuals with a family history of macular degeneration may experience a more rapid decline. The severity of the telangiectasia and its progression are also key factors.
Long-Term Impact on Vision
The long-term impact of MT2 on vision can be substantial. The progressive nature of the disease means that patients may experience significant visual impairment over time, impacting their quality of life. This can affect daily activities such as reading, driving, and recognizing faces. Adjustments to daily routines, assistive technologies, and support systems are often necessary to maintain independence and well-being.
Macular telangiectasia type two can be a tricky condition, often causing vision changes. It’s frequently linked to other eye issues, and interestingly, research suggests a possible connection between this condition and dry eye, which can sometimes be a symptom in those experiencing migraines. For more on the potential relationship between dry eye and migraine, check out this helpful resource: dry eye and migraine.
Ultimately, understanding these potential connections is crucial for anyone dealing with macular telangiectasia type two.
For example, a patient diagnosed at a younger age may need to adapt more extensively to visual impairment compared to someone diagnosed later in life.
Macular telangiectasia type two can be a tricky condition to manage, often requiring various diagnostic tests. One such test is an MRI, which helps doctors get a clearer picture of the eye’s structure. To help you understand what to expect in an MRI procedure, I recommend checking out this helpful guide: what to expect in an mri.
Ultimately, these insights can provide a better overall understanding of your condition and its potential impact on your vision.
Managing Visual Deterioration
Effective management of visual deterioration in MT2 is multifaceted. Treatment strategies focus on slowing the progression of the disease, maintaining existing vision, and mitigating the impact on daily life. Strategies include regular monitoring, appropriate pharmacologic interventions, and lifestyle adjustments. For instance, some patients may benefit from vision rehabilitation therapies to help adapt to their changing vision.
Macular telangiectasia type two, a condition affecting the retina, can sometimes cause bleeding. If you’re noticing bright red blood in your stool, it’s crucial to seek medical advice right away. This could be a sign of a more serious issue, so it’s always best to check with a doctor. For more information on interpreting bright red blood in stool, you can refer to this helpful guide: advice about bright red blood in stool.
While rare, bleeding can be a symptom of macular telangiectasia type two, so don’t hesitate to consult your eye doctor if you have concerns.
Role of Regular Monitoring
Regular monitoring is critical in predicting and managing visual decline in MT2. Comprehensive ophthalmological examinations, including visual acuity testing, fundus photography, and optical coherence tomography (OCT), are essential for tracking the progression of the disease. These tests allow healthcare providers to assess the extent of macular changes and adjust treatment strategies as needed. This proactive approach helps to maintain the best possible visual function.
For example, a patient with a slow decline might require less frequent monitoring compared to someone with a rapid progression.
Comparison of Visual Acuity Outcomes
| Treatment | Visual Acuity Outcome |
|---|---|
| Anti-VEGF injections | Often shows stabilization or slight improvement in visual acuity, particularly in the early stages of the disease. Individual responses vary. |
| Laser photocoagulation | Limited efficacy in slowing the progression of MT2, although it may be used to treat secondary complications or to minimize further damage. Outcomes depend on the extent of macular involvement and individual response. |
| No intervention | Progressive visual loss is expected without intervention. The rate of progression varies significantly. |
Note: Visual acuity outcomes are influenced by a multitude of factors and should be considered in the context of the individual patient’s specific condition.
Research and Future Directions
Unraveling the complexities of Macular Telangiectasia Type 2 (MT2) requires ongoing research efforts. Current research is actively exploring various aspects of the disease, from its underlying mechanisms to potential therapeutic interventions. This exploration promises to shed light on the progression of MT2 and lead to more effective treatments.
Current Research Efforts
Researchers are actively investigating the genetic and environmental factors contributing to MT2. Studies are examining the role of specific genes in the development and progression of the disease, potentially identifying biomarkers for early detection. Moreover, research is focusing on the vascular abnormalities characteristic of MT2, aiming to understand the precise mechanisms driving the formation and progression of the telangiectatic vessels.
Animal models are also being utilized to study the disease’s progression in vivo, offering valuable insights into potential therapeutic targets.
Gaps in Current Knowledge
Despite significant advancements, crucial gaps remain in our understanding of MT2. Precisely defining the interplay between genetic predisposition and environmental triggers in MT2 pathogenesis remains a significant challenge. The lack of effective biomarkers for early detection and disease progression monitoring hinders timely intervention and treatment optimization. Further research is also needed to clarify the specific cellular and molecular pathways involved in the development and progression of the telangiectasia.
Moreover, understanding the impact of various risk factors, including lifestyle and environmental exposures, on the disease’s course is still limited.
Potential Future Research Directions
Future research should focus on developing more effective diagnostic tools. This includes identifying novel biomarkers that can detect MT2 at its earliest stages, enabling timely intervention and potentially slowing disease progression. Furthermore, research should explore the potential of novel therapeutic strategies targeting the underlying mechanisms of MT2. This could include therapies that aim to stabilize or regress the telangiectatic vessels, thus preserving vision.
A strong emphasis on developing personalized treatment approaches, based on individual genetic profiles and disease characteristics, is essential.
Table of Key Research Areas and Objectives
| Research Area | Objective |
|---|---|
| Genetic and Environmental Risk Factors | Identify specific genes and environmental factors associated with MT2 development and progression. Determine the interaction between genetic predisposition and environmental triggers to understand the pathogenesis of MT2. |
| Early Detection Biomarkers | Develop novel biomarkers for early detection of MT2, enabling timely intervention and potentially slowing disease progression. |
| Therapeutic Strategies | Explore and develop novel therapeutic strategies targeting the underlying mechanisms of MT2, focusing on stabilizing or regressing telangiectatic vessels. Investigate the effectiveness of existing treatments in different genetic subtypes of MT2. |
| Personalized Treatment Approaches | Develop personalized treatment strategies tailored to individual genetic profiles and disease characteristics. |
Patient Education and Support
Understanding macular telangiectasia type 2 (MT2) can be overwhelming for patients and their families. Accurate information and supportive resources are crucial for navigating the challenges of this condition. Empowering patients with knowledge and connecting them with a supportive community can significantly improve their overall well-being and quality of life.Patient education is essential for effectively managing MT2. It equips patients with the knowledge needed to make informed decisions about their treatment and lifestyle choices.
This empowers them to actively participate in their eye care, leading to better outcomes and a greater sense of control over their condition. Understanding the progression of the disease, potential complications, and available treatment options allows patients to develop realistic expectations and proactive strategies for managing their vision loss.
Resources Available to Support Patients with MT2
Numerous resources are available to provide comprehensive support and education for patients with MT2. These resources can help individuals understand the condition, access appropriate medical care, and connect with others facing similar challenges. This comprehensive approach is critical for improving patient outcomes and well-being.
- Medical Professionals: Ophthalmologists specializing in macular diseases are crucial resources. They provide expert diagnoses, treatment plans, and ongoing monitoring. Regular communication with these professionals allows for proactive management of the condition and adaptation of treatment strategies as needed.
- Support Groups: Connecting with other patients with MT2 can offer invaluable emotional support and practical advice. Support groups provide a safe space for sharing experiences, coping mechanisms, and practical strategies for managing the condition’s challenges.
- Educational Programs: Organizations dedicated to eye health often provide educational programs and workshops for patients with MT2. These programs typically cover the basics of the disease, management techniques, and available resources.
- Online Forums and Communities: Online platforms can offer a convenient way for patients to connect with others, share experiences, and access information. However, it’s important for patients to verify the reliability and accuracy of information found online.
Support Groups and Educational Programs for MT2
Support groups offer a crucial network of individuals who understand the unique challenges associated with MT2. These groups provide a safe and supportive environment for sharing experiences, coping mechanisms, and advice. They foster a sense of community and belonging, reducing feelings of isolation and promoting emotional well-being.Educational programs, often offered by ophthalmology practices or eye health organizations, are invaluable for patients and their families.
These programs cover essential topics such as disease progression, treatment options, and lifestyle adjustments to manage the condition effectively.
Patient Resources and Support Organizations
| Resource | Description |
|---|---|
| American Academy of Ophthalmology | Provides comprehensive information on various eye conditions, including MT2. Their website often features educational materials and links to other relevant resources. |
| National Eye Institute (NEI) | A branch of the National Institutes of Health, the NEI funds research and provides information on eye health issues, including MT2. They frequently publish updates on the latest research and treatment developments. |
| Local Ophthalmologists | Consult local ophthalmologists for specialized care and information regarding MT2. They can offer personalized recommendations and treatment strategies. |
| Patient Advocacy Groups (if available locally) | Specific patient advocacy groups may focus on MT2 or related macular conditions. These groups may organize meetings, support groups, and educational events. |
Closing Notes
In conclusion, macular telangiectasia type two is a multifaceted condition requiring a multi-pronged approach to management. From early detection and diagnosis to the latest treatment options and ongoing research, this guide aims to provide a comprehensive resource for understanding and navigating the complexities of MT2. The key takeaways include the importance of regular monitoring, the available treatment options, and the crucial role of patient education and support in managing this condition effectively.
This guide hopes to empower individuals affected by MT2 and their loved ones with the knowledge they need to make informed decisions about their care.