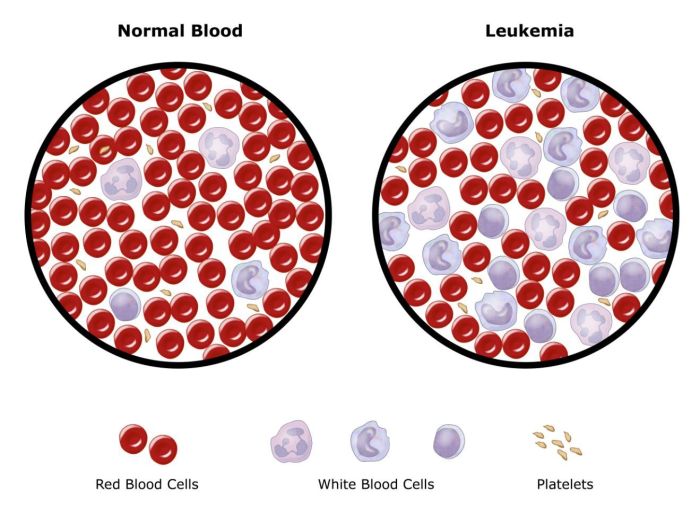
Mixed cellularity hodgkins lymphoma – Mixed cellularity Hodgkin lymphoma (MCHL) is a type of blood cancer that requires careful understanding. It’s characterized by the presence of specific abnormal cells, called Reed-Sternberg cells, and other unique histological features. Diagnosing and treating MCHL involves a multifaceted approach, encompassing various diagnostic procedures, treatment strategies, and considerations of prognosis and potential complications. This in-depth look delves into the intricacies of MCHL, from its defining characteristics to its management and future research directions.
This exploration of MCHL will cover its defining characteristics, including the key histological features that distinguish it from other Hodgkin lymphoma subtypes. We’ll examine the clinical presentation, common symptoms, and typical staging classifications. Further, we’ll discuss the epidemiology, risk factors, and the diagnostic methods, including the crucial role of lymph node biopsies and immunohistochemistry. Treatment strategies, including chemotherapy and radiation therapy, will be analyzed.
The discussion will also cover prognosis, potential complications, and the latest research in MCHL.
Defining Mixed Cellularity Hodgkin Lymphoma
Mixed Cellularity Hodgkin Lymphoma (MCHL) is a subtype of Hodgkin lymphoma, a cancer of the lymphatic system. Understanding its unique characteristics is crucial for accurate diagnosis and effective treatment. It’s important to differentiate MCHL from other Hodgkin lymphoma subtypes due to varying prognoses and treatment approaches. This blog post delves into the key features of MCHL, providing a comprehensive overview of its definition, histological attributes, clinical presentation, and staging.MCHL is characterized by a specific blend of reactive and malignant cells within the affected lymph nodes.
The histological appearance distinguishes it from other types of Hodgkin lymphoma. The presence of these specific cell types, and their proportions, aids in diagnosis. This distinctive cellular mix is crucial for diagnosis, differentiating it from other lymphoma subtypes. The clinical presentation can range from subtle to more pronounced symptoms, requiring careful evaluation by healthcare professionals.
Histological Features
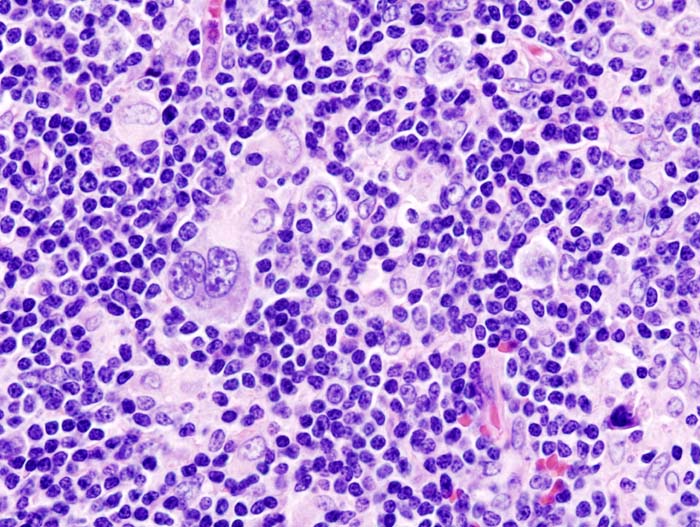
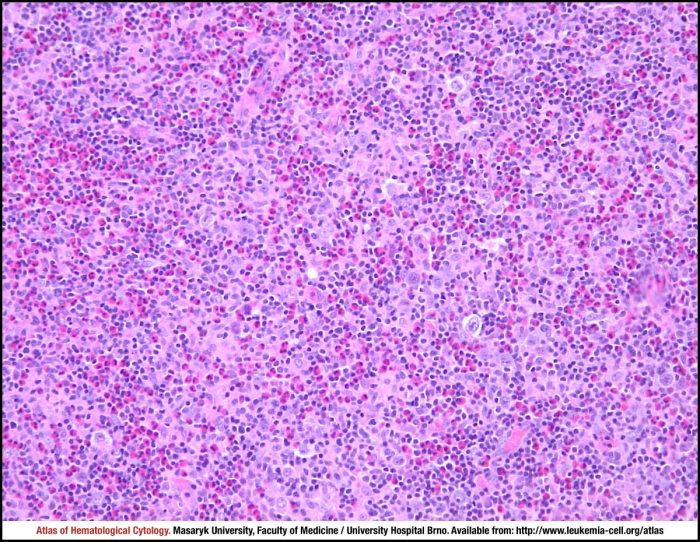
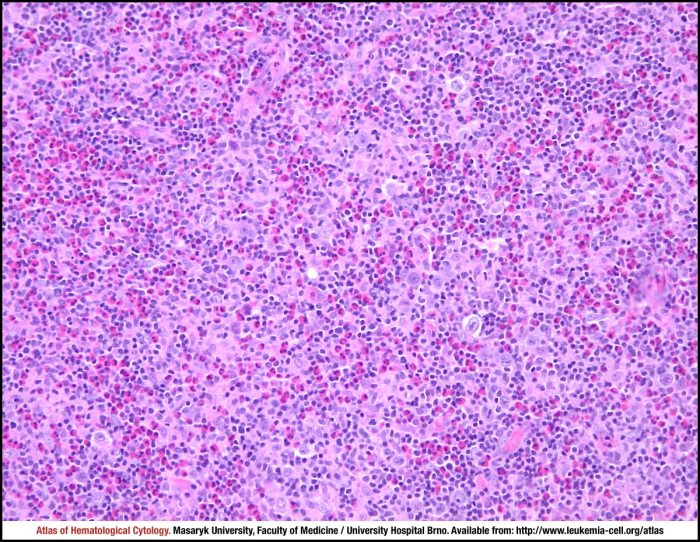
The defining feature of MCHL lies in its unique histological composition. It’s characterized by a mixture of reactive lymphocytes, often including significant numbers of eosinophils and plasma cells, along with Hodgkin and Reed-Sternberg cells. The proportion of these cells varies from case to case. The presence of significant numbers of these cells is critical for diagnosis. The specific ratios of different cell types contribute to the final diagnosis.
The histological examination plays a crucial role in identifying MCHL.
Cell Types
The mixed cellularity in MCHL is the hallmark of this subtype. The typical cell types found within the lymph node architecture include Hodgkin and Reed-Sternberg cells, but also a significant number of reactive lymphocytes, often with a prominent presence of eosinophils. The presence of plasma cells is also a key characteristic. The proportion of each cell type is a crucial element in distinguishing MCHL from other subtypes.
The presence of eosinophils is notable and is often present in greater numbers than in other subtypes. Plasma cells are also a characteristic feature.
Clinical Presentation
MCHL can present with a range of symptoms and signs, often reflecting the involvement of lymph nodes. Common symptoms include painless lymphadenopathy, which is often the initial manifestation. Patients may also experience fever, night sweats, and weight loss, though these are not always present. Splenomegaly and hepatomegaly may be present, particularly in advanced stages. Symptoms are generally less severe than in other types of Hodgkin lymphoma.
In some cases, the presentation may be subtle, making early detection challenging. This requires thorough physical examination and appropriate investigations.
Staging Classifications
Staging is a crucial aspect of managing MCHL. The Ann Arbor staging system, a widely used approach, classifies the extent of disease based on the involved lymph nodes and the presence of extranodal involvement. This system provides a framework for treatment planning and prognosis. The specific stage influences the treatment strategy. The stages are determined by factors such as the number of lymph node regions involved, the presence of extranodal disease, and the extent of systemic involvement.
Staging is critical for developing a personalized treatment plan. The specific stage influences the treatment strategy.
Mixed cellularity Hodgkin lymphoma, a type of blood cancer, can present with a range of symptoms. While often associated with physical challenges, it’s important to remember that the psychological toll can also be significant. This can sometimes manifest as social anxieties, impacting communication and daily life. In some cases, these anxieties can lead to selective mutism in adults, a condition where individuals have difficulty speaking in certain social situations.
Ultimately, understanding these potential connections is crucial for comprehensive care and support for those facing mixed cellularity Hodgkin lymphoma.
Epidemiology and Risk Factors
Mixed Cellularity Hodgkin Lymphoma (MCHL) is a type of Hodgkin lymphoma characterized by a mixed cellular infiltrate. Understanding its prevalence, potential risk factors, and demographic distribution is crucial for early detection and improved patient outcomes. This knowledge guides preventive measures and targeted research efforts.MCHL, like other cancers, exhibits variability in its global distribution and incidence rates. Factors such as genetic predisposition, environmental exposures, and lifestyle choices play a role in its development.
While a definitive cause remains elusive, exploring these potential contributors offers insights into risk mitigation and potential avenues for future prevention strategies.
Global Incidence and Prevalence
The global incidence and prevalence of MCHL vary significantly across different regions and populations. Precise figures are often challenging to obtain due to variations in diagnostic criteria and reporting standards. However, available data suggest a relatively low incidence rate compared to other types of lymphoma. This variability underscores the complexity of MCHL’s etiology and the need for further research to clarify these differences.
Potential Risk Factors
Numerous factors are hypothesized to increase the risk of developing MCHL. These include genetic susceptibility, certain infections, and environmental exposures. While definitive causal links are still being established, these potential risk factors offer avenues for future research and potential preventative measures.
Age of Onset and Gender Distribution
MCHL typically presents in adulthood, with a peak incidence in the 20s and 30s, followed by another smaller peak in the 50s and 60s. However, MCHL can affect individuals at any age. Gender-wise, there appears to be a slight male predominance, but the difference isn’t consistently significant across studies. These patterns warrant further investigation to better understand the factors contributing to these variations.
Genetic and Environmental Factors
Genetic factors likely play a role in MCHL development, although the specific genes involved remain largely unknown. Studies suggest a possible link between certain genetic mutations and increased susceptibility to the disease. Environmental exposures, including exposure to certain chemicals or infections, are also suspected to influence the risk of MCHL, though more research is needed to establish concrete correlations.
Environmental risk factors often interact with genetic predispositions, making a definitive link challenging to establish.
Diagnostic Methods and Procedures
Diagnosing Mixed Cellularity Hodgkin Lymphoma (MCHL) involves a multi-step process, starting with a thorough evaluation of symptoms and medical history. This is followed by a series of diagnostic tests, ultimately culminating in a definitive diagnosis based on the microscopic examination of tissue samples. Careful consideration of the results of these tests, combined with clinical findings, helps physicians to determine the appropriate treatment plan.
Lymph Node Biopsy
A lymph node biopsy is the cornerstone of diagnosing MCHL. This procedure involves removing a small sample of the affected lymph node for microscopic examination. The biopsy allows pathologists to observe the cellular architecture and identify the presence of Reed-Sternberg cells and other characteristic cells. The pathologist will also evaluate the degree of cellularity and the specific types of inflammatory cells present.
Mixed cellularity Hodgkin lymphoma can be a tough battle, but staying active is key. Building strength, especially in your legs, can really help with overall well-being, and I’ve found some fantastic exercises for that. Check out my favorite leg strengthening exercises for some ideas to incorporate into your routine. favorite leg strengthening exercises These exercises can help boost energy levels and overall stamina, which can be really helpful in managing the physical demands of treating mixed cellularity Hodgkin lymphoma.
This detailed assessment is crucial in differentiating MCHL from other lymphomas and related conditions. The procedure involves local anesthesia and usually involves a small incision.
Immunohistochemistry and Flow Cytometry
Immunohistochemistry (IHC) and flow cytometry are crucial supplementary techniques in the diagnostic process. IHC uses antibodies to identify specific proteins within the cells. This helps to confirm the presence of Reed-Sternberg cells and to further characterize the specific cell types involved. Flow cytometry analyzes the physical and chemical properties of cells, including their surface markers. This technique helps to distinguish MCHL from other lymphomas with similar appearances and further classify the subtypes of MCHL.
These techniques help confirm the diagnosis and aid in understanding the disease’s specific features.
Bone Marrow Biopsy
A bone marrow biopsy is often performed to assess the extent of the disease and to evaluate the involvement of bone marrow. This procedure involves extracting a small sample of bone marrow from the hip bone. The sample is examined under a microscope to determine the presence of lymphoma cells. The significance of this test in MCHL lies in determining if the disease has spread beyond the lymph nodes to other parts of the body.
This helps in staging the disease and guides treatment strategies.
Key Diagnostic Tests and Expected Results in MCHL
| Test | Expected Result in MCHL | Explanation |
|---|---|---|
| Lymph Node Biopsy | Presence of Reed-Sternberg cells and other characteristic cells, along with a mixed cellular infiltrate. | The microscopic examination reveals a diverse array of immune cells alongside the Reed-Sternberg cells, characteristic of MCHL. |
| Immunohistochemistry (IHC) | Positive staining for specific markers like CD15 and CD30 on Reed-Sternberg cells. | IHC confirms the presence of Reed-Sternberg cells and helps distinguish MCHL from other lymphomas. |
| Flow Cytometry | Presence of a mixed population of lymphocytes and other immune cells. | This method analyzes the physical and chemical properties of cells, identifying specific markers on the cells’ surface. |
| Bone Marrow Biopsy | May show infiltration of lymphoma cells if the disease has spread. | Absence of lymphoma cells suggests the disease is localized to lymph nodes. |
Treatment Strategies
Mixed Cellularity Hodgkin Lymphoma (MCHL) treatment aims to eradicate the cancerous cells while minimizing harm to healthy tissues. The choice of treatment often depends on the stage of the lymphoma, the patient’s overall health, and individual factors. A multidisciplinary approach, involving oncologists, radiation oncologists, and other healthcare professionals, is crucial for optimal outcomes.
Standard Treatment Approaches for MCHL
The standard treatment for MCHL usually involves a combination of chemotherapy, radiation therapy, and sometimes stem cell transplantation. The specific approach is tailored to the individual patient. Early-stage MCHL might be effectively treated with radiation therapy alone, while more advanced cases often necessitate chemotherapy regimens in addition to radiation. The goal is to achieve remission and prevent recurrence.
Role of Chemotherapy Regimens in MCHL
Chemotherapy plays a significant role in MCHL treatment, targeting rapidly dividing cells, including the cancerous Hodgkin and Reed-Sternberg cells. Various chemotherapy regimens are employed, often incorporating multiple drugs with different mechanisms of action. These regimens are designed to maximize the effectiveness of the treatment while minimizing side effects. Examples include ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) and BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone).
Mixed cellularity Hodgkin lymphoma (MCHL) can be a tricky beast to diagnose, requiring careful analysis of lymph node biopsies. Similar to how diagnosing her2 positive breast cancer often involves specific genetic testing, like diagnosis and testing for her2 positive breast cancer , the process for MCHL involves a range of tests to pinpoint the exact type and stage of the lymphoma.
Ultimately, accurate diagnosis is crucial for developing an effective treatment plan for MCHL.
The specific regimen chosen depends on the individual patient’s characteristics.
Use of Radiation Therapy in MCHL Treatment
Radiation therapy is frequently used in MCHL treatment, particularly for localized disease. High-energy radiation beams are directed at the affected area, destroying the cancer cells. External beam radiation therapy is a common approach. The dosage and the extent of the irradiated area are carefully determined based on the tumor’s location and size. In some cases, brachytherapy (placing radioactive material directly into the tumor) might also be employed.
Comparison of Efficacy of Different Treatment Options for MCHL
The efficacy of various treatment options for MCHL is evaluated based on factors such as remission rates, long-term survival, and side effects. While chemotherapy regimens have shown efficacy in controlling the disease and achieving remission, radiation therapy often proves effective in localized MCHL. The combination of chemotherapy and radiation therapy is often the most effective approach for more advanced or widespread disease.
Summary Table Comparing Various Treatment Options for MCHL
| Treatment | Mechanism | Advantages | Disadvantages |
|---|---|---|---|
| Chemotherapy (e.g., ABVD, BEACOPP) | Targeting rapidly dividing cells, including cancerous cells | Effective in controlling the disease, particularly in advanced or disseminated MCHL; potentially curative | Potential for side effects, including nausea, hair loss, fatigue, and damage to other healthy tissues; risk of secondary cancers |
| Radiation Therapy | High-energy radiation beams destroy cancer cells in localized areas | Effective in localized disease, often used as a primary or adjuvant treatment | Potential for side effects depending on the area irradiated; less effective for disseminated disease |
| Stem Cell Transplantation | Replacing damaged bone marrow with healthy stem cells | Potentially curative in high-risk cases | High risk of complications, including infections and graft-versus-host disease; intensive and prolonged recovery period |
Prognosis and Outcomes
Mixed cellularity Hodgkin lymphoma (MCHL) prognosis is complex and depends on various factors. While advancements in treatment have significantly improved outcomes, understanding the nuances of long-term survival is crucial for both patients and healthcare providers. Individual responses to treatment vary, and factors like the extent of disease, patient age, and overall health play a vital role in determining the long-term outlook.Understanding the factors that influence prognosis allows for more personalized treatment strategies and realistic expectations.
Early detection and aggressive, well-timed treatment are key to improving outcomes. The overall survival rates are influenced by these factors and often vary depending on the specific treatment approach.
Long-Term Prognosis Overview, Mixed cellularity hodgkins lymphoma
The long-term prognosis for patients with MCHL has significantly improved with advancements in treatment. While not a cure-all, modern therapies have dramatically increased the chances of long-term survival and remission. However, it’s important to note that individual experiences and responses to treatment can differ considerably.
Factors Influencing Prognosis
Several factors influence the prognosis of MCHL. These factors often need to be considered in a holistic manner, as no single factor dictates the overall outcome.
- Stage of the disease at diagnosis:
- Patient age and overall health:
- Response to initial treatment:
- Treatment approach and intensity:
- Presence of specific risk factors:
The extent of the disease’s spread significantly impacts the prognosis. Early-stage MCHL, where the lymphoma is localized, generally has a better prognosis than advanced-stage disease, which has spread to other parts of the body.
Younger patients with fewer underlying health conditions often have better outcomes. The presence of other medical conditions or older age may impact the body’s ability to respond to treatment.
How a patient responds to the initial treatment regimen significantly influences the long-term outlook. A complete response or a partial response to treatment generally correlates with a more favorable prognosis.
The chosen treatment strategy, its intensity, and adherence to the treatment plan all contribute to the success rate and ultimate outcome.
Certain risk factors, such as the presence of specific genetic markers, may impact the prognosis. These factors are often considered in developing a personalized treatment plan.
Role of Early Diagnosis and Treatment
Early diagnosis and prompt treatment are crucial in improving outcomes for MCHL. Early intervention allows for treatment to be initiated before the disease has advanced, increasing the likelihood of a successful outcome. Early detection often leads to a more favorable response to treatment and a higher chance of achieving long-term remission.
Survival Rates
Survival rates for MCHL are influenced by the factors mentioned above and vary based on the time period following diagnosis. It is essential to interpret these figures in the context of the entire patient’s medical history.
| Time Period | 5-Year Survival Rate | 10-Year Survival Rate |
|---|---|---|
| First 5 years | 70-80% | 60-70% |
| Beyond 10 years | Data is less readily available and often influenced by factors such as individual patient characteristics, and treatment approaches | Data is less readily available and often influenced by factors such as individual patient characteristics, and treatment approaches |
Complications and Side Effects: Mixed Cellularity Hodgkins Lymphoma
Mixed Cellularity Hodgkin Lymphoma (MCHL) treatment, while effective, can unfortunately lead to various complications and side effects. Understanding these potential consequences is crucial for patients and healthcare providers to proactively manage them and ensure optimal outcomes. Careful monitoring and proactive management strategies are essential to mitigate these risks and enhance the overall quality of life during and after treatment.Treatment for MCHL, like many cancer therapies, targets rapidly dividing cells, which unfortunately also includes healthy cells.
This can lead to a range of side effects, some temporary and others potentially long-lasting. These side effects vary greatly depending on the specific treatment regimen, the individual patient’s response, and the overall health status.
Potential Treatment-Related Complications
MCHL treatment, often involving chemotherapy, radiation therapy, or a combination of both, can potentially lead to a range of complications. These complications can affect various organ systems and impact a patient’s daily life. Careful monitoring and supportive care are essential to mitigate these risks.
Common Side Effects of MCHL Treatment
Various side effects are commonly associated with MCHL treatment. These effects can range from mild discomfort to more serious complications. Early recognition and prompt management are crucial for minimizing their impact on patients.
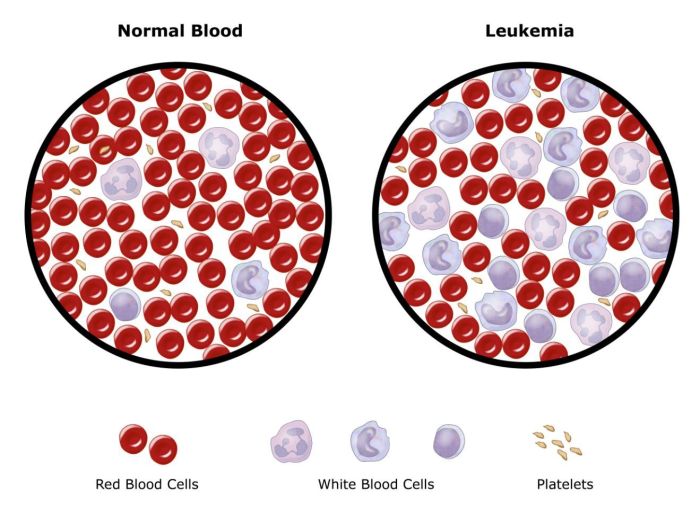
- Hematologic Effects: Chemotherapy drugs often suppress the production of blood cells, potentially leading to anemia (low red blood cell count), neutropenia (low white blood cell count), and thrombocytopenia (low platelet count). These conditions increase the risk of infections, fatigue, and bleeding. Careful monitoring of blood counts is essential to adjust treatment regimens and prevent serious complications. A patient experiencing significant anemia might require blood transfusions.
- Gastrointestinal Effects: Nausea, vomiting, and diarrhea are common gastrointestinal side effects of chemotherapy. These can significantly impact a patient’s nutritional intake and overall well-being. Medications and dietary modifications can help manage these symptoms. For example, antiemetic medications can significantly reduce nausea and vomiting, allowing patients to maintain their nutritional intake.
- Cardiovascular Effects: Some chemotherapy drugs can potentially affect the heart, leading to long-term cardiac complications. Careful monitoring of cardiac function is necessary, particularly during and after treatment. This often includes regular electrocardiograms (ECGs) and echocardiograms to assess the heart’s health.
- Neurological Effects: Some patients experience neurological side effects, including peripheral neuropathy (nerve damage in the extremities), headaches, and cognitive changes. These side effects can be managed with supportive care and potentially specific medications. Careful monitoring of neurological function is crucial, and early intervention can significantly reduce the severity of these side effects.
- Reproductive Effects: Chemotherapy can impact fertility in both men and women. Patients considering family planning should discuss potential reproductive consequences with their oncologist. Pre-emptive measures, such as sperm banking, might be considered for male patients. Some chemotherapy regimens are associated with a higher risk of infertility, and this should be addressed during the treatment plan discussion.
- Infections: Suppressed immune systems due to chemotherapy increase the risk of infections. Patients need to be vigilant about infection prevention and receive appropriate treatment for any infections that arise. Patients undergoing chemotherapy may be more susceptible to opportunistic infections, highlighting the importance of regular monitoring and preventative measures.
Managing Treatment-Related Side Effects
Proactive management of treatment-related side effects is crucial for maximizing patient comfort and well-being during and after MCHL treatment. This involves close collaboration between the patient, healthcare team, and support systems.
- Patient Education: Thorough education about potential side effects and management strategies is vital. This allows patients to actively participate in their care and recognize warning signs. Detailed information provided to patients about potential side effects empowers them to actively participate in their care.
- Symptom Monitoring: Regular monitoring of symptoms, including detailed records of their severity and duration, is essential. This enables early intervention and adjustments to treatment plans when needed. Detailed symptom tracking by the patient allows the healthcare team to identify trends and make necessary adjustments.
- Supportive Care: Supportive care strategies, including pain management, nutrition support, and psychological support, play a vital role in improving patient comfort and well-being. Nutrition counseling can help patients maintain a healthy diet despite gastrointestinal side effects.
- Medications: A range of medications can help manage specific side effects. Medications to reduce nausea and vomiting, manage pain, and support blood cell production are often part of the treatment plan. Regular follow-up with the healthcare team to adjust medication as needed is essential.
Research and Future Directions
Unraveling the complexities of Mixed Cellularity Hodgkin Lymphoma (MCHL) requires ongoing research. Current efforts are focused on understanding the disease’s biology, improving diagnostic accuracy, and developing more effective and less toxic treatment options. This exploration of the future of MCHL research promises to significantly enhance patient outcomes.
Current Research Efforts
Research into MCHL is multifaceted, encompassing various areas. Scientists are actively investigating the genetic and molecular underpinnings of MCHL, aiming to identify specific biomarkers that can aid in early diagnosis and prognosis. This includes exploring the role of specific genes and proteins in driving the disease, potentially leading to personalized treatment strategies. Immunotherapy approaches are also being rigorously examined, with the goal of leveraging the immune system to target and eliminate MCHL cells more effectively.
Studies are evaluating the use of novel agents, such as targeted therapies, in combination with standard chemotherapy regimens to potentially enhance efficacy while minimizing side effects.
Areas Needing Further Research
Despite significant progress, several areas require further investigation. One critical area is the development of more accurate and less invasive diagnostic tools. Currently, diagnosis often relies on biopsy, which can be associated with complications. Research is needed to identify blood-based biomarkers that can accurately diagnose MCHL, facilitating earlier intervention. Furthermore, understanding the long-term effects of MCHL treatments, particularly on fertility and cardiovascular health, is crucial.
Prospective studies are necessary to address these concerns. A critical area for research is tailoring treatment strategies based on specific genetic profiles. Identifying genetic markers that predict treatment response could lead to personalized treatment plans, maximizing effectiveness and minimizing adverse effects.
Importance of Research in Improving Treatments and Outcomes
Research plays a pivotal role in improving MCHL treatments and outcomes. By understanding the disease’s intricacies, researchers can develop targeted therapies that effectively eliminate MCHL cells while sparing healthy tissues. This leads to fewer side effects and improved quality of life for patients. The pursuit of improved diagnostic tools also shortens the time to diagnosis and treatment, potentially impacting patient outcomes positively.
Incorporating genetic and molecular insights into treatment strategies allows for personalized approaches, maximizing efficacy and minimizing harm. Ultimately, ongoing research will contribute to the development of more precise and less toxic therapies, significantly enhancing patient survival and quality of life.
Potential Future Directions in MCHL Research
Future directions in MCHL research should focus on developing more personalized treatment strategies. This includes utilizing genetic profiling to identify specific genetic markers that predict treatment response and tailor therapies accordingly. Another important avenue is exploring novel immunotherapeutic approaches, including chimeric antigen receptor (CAR) T-cell therapy, to harness the power of the immune system to target and destroy MCHL cells.
Moreover, research into novel combinations of existing therapies could yield improved outcomes, leading to enhanced efficacy and reduced side effects. Developing non-invasive diagnostic tools, such as blood tests, is crucial for earlier detection and improved patient management.
The Need for Clinical Trials in MCHL
Clinical trials are essential to translate research findings into improved patient care. These trials provide a controlled environment to evaluate the safety and efficacy of new therapies and diagnostic tools in a diverse population of MCHL patients. Clinical trials are crucial for evaluating the potential benefits and risks of new treatments. By testing these new strategies, researchers can assess their effectiveness in treating MCHL and determine the optimal treatment approach for individual patients.
Through clinical trials, researchers can collect data on the long-term effects of different treatments, providing valuable insights into potential side effects and long-term outcomes. Clinical trials are essential for advancing MCHL treatment and ultimately improving the quality of life for patients.
Last Word
In conclusion, mixed cellularity Hodgkin lymphoma presents a complex picture demanding a comprehensive understanding of its various facets. From its defining characteristics and diagnostic procedures to the nuanced treatment strategies and prognosis, this exploration highlights the importance of early detection, tailored treatment, and ongoing research. The 5-year and 10-year survival rates, while encouraging, underscore the necessity for ongoing efforts to improve outcomes and manage potential complications.
The future of MCHL treatment hinges on continued research and innovation, particularly in identifying personalized approaches and improving existing therapies.
/leukemia-myeloid-250x-at-35mm-this-type-of-leukemia-has-its-origin-in-the-bone-marrow-myeloid-tissue-it-involves-a-malignant-proliferation-of-immature-white-blood-cells-this-action-can-crowd-out-production-of-rbc-s-and-platelets-leading-to-an--58aca68c3df78c345b81d051.jpg?w=700)
