Back pain as a symptom of lung cancer is a complex and often overlooked possibility. While back pain is frequently associated with other conditions, its unusual manifestation in relation to lung cancer warrants careful consideration. This exploration delves into the potential link, highlighting the various ways back pain can manifest, its location, characteristics, and the underlying mechanisms at play.
This in-depth look at the interplay between back pain and lung cancer will cover the potential physiological pathways, the role of metastasis, and the types of lung cancer most likely to cause back pain. We’ll also examine the differentiating factors that distinguish this type of back pain from other causes and the critical diagnostic considerations involved.
Introduction to Back Pain and Lung Cancer
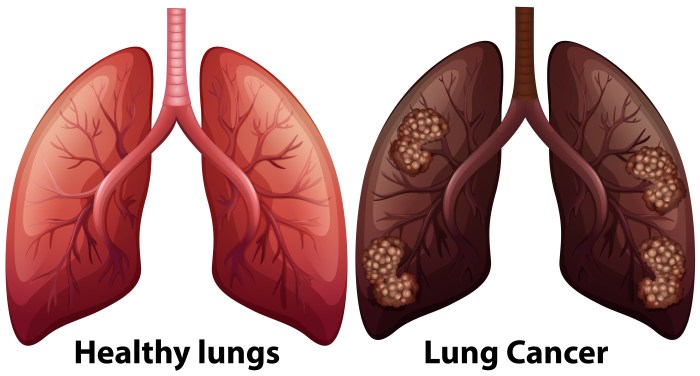
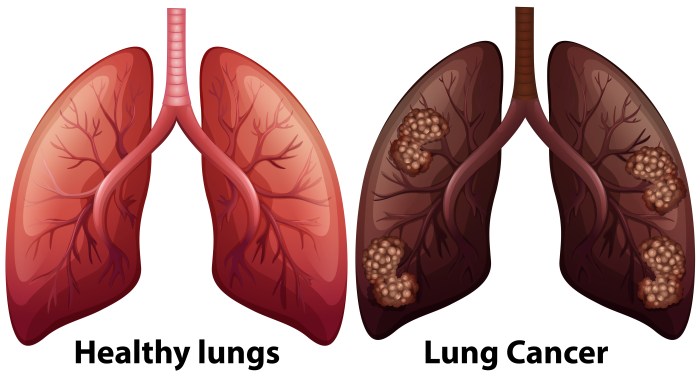
Back pain is a common ailment, often caused by musculoskeletal issues, injuries, or lifestyle factors. However, back pain can sometimes be a subtle yet crucial indicator of an underlying, more serious condition. One such possibility is the presence of lung cancer, although this association is less common and frequently presents with atypical symptoms. Understanding the potential link between back pain and lung cancer is essential for early detection and appropriate medical intervention.The connection between back pain and lung cancer is not straightforward.
Unlike other symptoms like coughing or shortness of breath, back pain as a primary symptom of lung cancer is relatively unusual. This is because lung cancer typically involves the lungs and surrounding structures, not the spine or musculoskeletal system directly. However, the spread of cancer to distant sites, a process known as metastasis, can cause pain in areas seemingly unrelated to the original tumor location.
This phenomenon, when linked to lung cancer, requires a careful assessment by medical professionals to differentiate it from other potential causes of back pain.
Manifestations of Back Pain in Lung Cancer
Back pain associated with lung cancer can manifest in diverse ways. The pain might be dull, aching, or sharp, and its intensity can vary from mild to severe. It’s not always constant and can fluctuate throughout the day. Crucially, the pain might be localized to a specific area of the back or radiate to other parts of the body.
The characteristics of the pain, including its location, intensity, and frequency, can provide valuable clues to its underlying cause.
Location and Characteristics of Back Pain
The location of back pain related to lung cancer metastasis is not always predictable. It can be in the upper back, lower back, or even in the mid-back region. Pain can also radiate from the back to the sides or down the arms or legs, mimicking other types of musculoskeletal conditions. The pain’s intensity and duration can vary significantly between individuals and can be influenced by factors such as the extent of the metastasis and the individual’s overall health.
While back pain is often shrugged off as a common ailment, it can sometimes be a surprisingly subtle sign of something more serious, like lung cancer. It’s crucial to remember that understanding your body and seeking medical attention when needed is key. Fortunately, there are various methods to address the cosmetic concerns associated with stretch marks, such as how to get rid of stretch marks , but if you experience persistent back pain, don’t hesitate to consult a doctor for a proper diagnosis.
This is especially important given the potential for underlying conditions like lung cancer, and early detection is always best.
Pain is often worse at night or with certain movements, like coughing or bending.
Mechanisms of Back Pain from Lung Cancer
The mechanisms behind back pain in lung cancer are typically linked to the spread of cancer cells (metastasis) to areas outside the lungs. These cancer cells can settle in the bones, potentially causing inflammation, pressure, or damage to the surrounding tissues. This process can result in localized pain, particularly in the spine and surrounding areas. In some cases, the cancerous growth can impinge on nerves, leading to a more severe or sharp pain sensation.
Additionally, the body’s response to the presence of cancer cells can further contribute to the pain experience.
Comparison of Typical Back Pain and Lung Cancer-Related Back Pain
| Feature | Typical Back Pain | Lung Cancer-Related Back Pain |
|---|---|---|
| Symptoms | Muscle soreness, stiffness, tightness, or spasms. Possible localized pain. | May include dull, aching, or sharp pain; may radiate to other areas; can be worse at night or with certain movements. |
| Severity | Generally mild to moderate, often manageable with over-the-counter pain relievers. | Can range from mild to severe, potentially debilitating. Severity can fluctuate. |
| Duration | Typically resolves within a few days or weeks, depending on the cause. | Can persist or worsen over time, especially if the cancer continues to spread. |
| Other symptoms | Often associated with recent injury, poor posture, or strenuous activity. | Often accompanied by other lung cancer symptoms like persistent cough, shortness of breath, weight loss, fatigue, or chest pain. |
Underlying Mechanisms
Back pain, a seemingly unrelated symptom, can sometimes be a crucial indicator of a more serious condition, such as lung cancer. Understanding the underlying mechanisms connecting these two seemingly disparate issues is vital for early diagnosis and appropriate treatment. Lung cancer, particularly when it spreads (metastasizes), can exert pressure on and damage surrounding structures, leading to pain, often felt in the back.The journey from lung cancer to back pain is complex, involving a cascade of physiological events and the intricate interplay between the cancer cells, the body’s defense mechanisms, and the structures of the spine and surrounding tissues.
Back pain can sometimes be a sneaky symptom of lung cancer, often dismissed as something less serious. While it’s crucial to get any persistent back pain checked out by a doctor, it’s also important to maintain a healthy lifestyle. Eating a balanced diet, including fruits like pineapple, which, according to what does pineapple do for women , can offer various benefits for women’s health, can play a role in overall well-being and potentially reduce the risk of certain health issues.
Still, if you’re experiencing ongoing back pain, it’s essential to consult a medical professional for proper diagnosis and treatment.
This exploration delves into the specific pathways through which lung cancer can cause back pain.
Metastasis and its Role in Back Pain
Lung cancer cells, if left unchecked, can detach from the primary tumor site and travel through the bloodstream or lymphatic system to other parts of the body. This process, known as metastasis, is a critical factor in the development of back pain. Metastatic cancer cells, reaching the spine and adjacent structures, can disrupt the normal function of these tissues, leading to inflammation, pain, and potential neurological complications.
Types of Lung Cancer Predisposed to Cause Back Pain
Certain types of lung cancer are more prone to metastasizing to the spine than others. Non-small cell lung cancer (NSCLC) is a more common type and often exhibits a tendency to spread to distant sites, including the spine. Specific subtypes within NSCLC, such as adenocarcinoma and squamous cell carcinoma, can also have a higher likelihood of spreading to the skeletal system.
Effects of Tumors on Surrounding Tissues, Including the Spine
Tumors, whether primary or metastatic, can exert pressure on adjacent tissues, including the vertebrae, ligaments, and muscles of the spine. This pressure can lead to pain, inflammation, and potentially compromise the structural integrity of the spine. Furthermore, the inflammatory response triggered by the presence of cancer cells can exacerbate the pain signals. For example, a tumor pressing on the spinal cord can cause severe pain radiating to the back and extremities.
Nerve Compression or Irritation as a Cause of Back Pain
Lung cancer metastases can directly compress or irritate nerves within the spine and surrounding areas. This nerve compression or irritation is a significant source of back pain. The spinal nerves, responsible for transmitting sensory information, can be affected by the tumor mass, leading to a range of symptoms, including pain, numbness, and tingling in the back, arms, or legs.
This pressure can be caused by tumor growth, inflammation, or edema (swelling).
Potential Metastasis Sites from Lung Cancer to the Spine and Surrounding Structures
The following table highlights potential locations of lung cancer metastasis that can affect the spine and adjacent structures, often leading to back pain. Note that this isn’t an exhaustive list, and other sites may also be affected.
| Potential Metastasis Site | Potential Effect on Spine/Surrounding Structures |
|---|---|
| Vertebrae (spinal bones) | Direct pressure on the spinal cord or nerve roots, leading to pain, numbness, and potentially spinal instability. |
| Spinal Cord | Compression or irritation of the spinal cord, resulting in severe back pain, muscle weakness, and sensory loss. |
| Nerve Roots | Compression or irritation of nerve roots emanating from the spinal cord, leading to pain radiating to the limbs, as well as numbness and tingling. |
| Paravertebral Tissues (tissues alongside the spine) | Inflammation and pressure on surrounding muscles, ligaments, and tissues, exacerbating back pain. |
| Ligaments and Joints | Weakening of supporting structures and potential for spinal instability, increasing the risk of fractures or dislocations. |
Differentiating Factors
Back pain is a common ailment, often stemming from a multitude of causes, ranging from simple muscle strains to more serious conditions. Distinguishing back pain related to lung cancer from other causes is crucial for timely and accurate diagnosis and treatment. This necessitates a careful consideration of the patient’s overall medical history, specific symptoms, and the nature of the pain itself.Identifying the precise cause of back pain, especially when linked to lung cancer, hinges on distinguishing characteristics that set it apart from other, more benign conditions.
This involves a thorough evaluation of the pain’s location, intensity, duration, and associated symptoms. Recognizing these subtle differences can significantly impact the diagnostic process and guide appropriate treatment strategies.
Factors Differentiating Lung Cancer-Related Back Pain
Differentiating back pain originating from lung cancer from other causes requires careful consideration of several factors. These factors include the patient’s medical history, the characteristics of the pain, and the presence of any associated symptoms.
Typical Characteristics of Lung Cancer-Related Back Pain
Lung cancer-related back pain often exhibits certain characteristics that can help distinguish it from other conditions. These characteristics include the pain’s insidious onset, progressive nature, and its tendency to be persistent and unremitting. The pain may also be accompanied by other symptoms, such as unexplained weight loss, fatigue, or night sweats. Importantly, the pain may not be directly localized to the site of the tumor.
In some instances, the pain can be diffuse, encompassing a wide area of the back.
Comparison with Other Common Back Pain Conditions
| Cause | Location | Characteristics | Associated Symptoms | Duration |
|---|---|---|---|---|
| Muscle Strain | Localized to specific muscle groups | Sharp, aching, or throbbing | Muscle tenderness, stiffness | Acute (days to weeks) |
| Spinal Stenosis | Lower back, radiating to buttocks or legs | Numbness, tingling, pain worsened by standing or walking | Neurological symptoms (e.g., weakness, numbness) | Progressive, often worse with activity |
| Osteoporosis | Lower back, spine | Aching, gradual onset, often worse at night | Fractures, loss of height | Chronic, often worsening over time |
| Lung Cancer | Can be localized or diffuse, often non-specific | Persistent, unremitting, progressive, insidious onset | Unexplained weight loss, fatigue, night sweats, cough | Chronic, worsening over time |
The table above highlights key differences in location, characteristics, and associated symptoms between various back pain causes and back pain related to lung cancer. While a localized pain in a muscle group might suggest a muscle strain, a persistent, non-specific pain accompanied by systemic symptoms strongly warrants further investigation.
Importance of Medical History and Symptoms
A comprehensive medical history, including smoking history, exposure to asbestos, and previous respiratory illnesses, is vital in assessing the possibility of lung cancer. The presence of other symptoms, such as a persistent cough, shortness of breath, or hemoptysis (coughing up blood), should also be meticulously noted. These factors can significantly influence the likelihood of lung cancer as the cause of back pain.
Consider a patient’s overall health status, recent illnesses, and other relevant factors.
Importance of Excluding Other Potential Causes
Before attributing back pain to lung cancer, it’s crucial to exclude other potential causes. This involves conducting thorough diagnostic evaluations, including imaging studies (such as X-rays, CT scans, or MRIs), blood tests, and possibly a biopsy. The goal is to confirm the presence of a malignancy or rule out other conditions that could be responsible for the pain.
Failure to rule out these other causes could lead to misdiagnosis and inappropriate treatment.
Diagnostic Considerations
Pinpointing the cause of back pain, especially when coupled with potential lung cancer, requires a meticulous and multifaceted approach. A thorough diagnostic evaluation involves a combination of physical examinations, patient histories, imaging techniques, blood tests, and other investigations. This process aims to distinguish between back pain stemming from lung cancer and other, more common causes.
Thorough Physical Examination and Patient History
A comprehensive physical examination is crucial in assessing the nature and extent of back pain. This includes evaluating posture, range of motion, muscle strength, and neurological function. A detailed patient history, encompassing the onset, duration, location, and character of the pain, as well as any associated symptoms like coughing, shortness of breath, or weight loss, is equally important.
The physician will need to ascertain the patient’s medical history, including any prior diagnoses, surgeries, or treatments. The collected data provides valuable context and helps narrow down potential diagnoses.
Imaging Techniques
Imaging plays a vital role in diagnosing lung cancer and its potential impact on the spine. X-rays are often the initial imaging modality employed. They provide basic anatomical information, helping to identify any bone abnormalities or fractures. Computed Tomography (CT) scans offer a more detailed view of the spine and surrounding tissues, revealing potential soft tissue masses or bone lesions.
Magnetic Resonance Imaging (MRI) is particularly useful in assessing the condition of soft tissues and spinal cord structures. MRI scans can provide high-resolution images of the spinal cord and surrounding tissues, which can be crucial for detecting subtle signs of involvement. Positron Emission Tomography (PET) scans, often used in conjunction with CT scans (PET-CT), can highlight areas of metabolic activity, aiding in identifying potential tumors, including those in the lungs or spine.
Blood Tests and Other Investigations
Blood tests, such as complete blood counts (CBCs) and tumor markers (e.g., CA 125, CEA), can provide insights into the patient’s overall health and potential malignancy. Elevated levels of certain tumor markers may suggest the presence of cancer, though further investigation is usually required to confirm the diagnosis. Biopsies, if necessary, provide a definitive diagnosis, enabling the examination of tissue samples under a microscope to ascertain the nature of any suspicious lesions.
Summary of Diagnostic Tests
| Diagnostic Test | Relevance to Back Pain and Lung Cancer |
|---|---|
| X-ray | Initial screening to identify bone abnormalities or fractures. |
| CT Scan | Detailed visualization of the spine and surrounding tissues, potentially revealing soft tissue masses or bone lesions. |
| MRI | High-resolution imaging of soft tissues and spinal cord structures, useful for detecting subtle signs of involvement. |
| PET Scan (often with CT) | Identifies areas of metabolic activity, aiding in identifying potential tumors in the lungs or spine. |
| Blood Tests (CBC, Tumor Markers) | Assess overall health and potential malignancy. Elevated levels may suggest cancer but require further confirmation. |
| Biopsy | Definitive diagnosis by examining tissue samples under a microscope. |
Limitations of Diagnostic Methods
It’s crucial to recognize the limitations of various diagnostic methods in identifying back pain caused by lung cancer. Early-stage lung cancer may not manifest obvious symptoms, including back pain, making detection challenging. Similarly, other conditions can mimic the symptoms of lung cancer-related back pain. Proper interpretation of imaging results requires careful consideration of the patient’s history and physical examination findings.
The absence of definitive findings on diagnostic tests does not automatically rule out lung cancer as a potential cause. Subtle changes or subtle involvement may be missed, necessitating a comprehensive approach.
Treatment and Management
Managing back pain in patients suspected of having lung cancer requires a multifaceted approach, acknowledging the complex interplay between the cancer and the pain itself. Treatment strategies must address both the underlying lung cancer and the resulting back pain, considering potential side effects of cancer therapies. A crucial element is the individualization of care, as each patient’s experience and response to treatment will vary.Effective pain management is integral to the overall well-being of patients experiencing back pain related to suspected lung cancer.
It improves quality of life and allows for better participation in cancer treatment regimens. Pain management strategies should be tailored to the intensity and nature of the pain, considering the patient’s preferences and medical history.
Pain Management Strategies
Pain management is crucial for improving patient comfort and quality of life. A range of non-pharmacological and pharmacological approaches are employed to effectively address the pain. These strategies aim to reduce the intensity of pain signals and enhance the patient’s coping mechanisms. Non-pharmacological options often include physical therapy, relaxation techniques, and counseling.
Treatment Options for Lung Cancer
Lung cancer treatment options vary based on the stage and type of cancer, as well as the patient’s overall health. Common treatments include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment often involves a multidisciplinary approach, considering the patient’s preferences, the characteristics of the cancer, and potential side effects.
Impact of Lung Cancer Treatments on Back Pain
The treatments for lung cancer can sometimes affect the back pain, either by directly addressing the underlying cause or by inducing side effects that exacerbate or ameliorate the pain. For instance, some chemotherapy regimens may cause inflammation, potentially worsening existing back pain. Conversely, successful cancer treatment could lead to a reduction in tumor pressure on the spinal cord, thus alleviating the pain.
It’s important to monitor the patient’s response closely and adjust treatment plans as needed.
Multidisciplinary Approach to Care
A multidisciplinary approach, involving oncologists, pain management specialists, physical therapists, and other healthcare professionals, is vital in managing patients with both back pain and suspected lung cancer. This collaborative approach ensures a comprehensive assessment, tailored treatment plans, and ongoing support for the patient. The expertise of various specialists allows for a holistic understanding of the patient’s needs and promotes coordinated care.
Treatment Options Table
| Treatment Category | Treatment Options for Back Pain | Treatment Options for Lung Cancer |
|---|---|---|
| Pharmacological | Analgesics (NSAIDs, opioids), nerve pain medications | Chemotherapy, targeted therapy, immunotherapy |
| Non-Pharmacological | Physical therapy, exercise, relaxation techniques, acupuncture | Surgery, radiation therapy, targeted therapy |
| Interventional | Epidural injections, nerve blocks | Clinical trials, palliative care |
Case Examples
A patient with a history of chronic back pain and a recent diagnosis of lung cancer experienced increased pain intensity after starting chemotherapy. The pain management team adjusted the medication regimen, incorporated physical therapy, and implemented relaxation techniques, resulting in a significant reduction in pain and improved quality of life. Another patient, diagnosed with stage III lung cancer, underwent surgery and radiation therapy.
The back pain, initially attributed to tumor pressure, subsided significantly after the surgical removal of the tumor. These examples illustrate the diverse nature of the patient experience and the importance of a tailored approach to care.
Illustrative Cases
Back pain, a seemingly common ailment, can sometimes be a cryptic symptom, masking a more serious underlying condition like lung cancer. Understanding how this connection manifests in patients is crucial for early diagnosis and effective treatment. These illustrative cases will shed light on the diagnostic journey and management strategies employed.
Case Study 1: Suspected Lung Cancer Metastasis
A 65-year-old male presented with persistent, dull back pain, radiating to his right hip. He reported a history of smoking for 40 years and had recently experienced some shortness of breath. Physical examination revealed tenderness in the lower back, with no other significant findings. Initial blood tests and imaging studies (X-rays and CT scans) showed no obvious fractures or bony lesions.Given the patient’s risk factors and the persistent pain, a suspicion of lung cancer metastasis to the spine arose.
Further investigations included a chest X-ray, which revealed a nodule in the right lung. A subsequent CT scan of the chest and abdomen confirmed the presence of a tumor in the right lung, with suspected metastasis to the lumbar spine. A biopsy of the lung nodule confirmed the diagnosis of non-small cell lung cancer (NSCLC).The patient underwent chemotherapy and radiation therapy targeted at the lung tumor.
While back pain is often associated with everyday aches and pains, it can sometimes be a surprising symptom of lung cancer. It’s important to remember that various factors can contribute to back pain, but if you’re experiencing persistent back pain alongside other unusual symptoms, it’s crucial to consult a doctor. Luckily, when you’re battling a cold, sipping on some soothing herbal teas can offer a much-needed respite.
For a comprehensive list of the best teas for a cold, check out this resource: best teas for a cold. However, persistent back pain, especially when accompanied by other symptoms, should never be ignored and warrants a medical evaluation.
Pain management strategies, including analgesics and physical therapy, were implemented to address the back pain. The patient’s pain gradually subsided, and he experienced a marked improvement in his overall condition. Follow-up scans monitored the tumor’s response to treatment.
Case Study 2: Atypical Presentation
A 72-year-old female presented with a sharp, intermittent back pain, accompanied by numbness in her right leg. She denied any smoking history, but had a history of asbestos exposure in her previous occupation. Initial examinations and imaging studies did not reveal any obvious abnormalities. Her symptoms persisted, leading to further investigations.Suspecting a possible connection between her back pain and lung cancer, a PET scan was performed, which revealed a tumor in the left lung.
Biopsy confirmed the presence of small cell lung cancer (SCLC). This case highlights the importance of considering atypical presentations and exploring potential occupational risk factors in the diagnostic process. The patient was promptly started on chemotherapy, and her condition was monitored closely.
Summary of Illustrative Cases
| Case | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| 1 | Persistent dull back pain, radiating to right hip, shortness of breath | Lung cancer (NSCLC) with suspected metastasis to the lumbar spine | Chemotherapy, radiation therapy, pain management |
| 2 | Sharp, intermittent back pain, numbness in right leg, history of asbestos exposure | Lung cancer (SCLC) | Chemotherapy, close monitoring |
Patient Journey and Outcome
Both cases illustrate the importance of a thorough assessment, including considering the patient’s history, risk factors, and presenting symptoms. Early detection and appropriate treatment can significantly improve the patient’s quality of life and overall outcome. The journey often involves a multidisciplinary approach, including oncologists, radiologists, and pain management specialists. Regular follow-up appointments and monitoring are essential for effective management.
The outcomes in both cases demonstrated that with timely diagnosis and comprehensive treatment, patients can experience significant relief and improved quality of life, even with the presence of lung cancer.
Public Health Implications: Back Pain As A Symptom Of Lung Cancer

Back pain, a common ailment, can sometimes be a crucial early warning sign of a more serious condition, such as lung cancer. Raising awareness about this connection is vital for early detection, leading to improved treatment outcomes and potentially saving lives. Understanding the potential link between back pain and lung cancer allows individuals and healthcare professionals to approach such symptoms with heightened vigilance.Early diagnosis and intervention are paramount in managing lung cancer effectively.
Awareness campaigns, coupled with readily available resources for both patients and healthcare providers, can play a pivotal role in this process. By equipping individuals with the knowledge to recognize potential symptoms and encouraging prompt medical attention, we can potentially improve outcomes and reduce the impact of this disease.
Importance of Raising Awareness
Raising awareness about back pain as a possible symptom of lung cancer is crucial for early detection. Many individuals might dismiss back pain as a common ailment, delaying necessary medical attention. This delay can lead to a more advanced stage of the disease, making treatment more challenging and potentially reducing survival rates. By educating the public about this less-common presentation of lung cancer, we can empower individuals to seek medical evaluation when experiencing persistent or unexplained back pain, particularly if accompanied by other concerning symptoms.
Available Resources for Patients and Healthcare Professionals
Access to reliable information and support is vital for both patients and healthcare professionals. Well-structured educational materials and online resources can help patients understand the potential connection between back pain and lung cancer. These resources should also offer guidance on when to seek medical attention and which healthcare professionals to consult. For healthcare providers, access to updated diagnostic guidelines, treatment protocols, and reliable diagnostic tools can significantly improve the quality of care provided to patients experiencing back pain.
Potential for Early Detection and Improved Outcomes, Back pain as a symptom of lung cancer
Early detection of lung cancer is directly correlated with improved treatment outcomes. By recognizing back pain as a potential symptom, individuals can seek medical attention sooner, potentially leading to earlier diagnosis and more effective treatment options. Early intervention can significantly enhance the chances of successful treatment and improve the quality of life for affected individuals. For instance, if a patient with back pain is also experiencing other symptoms like persistent cough, unexplained weight loss, or shortness of breath, they should promptly consult a physician.
Resources for Patients and Healthcare Providers
| Resource Category | Description |
|---|---|
| Patient Resources | Websites providing information on lung cancer symptoms, including back pain, and advice on when to seek medical attention. Support groups offering emotional and practical support to patients and their families. |
| Healthcare Provider Resources | Medical journals and publications with the latest research on lung cancer diagnosis and treatment, particularly concerning less-common presentations like back pain. Guidelines from reputable medical organizations on appropriate diagnostic procedures and treatment protocols for suspected lung cancer. |
Preventative Measures and Regular Check-ups
Smoking cessation is a critical preventative measure for reducing the risk of lung cancer. Furthermore, individuals with a family history of lung cancer or those with a history of smoking should prioritize regular check-ups with their healthcare providers. These check-ups, which include routine lung function tests and cancer screenings, can help identify potential problems early on, leading to timely intervention and improved outcomes.
Early detection through regular check-ups can potentially save lives and improve overall health. For example, annual chest X-rays for high-risk individuals can aid in early detection.
Closure
In conclusion, recognizing back pain as a potential symptom of lung cancer is crucial for early detection and improved patient outcomes. This article highlights the multifaceted nature of this connection, offering a comprehensive overview of the underlying mechanisms, diagnostic procedures, and treatment approaches. By understanding the nuances of this unusual symptom, healthcare professionals and patients can collaborate to navigate this complex health challenge more effectively.