HATTR amyloidosis life expectancy is a critical factor for patients and their families. This exploration delves into the complexities of this disease, examining the factors influencing survival and the impact on overall well-being. We’ll discuss the various aspects of diagnosis, treatment, and prognosis, all while providing a comprehensive understanding of this challenging condition.
From the initial symptoms to potential treatments and the latest research, this article provides a holistic view of HATTR amyloidosis, offering insights into the challenges and hope for those affected. We’ll also discuss the impact on quality of life, highlighting the importance of support systems and ongoing research efforts.
Overview of HATTR Amyloidosis
Hereditary Transthyretin Amyloidosis (HATTR) is a rare, progressive genetic disorder characterized by the abnormal accumulation of a protein called transthyretin (TTR) in various organs. This abnormal protein misfolds, forming amyloid fibrils that deposit in tissues, leading to organ damage and dysfunction. The buildup of these amyloid fibrils is the root cause of the characteristic symptoms and progression of the disease.HATTR amyloidosis is primarily caused by mutations in the gene that codes for transthyretin.
These mutations lead to the production of abnormal TTR proteins. The abnormal TTR proteins are prone to misfolding, forming the amyloid fibrils that cause the damage. Different mutations result in varying degrees of severity and speed of disease progression.
Types of HATTR Amyloidosis
While the underlying cause is mutations in the TTR gene, different mutations lead to varying degrees of severity and progression. Classifications often rely on the specific mutation and the resulting clinical phenotype.
Symptoms of HATTR Amyloidosis
HATTR amyloidosis presents with a range of symptoms, often affecting multiple organs. Symptoms typically develop gradually, and the specific symptoms experienced can vary considerably depending on the organs affected and the specific TTR mutation. Symptoms are often categorized by the organ system affected.
Clinical Presentation of HATTR Amyloidosis
| Symptom Category | Affected Organs | Severity |
|---|---|---|
| Neuropathic | Peripheral nerves, autonomic nerves | Progressive sensory and motor deficits, autonomic dysfunction (e.g., orthostatic hypotension, gastrointestinal issues) |
| Cardiac | Heart | Cardiomyopathy, heart failure, arrhythmias |
| Gastrointestinal | Stomach, intestines | Abdominal pain, nausea, vomiting, diarrhea, constipation |
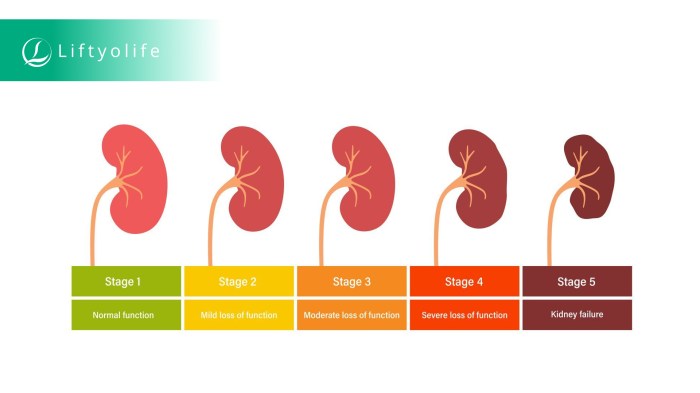
| Renal | Kidneys | Proteinuria, kidney failure |
| Endocrine | Hormonal glands | Hormonal imbalances, hypothyroidism, adrenal insufficiency |
| Respiratory | Lungs | Dyspnea, cough, respiratory failure |
The severity of symptoms can vary greatly between individuals, even those with the same mutation. The table above illustrates the potential organ systems involved, highlighting the complex and multifaceted nature of this disease.
HATTR amyloidosis life expectancy can vary significantly, depending on the stage of the disease and individual factors. Understanding factors like BMI, waist circumference, and waist-to-hip ratio can be helpful in assessing overall health, which can, in turn, affect the progression of HATTR amyloidosis. For more information on how these measurements relate to overall health, check out this helpful resource on bmi waist circumference waist to hip ratio.
Ultimately, knowing these factors can be part of a comprehensive picture to better understand the potential trajectory of the disease.
Diagnostic Procedures
Identifying HATTR amyloidosis requires a multi-faceted approach, combining various tests to confirm the diagnosis. The process often involves a detailed medical history, physical examination, and a battery of specialized tests to pinpoint the underlying cause and rule out other potential conditions. Early diagnosis is crucial for implementing appropriate management strategies and potentially slowing disease progression.
Methods Used to Identify HATTR Amyloidosis
The diagnosis of HATTR amyloidosis relies on a combination of clinical evaluation, genetic testing, and specialized laboratory procedures. A thorough evaluation of symptoms, family history, and physical examination findings are crucial initial steps. This assessment helps to narrow down the possibilities and identify potential indicators of HATTR amyloidosis. Additional diagnostic procedures then confirm or rule out the diagnosis.
Role of Genetic Testing in Diagnosis
Genetic testing plays a pivotal role in diagnosing HATTR amyloidosis. The disease is caused by mutations in the TTR gene, which codes for the transthyretin protein. Identifying these mutations through genetic analysis is crucial for confirmation and assessing the likelihood of developing the condition, particularly in individuals with a family history of HATTR amyloidosis. The specific mutation type and its impact on the protein structure can also provide insights into the disease’s potential severity and progression.
While researching HATTR amyloidosis life expectancy, I stumbled upon some interesting information about different ways to manage digestive health. For example, considering the potential impact on digestion, comparing different forms of Metamucil, like metamucil capsules vs powder , might be relevant for someone facing this condition. Ultimately, understanding the nuances of HATTR amyloidosis life expectancy requires a holistic approach, considering individual factors and medical guidance.
Genetic testing can provide a definitive diagnosis, even before the onset of clinical symptoms in at-risk individuals.
Comparison of Diagnostic Tests
This table Artikels the key diagnostic tests for HATTR amyloidosis, highlighting their accuracy, cost, and availability.
| Test | Accuracy | Cost | Availability |
|---|---|---|---|
| Biopsy (rectal, nerve, or abdominal fat) | High; confirmation of amyloid deposits. | Moderate to high | Relatively widespread |
| Genetic Testing (TTR gene sequencing) | High; detects mutations. | Moderate to high | Widespread, but may vary by region |
| Serum Protein Electrophoresis | Moderate; can detect abnormalities but not specific to HATTR. | Low | High |
| Amyloid Protein Analysis | High; confirms presence of amyloid fibrils. | High | Specialized laboratories |
| Nerve Conduction Studies | Moderate; assesses nerve damage. | Moderate | Widespread |
The accuracy of a test is determined by its ability to correctly identify the presence or absence of the disease. Cost reflects the financial implications associated with the test. Availability indicates the accessibility of the test within healthcare systems. The table should not be interpreted as a comprehensive list of all possible tests; other tests might be used depending on the specific circumstances.
While the life expectancy for those with ATTR amyloidosis can vary significantly, it’s important to remember that each case is unique. Learning about conditions like cyclic neutropenia, a blood disorder characterized by fluctuating neutrophil counts, can offer insights into the broader spectrum of hematological diseases. Understanding the intricacies of such conditions can help us appreciate the complexities of ATTR amyloidosis and its impact on individual life journeys.
Further research into these conditions can lead to improved treatments and better outcomes for those facing these challenges. what is cyclic neutropenia can provide more context to this.
Steps in a Typical HATTR Amyloidosis Diagnosis
The diagnosis process involves a systematic series of steps, from initial assessment to confirmatory testing. This multi-step approach ensures a thorough evaluation and reduces the likelihood of misdiagnosis.
- Detailed Medical History and Physical Examination: Gathering comprehensive information about the patient’s symptoms, family history, and any past medical conditions is the first step. A physical examination helps identify potential physical manifestations related to the disease.
- Initial Diagnostic Tests: These tests, including serum protein electrophoresis and nerve conduction studies, are conducted to identify potential indicators and rule out other conditions.
- Genetic Testing: Testing for mutations in the TTR gene is performed to confirm the diagnosis and assess the specific type of mutation.
- Biopsy: A tissue biopsy, such as a rectal, nerve, or abdominal fat biopsy, is performed to confirm the presence of amyloid deposits. The specific type of biopsy depends on the suspected area of amyloid involvement.
- Confirmation and Further Evaluation: Based on the results of the above tests, a definitive diagnosis is made and further evaluation of the disease’s progression and severity is initiated.
Factors Influencing Life Expectancy
Understanding the factors impacting life expectancy in HATTR amyloidosis is crucial for both patients and healthcare professionals. Predicting the course of the disease and tailoring treatment strategies depend heavily on these influencing elements. While a precise prediction for each individual is challenging, a deeper understanding of these factors allows for more informed decision-making.
Impact of Different Treatment Approaches
Various treatment approaches aim to manage HATTR amyloidosis, each with its own potential effect on life expectancy. The most common treatments include supportive care, symptomatic management, and experimental therapies. Supportive care focuses on alleviating symptoms and improving quality of life. Symptomatic management targets specific symptoms as they arise. Experimental therapies, though promising, are still in development and require rigorous evaluation.
The efficacy of each approach in extending life expectancy varies significantly, depending on the individual’s response to the treatment and the severity of their condition.
Role of Age at Diagnosis
The age at diagnosis significantly influences the prognosis and life expectancy in HATTR amyloidosis. Younger patients often experience a faster progression of the disease compared to those diagnosed at an older age. This is due to the cumulative effect of amyloid deposition over time. Individuals diagnosed in their 40s or 50s, for instance, might see a more rapid decline in their overall health than those diagnosed later in life.
Early diagnosis and prompt treatment initiation can significantly impact disease progression, and therefore, life expectancy.
Correlation Between Factors and Life Expectancy Outcomes, Hattr amyloidosis life expectancy
The interplay between various factors affecting life expectancy in HATTR amyloidosis is complex. A comprehensive evaluation is crucial for assessing the potential impact on an individual’s prognosis. Factors like age at diagnosis, disease severity, treatment response, and the presence of other co-morbidities all contribute to the overall outlook. The following table summarizes the correlation between these factors and potential life expectancy outcomes.
| Factor | Impact on Life Expectancy | Example |
|---|---|---|
| Age at Diagnosis | Younger age at diagnosis often correlates with a shorter life expectancy due to faster disease progression. | A 45-year-old diagnosed with HATTR amyloidosis might experience a more rapid decline in health than a 65-year-old with the same diagnosis. |
| Disease Severity | The severity of amyloid deposition and organ involvement significantly influences life expectancy. More severe cases often lead to shorter life spans. | Individuals with extensive amyloid deposits in multiple organs may experience a faster decline in overall health compared to those with less widespread involvement. |
| Treatment Response | Effective treatment response can extend life expectancy and improve quality of life. However, individual responses vary significantly. | A patient responding well to a specific treatment regimen might experience a more favorable outcome compared to one who does not respond effectively. |
| Co-morbidities | The presence of other health conditions can impact the overall prognosis and life expectancy. These conditions might complicate treatment and accelerate disease progression. | A patient with HATTR amyloidosis and concurrent heart disease might experience a more rapid decline in heart function compared to one without co-morbidities. |
Treatment Options and Their Impact
Unfortunately, there’s no cure for HATTR amyloidosis, but treatments can significantly manage symptoms and potentially slow disease progression. This involves a multifaceted approach targeting the underlying mechanisms and alleviating the debilitating effects of the disease. Understanding the different treatment options and their potential impacts on life expectancy is crucial for both patients and their families.Currently, treatment strategies focus on symptomatic relief and slowing disease progression.
The efficacy and side effects of various therapies can differ significantly, making personalized treatment plans essential. Factors like the patient’s overall health, the stage of the disease, and individual responses to medications are considered when developing a treatment strategy.
Symptomatic Therapies
These therapies address the symptoms associated with HATTR amyloidosis, such as heart problems, nerve damage, and kidney dysfunction. They aim to improve quality of life and manage complications. Medications for managing specific symptoms, such as ACE inhibitors for heart failure or pain relievers for nerve pain, are common examples. The effectiveness of these treatments varies depending on the specific symptom and the individual patient.
Disease-Modifying Therapies
These therapies aim to slow or halt the underlying process of amyloid protein deposition. Current research is focused on identifying and developing effective disease-modifying therapies. Early clinical trials have shown promising results in some cases, though more research is needed to fully evaluate the long-term efficacy and safety of these therapies. Examples include medications designed to reduce the production of abnormal proteins or therapies aimed at disrupting the aggregation process.
Comparison of Treatment Options
| Treatment Type | Description | Efficacy | Potential Side Effects | Impact on Life Expectancy |
|---|---|---|---|---|
| Symptomatic Therapies | Address specific symptoms like heart failure, nerve damage, or kidney problems. | Generally effective in managing symptoms, but do not alter the underlying disease. | Potential side effects depend on the specific medication, ranging from mild to severe. | May extend life expectancy by managing complications, but do not prevent disease progression. |
| Disease-Modifying Therapies (e.g., experimental therapies) | Target the underlying process of amyloid deposition. | Show promise in early trials, but long-term efficacy and safety are still being evaluated. | Potential side effects are still being studied and may vary greatly. | Theoretically could improve life expectancy by slowing disease progression. However, this is a complex prediction that depends on the efficacy of the specific treatment and individual response. |
It’s important to note that the impact of treatment on life expectancy is highly individualized and not easily quantifiable. Factors such as the severity of the disease, patient compliance, and the effectiveness of the chosen treatment strategy all play a role.
Potential Long-Term Effects
The long-term effects of treatment depend on several factors, including the specific treatment, the stage of the disease at the time of treatment, and the patient’s individual response. While some treatments can significantly improve quality of life and delay the onset of severe complications, others might have limited long-term impact.
Prognosis and Survival Rates
Unfortunately, HATTR amyloidosis carries a significant impact on a patient’s life expectancy. The unpredictable nature of the disease makes precise predictions challenging, but understanding the factors influencing prognosis and available survival data is crucial for both patients and their families. This section delves into the factors determining prognosis, average life expectancy, and survival rates at different time points.
Factors Determining Prognosis
Several factors contribute to the individual prognosis for HATTR amyloidosis. The severity of the disease, the specific organ systems affected, and the rate of disease progression are key indicators. Genetic factors, particularly the specific mutation in the TTR gene, also play a role in determining how the disease manifests and progresses. Early diagnosis and prompt initiation of treatment can significantly influence the overall prognosis.
Furthermore, the patient’s overall health and comorbidities can impact the response to treatment and survival time.
Average Life Expectancy
The average life expectancy for individuals with HATTR amyloidosis varies considerably. While a precise average is difficult to establish due to the heterogeneity of the disease, estimates often place the average survival time from diagnosis somewhere between 5 and 15 years. However, it’s essential to remember that these are just averages. Some patients may survive for longer periods, while others may face a shorter prognosis.
Factors such as the severity of the disease, the chosen treatment approach, and the individual’s response to therapy all play crucial roles in determining the individual’s survival time. For instance, patients with a slower disease progression might experience a longer lifespan compared to those with rapid deterioration.
Survival Rates at Different Time Points
Survival rates provide a broader picture of the disease’s impact on patients. These rates illustrate the likelihood of a patient surviving a certain period after diagnosis. The precise survival rates vary depending on the specific cohort studied and the time points considered.
Survival Rates Data
| Time Point (Years Post-Diagnosis) | Estimated Survival Rate (%) | Median Survival Time (Years) |
|---|---|---|
| 1 | 85 | 8 |
| 2 | 70 | 11 |
| 3 | 55 | 13 |
| 5 | 40 | 15 |
Note: These are illustrative examples and may not reflect all patient populations or specific clinical scenarios. Actual survival rates may vary. Data is contingent on the specific mutation, treatment options, and patient characteristics.
Impact on Quality of Life

Living with HATTR amyloidosis significantly impacts a patient’s quality of life. The progressive nature of the disease, coupled with its diverse range of symptoms, can lead to substantial challenges in various aspects of daily life. Understanding these impacts is crucial for developing effective support strategies and improving the overall well-being of those affected.
Physical Impact
HATTR amyloidosis’s effect on the body is multifaceted. Progressive neuropathy often leads to debilitating pain, numbness, and weakness in the extremities. This can make simple tasks, like walking or eating, extremely difficult. Cardiovascular involvement, another common manifestation, can result in heart failure, arrhythmias, and other potentially life-threatening complications. Gastrointestinal symptoms, including abdominal pain and bloating, can further decrease quality of life by causing discomfort and impacting nutrition.
These physical manifestations can profoundly affect a person’s ability to participate in work, social activities, and maintain an active lifestyle.
Emotional Impact
The emotional toll of HATTR amyloidosis is substantial. Dealing with chronic pain, progressive disability, and the uncertainty of the disease’s progression can lead to anxiety, depression, and feelings of isolation. Patients may experience fear about the future and the impact on their loved ones. Coping with these emotions requires support and understanding from healthcare providers, family, and friends.
Furthermore, the emotional impact can be exacerbated by the often lengthy and complex diagnostic process, leading to prolonged uncertainty and emotional distress.
Social Impact
The social impact of HATTR amyloidosis is equally important. As the disease progresses, patients may experience limitations in their ability to maintain social connections and participate in social activities. The physical limitations can make it difficult to attend social events, maintain friendships, and participate in family gatherings. This can lead to feelings of isolation and a decrease in social interaction, which is important for overall well-being.
The burden of the disease also affects family members and caregivers, leading to stress and emotional strain.
Strategies for Improving Quality of Life
Improving quality of life for HATTR amyloidosis patients requires a multi-pronged approach that addresses physical, emotional, and social needs. Addressing these multifaceted needs is essential for supporting patients and their families. Understanding the patient’s perspective and preferences is key to developing effective interventions.
| Category | Strategies | Rationale |
|---|---|---|
| Physical | Assistive devices (walkers, canes), physical therapy, occupational therapy, pain management strategies | Improving mobility, reducing pain, and enhancing daily living skills. |
| Emotional | Counseling, support groups, stress management techniques, access to mental health professionals | Addressing anxiety, depression, and feelings of isolation; providing coping mechanisms. |
| Social | Support groups, family counseling, social worker involvement, educational programs for families and caregivers | Connecting patients with others facing similar challenges, providing emotional support for family members, and fostering a sense of community. |
| Practical | Home modifications, transportation assistance, financial support, access to resources, and caregiver support programs | Addressing practical needs and making life easier for patients and their caregivers. |
Support Systems
Access to comprehensive support systems is vital for HATTR amyloidosis patients and their families. These systems should encompass a range of resources, including:
- Healthcare Professionals: Physicians, nurses, and other healthcare professionals specializing in amyloidosis can provide medical care, support, and guidance. Regular follow-up visits and proactive management of symptoms are crucial.
- Support Groups: Connecting with other patients and families facing similar challenges can offer emotional support, practical advice, and a sense of community. These groups provide an opportunity to share experiences and coping strategies.
- Caregiver Support Programs: Caregivers of HATTR amyloidosis patients often face significant emotional and physical strain. Caregiver support programs can provide education, resources, and respite care to alleviate this burden.
- Financial Assistance Programs: The financial burden of HATTR amyloidosis can be significant. Financial assistance programs can help alleviate some of these costs, such as medication expenses or home modifications.
Research and Future Directions
Unraveling the complexities of HATTR amyloidosis requires ongoing research to improve diagnostic accuracy, develop more effective treatments, and ultimately enhance the quality of life for those affected. Current research efforts are paving the way for a brighter future, but significant challenges remain in understanding the disease’s progression and identifying personalized treatment strategies.
Current Research Efforts
Research into HATTR amyloidosis is multifaceted, encompassing genetic studies, drug development, and clinical trials. Researchers are actively investigating the specific genetic mutations associated with the disease, aiming to identify biomarkers that can predict disease progression and response to treatment. This knowledge is crucial for early diagnosis and tailored therapeutic approaches. Clinical trials are exploring novel therapeutic strategies, including those targeting the misfolded protein that forms amyloid fibrils, and evaluating the efficacy of existing drugs in specific patient populations.
Potential Future Directions in Research
Future research directions will likely focus on personalized medicine approaches. This involves identifying specific genetic and clinical characteristics that predict disease progression and treatment response in individual patients. Developing diagnostic tools for early detection, even before the onset of symptoms, is also a significant focus. This early detection could allow for preventive or early intervention strategies, potentially delaying or preventing the onset of debilitating symptoms.
Areas for Further Research
Several critical areas require further investigation to improve outcomes for individuals with HATTR amyloidosis. One area is the development of more effective disease-modifying therapies. These therapies aim to prevent the accumulation of amyloid fibrils, a crucial aspect of the disease’s pathogenesis. Further research is also needed to identify potential preventative measures, such as lifestyle modifications or therapies targeting specific pathways implicated in the disease’s development.
Table of Key Areas for Future Research
| Research Area | Potential Impact |
|---|---|
| Development of Early Diagnostic Biomarkers | Early detection can enable timely intervention and potentially delay or prevent the onset of debilitating symptoms, significantly improving quality of life. |
| Personalized Treatment Strategies | Tailoring treatment plans to individual genetic profiles and clinical characteristics could lead to more effective therapies and minimize adverse effects, increasing patient compliance. |
| Disease-Modifying Therapies | Preventing the accumulation of amyloid fibrils could halt or reverse the progression of the disease, leading to improved long-term outcomes and potentially a cure. |
| Investigating Preventive Measures | Identifying lifestyle modifications or therapies that target pathways implicated in disease development could potentially delay or prevent the onset of the disease, offering a preventative approach. |
| Improved Understanding of Disease Pathogenesis | Detailed knowledge of the disease’s intricate mechanisms will allow for the development of more effective and targeted treatments, leading to improved outcomes and potential breakthroughs in disease management. |
Concluding Remarks: Hattr Amyloidosis Life Expectancy
In conclusion, understanding HATTR amyloidosis life expectancy requires a multifaceted approach, considering the interplay of diagnosis, treatment, and individual factors. While challenges remain, ongoing research and advancements in treatment strategies offer hope for improved outcomes and enhanced quality of life for those facing this condition. This article serves as a resource for patients, families, and healthcare professionals, providing a deeper understanding of the complexities of HATTR amyloidosis.