Overview of chronic myeloid leukemia is a complex blood cancer, and understanding its intricacies is crucial for those affected and those seeking to learn more. This introduction will explore the various facets of CML, from its defining characteristics and underlying pathophysiology to the available treatment strategies and future research directions.
Chronic myeloid leukemia (CML) is a type of cancer affecting the blood-forming cells in the bone marrow. Characterized by the presence of the BCR-ABL1 fusion gene, CML progresses through distinct phases. Early symptoms can be subtle, making early diagnosis crucial. This overview will explore the different diagnostic methods, treatment options, and the long-term prognosis for patients with CML.
Introduction to Chronic Myeloid Leukemia (CML)

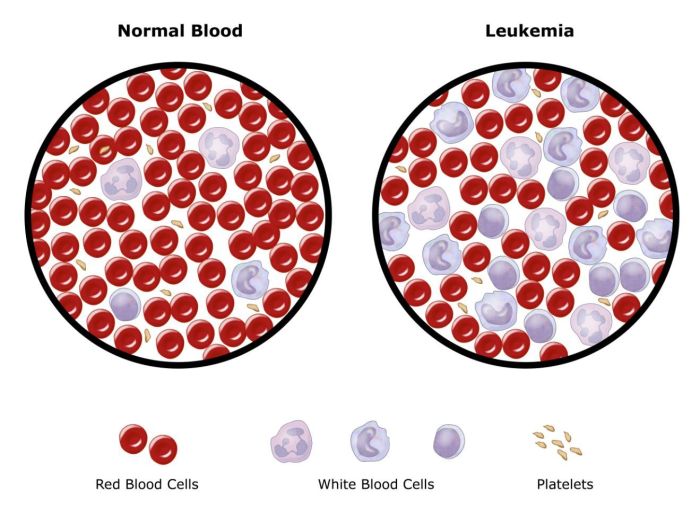
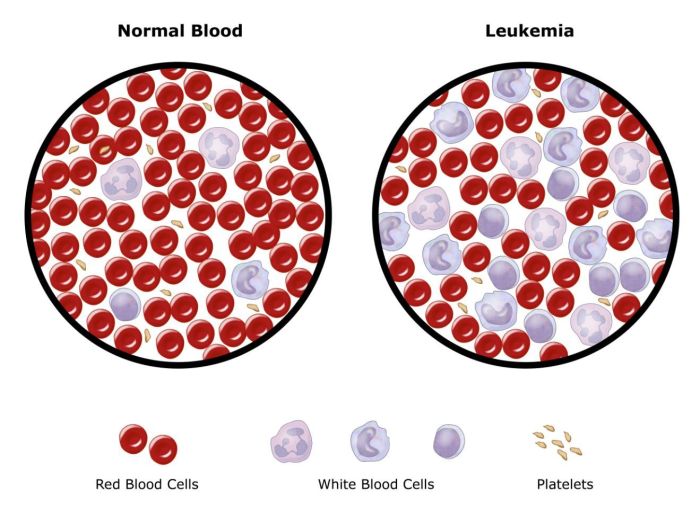
Chronic Myeloid Leukemia (CML) is a type of blood cancer characterized by the uncontrolled proliferation of myeloid cells in the bone marrow. These abnormal cells, instead of developing into healthy blood cells like red blood cells, white blood cells, and platelets, accumulate and crowd out the normal cells, leading to a variety of health complications. Understanding CML’s specific characteristics, symptoms, and prevalence is crucial for early diagnosis and effective treatment.
Key Characteristics of CML
CML is classified as a myeloproliferative neoplasm, a group of cancers arising from hematopoietic stem cells in the bone marrow. A defining feature is the presence of the Philadelphia chromosome, a unique chromosomal abnormality. This abnormality results from a reciprocal translocation between chromosomes 9 and 22, producing the BCR-ABL fusion gene. This fusion gene encodes an abnormal tyrosine kinase enzyme, driving the uncontrolled cell growth that characterizes CML.
Chronic myeloid leukemia (CML) is a type of blood cancer, and understanding its overview is crucial for effective management. While it’s important to research treatment options and preventative measures for CML, sometimes dealing with the side effects of treatments is more pressing. For example, if you experience diarrhea during treatment, it’s helpful to know how to make diarrhea go away here.
Ultimately, a comprehensive understanding of CML, its management, and potential side effects like diarrhea, is key for successful treatment and a better quality of life.
Typical Symptoms in Early Stages
In the early stages, CML often presents with nonspecific symptoms that may be easily mistaken for other conditions. Common symptoms include fatigue, weakness, and unexplained weight loss. Some patients may experience an enlarged spleen (splenomegaly), which can be felt as a fullness or discomfort in the left upper abdomen. Other potential symptoms include night sweats, fever, and bone pain.
It’s important to note that these symptoms can be subtle and often develop gradually, making early detection challenging.
Prevalence and Incidence Rates
The prevalence and incidence of CML vary geographically. While precise figures are difficult to pinpoint, CML is generally considered a relatively rare cancer compared to other blood cancers like acute myeloid leukemia. Data suggests a global incidence rate of approximately 1-2 cases per 100,000 people annually. Specific regional variations in incidence rates may exist but require further investigation based on detailed epidemiological studies.
Comparison of CML with Other Leukemia Types, Overview of chronic myeloid leukemia
| Characteristic | CML | Acute Myeloid Leukemia (AML) | Acute Lymphoblastic Leukemia (ALL) |
|---|---|---|---|
| Cell Type Affected | Myeloid cells | Myeloid cells | Lymphoid cells |
| Growth Rate | Slow | Rapid | Rapid |
| Philadelphia Chromosome | Often present (BCR-ABL fusion gene) | Rarely present | Rarely present |
| Symptoms | Often insidious, gradual onset | Rapid onset, often severe symptoms | Rapid onset, often severe symptoms |
| Prognosis | Generally more treatable in early stages with targeted therapies | Variable prognosis, depending on specific subtypes and patient factors | Variable prognosis, depending on specific subtypes and patient factors |
This table highlights key differences in cell type, growth rate, and characteristic features among various leukemia types. The presence of the Philadelphia chromosome and the slower growth rate are important diagnostic factors for CML differentiation. Furthermore, early diagnosis and targeted therapies play a critical role in improving outcomes for patients with CML.
Pathophysiology of CML
Chronic myeloid leukemia (CML) is a cancer of the blood characterized by the uncontrolled proliferation of myeloid cells. Understanding the underlying pathophysiology is crucial for developing effective treatment strategies. This involves delving into the molecular mechanisms driving the disease, the progression stages, and the role of signaling pathways in the disease’s development.The fundamental driver of CML is a specific genetic alteration: the BCR-ABL1 fusion gene.
This fusion, resulting from a reciprocal translocation between chromosomes 9 and 22, creates a new, oncogenic protein that disrupts normal cellular regulation and promotes uncontrolled cell growth. The resulting protein, p210 BCR-ABL1, has constitutive tyrosine kinase activity, leading to aberrant signaling cascades that contribute to the disease’s development and progression.
BCR-ABL1 Fusion Gene
The Philadelphia chromosome, a characteristic cytogenetic abnormality in CML, is directly linked to the BCR-ABL1 fusion gene. This fusion gene product, p210 BCR-ABL1, possesses enhanced tyrosine kinase activity compared to normal cellular proteins. This heightened activity triggers a cascade of downstream signaling events that promote cell proliferation, inhibit apoptosis (programmed cell death), and ultimately lead to the development of CML.
Importantly, the specific breakpoint in the BCR and ABL1 genes can influence the type of BCR-ABL1 fusion protein produced and the clinical behavior of the disease.
Stages of CML Progression
CML progresses through distinct phases, each with varying clinical features and treatment responses. These stages are crucial to understanding the disease’s evolution and guiding treatment decisions.
- Chronic Phase: In this initial phase, the disease is often asymptomatic or presents with mild symptoms. The bone marrow is primarily populated by immature myeloid cells, but the rate of proliferation is relatively controlled. Diagnosis in this phase is crucial, as early intervention can significantly impact long-term outcomes.
- Accelerated Phase: As the disease progresses, the bone marrow becomes increasingly infiltrated with abnormal cells, leading to a decline in normal blood cell counts. This phase is marked by the appearance of more immature cells in the blood and bone marrow. Symptoms worsen, and the patient becomes more susceptible to infections. The accelerated phase is characterized by increasing numbers of immature cells and the presence of additional genetic mutations.
- Blast Crisis Phase: In this advanced phase, the bone marrow is almost entirely replaced by immature blood cells (blasts). The uncontrolled proliferation of these blasts can lead to severe complications, including organ damage and bleeding. The blast crisis phase is often associated with the development of additional genetic abnormalities and represents a significant clinical challenge.
Signaling Pathways in CML Pathogenesis
The BCR-ABL1 fusion protein dysregulates numerous signaling pathways, most notably the RAS/MAPK and PI3K/AKT pathways. These pathways are crucial for normal cell growth and survival, but aberrant activation by BCR-ABL1 leads to their hyperactivation. This hyperactivation promotes uncontrolled cell proliferation, survival, and differentiation, further contributing to the disease process. Understanding these pathways is essential for developing targeted therapies that specifically inhibit the aberrant signaling.
Genetic Mutations in CML
Additional genetic abnormalities frequently arise during CML progression, further contributing to the complexity of the disease.
Chronic myeloid leukemia (CML) is a type of cancer that affects the blood-forming cells in the bone marrow. Understanding the various treatments, including targeted therapies, is crucial for managing the disease effectively. Often, patients battling CML also face sleep disruptions, and cognitive behavioral therapy for insomnia (CBT-I) what is cognitive behavioral therapy for insomnia cbti can be a helpful tool in improving sleep quality and overall well-being.
Fortunately, various strategies can alleviate symptoms and improve the quality of life for individuals living with CML. This highlights the interconnectedness of physical and mental health, particularly when facing a complex medical condition like CML.
| Mutation Type | Description |
|---|---|
| BCR-ABL1 mutations | Variations within the BCR-ABL1 fusion gene can impact the activity and function of the fusion protein. These mutations can affect the responsiveness to therapy and the clinical course of the disease. |
| Other chromosomal abnormalities | Additional chromosomal translocations, deletions, or amplifications can occur in CML, often in the accelerated and blast crisis phases. These mutations can further contribute to the uncontrolled cell proliferation and survival mechanisms. |
| Epigenetic modifications | Changes in gene expression without alterations to the DNA sequence. These modifications can impact the regulation of critical genes involved in cell growth and differentiation. |
Diagram of Key Molecular Events
[Imagine a diagram here depicting the BCR-ABL1 fusion gene, its interaction with downstream signaling pathways (RAS/MAPK, PI3K/AKT), and the resulting effects on cell proliferation and survival. The diagram would visually illustrate the cascade of events triggered by the fusion gene, highlighting the key molecular players and their interactions.]
Diagnosis and Staging of CML
Chronic myeloid leukemia (CML) diagnosis relies on a multi-faceted approach, combining various tests to identify the disease and determine its progression. Early detection is crucial for effective treatment and improved outcomes. This involves not only recognizing the characteristic features but also assessing the extent of the disease, a process known as staging.
Common Diagnostic Methods
Several methods are employed to diagnose CML, each contributing unique information to the overall picture. Blood tests, such as complete blood counts (CBCs), are frequently the first line of investigation. These tests assess the levels of different blood cells, including red blood cells, white blood cells, and platelets. Anomalies in these cell counts can be indicative of CML, but are not definitive.
Bone marrow biopsies provide a more direct assessment of the bone marrow’s cellular composition. A pathologist examines the tissue under a microscope to identify any unusual or cancerous cell growth.
Cytogenetic Analysis
Cytogenetic analysis is a cornerstone of CML diagnosis. This technique examines the chromosomes in cells, searching for structural abnormalities. In CML, a characteristic abnormality is the Philadelphia chromosome, a fusion of chromosomes 9 and 22. The presence of the Philadelphia chromosome is highly indicative of CML. The Philadelphia chromosome results in the production of the BCR-ABL1 fusion gene, a hallmark of the disease.
Molecular Testing
Molecular testing, including techniques like fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR), provides highly sensitive and specific detection of the BCR-ABL1 fusion gene. FISH utilizes fluorescent probes to visualize the fusion gene’s presence under a microscope. PCR amplifies the fusion gene’s DNA, allowing for its detection even in very low quantities. These methods are particularly valuable for detecting the BCR-ABL1 fusion gene in suspected cases or in monitoring treatment response.
Staging Systems
Staging systems, such as the Sokal and Hasford scoring systems, are used to estimate the prognosis and guide treatment strategies. These systems consider various clinical and laboratory factors, including age, white blood cell count, platelet count, and cytogenetic abnormalities. These factors are integrated into scores that provide a numerical estimate of the risk of disease progression and the potential need for more aggressive treatment approaches.
Summary of Diagnostic Criteria for Different Stages of CML
| Stage | Cytogenetics | Sokal Score | Hasford Score | Clinical Features |
|---|---|---|---|---|
| Chronic Phase (CP) | Philadelphia chromosome positive | Low | Low | Relatively stable disease; mild symptoms |
| Accelerated Phase (AP) | Presence of additional chromosomal abnormalities | Intermediate to High | Intermediate to High | Increasing symptoms; increased risk of complications |
| Blast Crisis (BC) | Significant increase in blast cells | High | High | Rapidly progressive disease; severe symptoms |
Note: The specific criteria for each stage can vary depending on the staging system used. These tables are a simplified representation of complex clinical criteria. Consultation with a healthcare professional is crucial for accurate diagnosis and staging. The table does not fully encompass all possible variables in assessing CML stages.
Treatment Strategies for CML
Chronic myeloid leukemia (CML) is a complex disease, but effective treatment strategies have significantly improved patient outcomes. Early diagnosis and appropriate intervention are crucial for managing the disease and achieving long-term remission. Modern treatments focus on controlling the uncontrolled cell growth, preventing progression to acute leukemia, and maintaining a good quality of life.Effective treatment options are now available, and many patients can achieve a long-term, comfortable remission.
These therapies are often tailored to the individual patient’s needs and the specific characteristics of their CML.
Tyrosine Kinase Inhibitors (TKIs)
Tyrosine kinase inhibitors (TKIs) are the cornerstone of modern CML treatment. They specifically target the BCR-ABL1 fusion protein, which is the driver of the disease. This targeted approach minimizes harm to healthy cells, maximizing efficacy and minimizing side effects compared to traditional chemotherapy.
Different Types of TKIs
Various TKIs are available, each with its own efficacy profile and side effect profile. Understanding the characteristics of each TKI is essential for selecting the most appropriate treatment for a particular patient.
Chronic myeloid leukemia (CML) is a type of cancer that affects the blood-forming cells in the bone marrow. While researching CML, I came across an inspiring story about Jordan Chiles and her work with Sanofi for T1D awareness jordan chiles sanofi t1d awareness. It’s amazing how different areas of health can intersect and highlight the importance of supporting research in areas like CML and other blood cancers.
- Imatinib (Gleevec): Imatinib was the first TKI approved for CML. It is generally well-tolerated and highly effective in achieving remission in most patients. Its broad effectiveness and relatively low side effect profile make it a primary choice for initial treatment.
- Dasatinib (Sprycel): Dasatinib is a second-generation TKI, known for its strong activity against BCR-ABL1 mutations that may be resistant to imatinib. It is often used for patients who have failed or are intolerant to imatinib. Its stronger activity may lead to a higher incidence of side effects.
- Nilotinib (Tasigna): Similar to dasatinib, nilotinib is also a second-generation TKI with high potency and efficacy. It has been shown to be effective in patients who have developed resistance to imatinib. Side effect profiles are comparable to dasatinib.
- Bosutinib (Bosulif): Bosutinib is a third-generation TKI with broad spectrum activity. It can be effective in patients who have failed other TKIs. Its effectiveness comes with a potentially higher risk of side effects compared to imatinib.
- Ponatinib (Iclusig): Ponatinib is a potent TKI specifically designed to target resistant mutations. Its high efficacy against resistant forms of CML makes it a crucial treatment option for patients with specific genetic markers. However, it comes with a higher risk of serious side effects, including cardiovascular issues and dental problems.
Efficacy and Side Effects Comparison
The efficacy of TKIs varies, with some being more potent than others. Side effects also differ, ranging from mild gastrointestinal issues to more serious cardiovascular or dermatological problems. The choice of TKI is tailored to individual patient needs, considering their specific CML characteristics, potential for resistance, and tolerance to side effects. A doctor’s careful assessment and monitoring are crucial to ensure the best possible outcome.
Targeted Therapies in CML Treatment
Targeted therapies, particularly TKIs, are crucial in CML treatment due to their ability to specifically target the BCR-ABL1 fusion protein. This approach allows for more precise treatment, potentially minimizing harm to healthy cells compared to traditional chemotherapy. This targeted approach is a significant advancement in cancer treatment.
Treatment Strategies for Different CML Stages
The treatment strategy for CML is tailored to the specific stage of the disease.
- Chronic Phase (CP): In the chronic phase, the disease is often effectively managed with TKIs, aiming to achieve molecular remission. Close monitoring and adjustments to treatment plans are critical to prevent progression.
- Accelerated Phase (AP): In the accelerated phase, the treatment strategy often shifts to more potent TKIs or combinations of therapies, along with supportive care. The focus is on controlling disease progression and improving quality of life.
- Blast Crisis (BC): In the blast crisis, treatment becomes more complex and intensive, often involving combinations of chemotherapy and targeted therapies, along with supportive care to manage the complications of advanced disease.
Summary Table of TKIs
| TKI | Generation | Mechanism of Action | Efficacy | Side Effects | Usage |
|---|---|---|---|---|---|
| Imatinib | First | Inhibits BCR-ABL1 tyrosine kinase | High | Generally low | First-line treatment |
| Dasatinib | Second | Inhibits BCR-ABL1 tyrosine kinase | High | Potentially higher | Second-line or resistant cases |
| Nilotinib | Second | Inhibits BCR-ABL1 tyrosine kinase | High | Potentially higher | Second-line or resistant cases |
| Bosutinib | Third | Inhibits BCR-ABL1 tyrosine kinase | High | Potentially higher | Resistant cases or after other TKIs |
| Ponatinib | Third | Inhibits BCR-ABL1 tyrosine kinase, including resistant mutations | High (for resistant cases) | High risk of serious side effects | Highly resistant cases |
Prognosis and Patient Management: Overview Of Chronic Myeloid Leukemia
Chronic myeloid leukemia (CML) has significantly improved prognosis with effective treatment, shifting from a fatal disease to a manageable condition for many patients. The long-term outlook for those undergoing successful treatment is generally positive, allowing for a good quality of life. However, diligent monitoring and adherence to treatment are crucial for maintaining remission and preventing relapse.
Long-Term Prognosis for CML Patients
The prognosis for CML patients undergoing effective treatment has dramatically improved. Early diagnosis and timely intervention with tyrosine kinase inhibitors (TKIs) are critical factors in achieving long-term remission. Studies have shown that patients who achieve and maintain molecular remission, a state where the leukemia-causing genetic abnormality is undetectable, have a very good long-term outlook. These patients can often lead fulfilling lives, comparable to those without the disease, though long-term effects of TKIs should be considered.
The specific prognosis depends on factors such as the type and duration of treatment, individual patient response, and adherence to the treatment regimen.
Importance of Regular Monitoring and Follow-up
Regular monitoring is essential for CML patients to detect any signs of disease progression or treatment resistance early. This includes regular blood tests, genetic assessments, and physical examinations. Early detection of relapse allows for prompt intervention, potentially preventing the need for more aggressive treatments. Close monitoring allows for adjustments to treatment plans as needed, ensuring the best possible outcomes.
Role of Supportive Care and Patient Education
Supportive care plays a vital role in managing CML. This includes addressing the physical, emotional, and psychological effects of the disease and its treatment. Patient education is crucial for empowering patients to actively participate in their care. Understanding the disease, treatment options, and potential side effects allows for informed decision-making and better adherence to the treatment plan.
This education can also alleviate anxieties and improve the patient’s overall well-being. Support groups and counseling services can provide invaluable emotional support and coping strategies for patients and their families.
Importance of Adherence to Treatment Regimens
Adherence to the prescribed treatment regimen is paramount for optimal outcomes in CML. Consistent medication intake, as directed by the healthcare provider, is essential for maintaining remission and preventing relapse. Understanding the importance of adhering to the treatment plan is key for long-term success. Missed doses or inconsistent treatment can lead to disease progression and treatment resistance.
Patient Support Resources
Numerous patient support resources are available for individuals diagnosed with CML. These resources provide valuable information, emotional support, and a sense of community. Online forums, support groups, and patient advocacy organizations offer opportunities to connect with others facing similar challenges. These resources provide a network of understanding and encouragement, reducing feelings of isolation and promoting active participation in managing the disease.
Healthcare providers can also direct patients to appropriate support systems. Local support groups or online forums can offer practical advice, emotional support, and a sense of community for patients and their families.
Research and Future Directions

Chronic myeloid leukemia (CML) research is a dynamic field, constantly evolving with new discoveries and advancements. Scientists are actively pursuing innovative strategies to improve treatment efficacy, minimize side effects, and ultimately achieve a cure for CML. This involves exploring various approaches, from refining existing therapies to developing entirely new treatment modalities.
Current Research Efforts
Current research efforts in CML are multifaceted and encompass several key areas. Scientists are refining existing tyrosine kinase inhibitors (TKIs) to enhance their effectiveness and reduce resistance development. They are also exploring new targeted therapies, including those that inhibit other pathways implicated in CML pathogenesis. These efforts are aimed at improving treatment outcomes, particularly for patients who develop resistance to current TKIs.
The focus is on personalized medicine approaches to tailor treatments to individual patient needs.
Potential Future Directions
Future research in CML holds promising avenues, including the development of novel therapies and preventive strategies. Immunotherapy, a rapidly advancing field, is showing significant potential in cancer treatment. Strategies combining immunotherapy with targeted therapies could enhance the efficacy of CML treatment and potentially eliminate the disease in a more complete way. Research into stem cell transplantation and gene editing technologies, like CRISPR, are also actively being explored, with the aim of permanently correcting the genetic defect responsible for CML.
Another important area of research is identifying biomarkers to predict treatment response and resistance, allowing for earlier and more targeted interventions.
Clinical Trials in CML Research
Clinical trials are crucial for evaluating the safety and efficacy of new treatments and strategies in CML. These trials rigorously assess the impact of novel therapies on patient outcomes, comparing them to existing standards of care. The data gathered from these trials provide critical evidence for regulatory approvals and inform treatment guidelines. For example, the development of TKIs, such as imatinib, was significantly aided by the results from well-designed clinical trials.
By participating in these trials, patients contribute directly to advancing knowledge and improving the lives of future CML patients.
Challenges and Opportunities in CML Research
Despite significant progress, CML research faces challenges. One major obstacle is the development of resistance to TKIs. Another challenge is the need for more effective and less toxic therapies for patients who cannot tolerate existing treatments. However, the field also presents significant opportunities. The ongoing development of new targeted therapies, combined with advances in genomic analysis and personalized medicine, promises to refine treatment approaches and improve outcomes for patients with CML.
The potential for immunotherapy and gene editing technologies further expands the horizon for innovative solutions.
Promising Areas of Research (e.g., Immunotherapy)
Immunotherapy holds substantial promise in CML treatment. Research is focusing on strategies to enhance the body’s immune response against CML cells. One area of investigation involves harnessing the power of T-cells to target and destroy cancerous cells. Preclinical studies suggest that combining immunotherapy with existing TKIs might synergistically enhance treatment efficacy. This approach could lead to more complete remission and potentially prevent the recurrence of the disease.
Moreover, research into immune checkpoint inhibitors could unlock further avenues for immunotherapy in CML.
Ending Remarks
In conclusion, overview of chronic myeloid leukemia presents a significant challenge, but significant progress has been made in understanding and treating this disease. From the initial diagnosis to the latest treatment options, this overview highlights the complexity of CML and the importance of ongoing research. The future holds promise for further advancements in treatment and improved outcomes for patients.


/leukemia-myeloid-250x-at-35mm-this-type-of-leukemia-has-its-origin-in-the-bone-marrow-myeloid-tissue-it-involves-a-malignant-proliferation-of-immature-white-blood-cells-this-action-can-crowd-out-production-of-rbc-s-and-platelets-leading-to-an--58aca68c3df78c345b81d051.jpg?w=700)
