Pain in back of knee when walking can be debilitating, impacting daily activities and overall well-being. This comprehensive guide delves into the various potential causes, from simple muscle strains to more complex conditions, offering insights into diagnosis, treatment, and prevention strategies.
We’ll explore the anatomy of the knee, differentiating between different types of pain, and examine potential underlying conditions that could be causing the discomfort. The discussion will also cover crucial diagnostic methods, including physical exams, imaging tests, and patient history, to help determine the root cause. Furthermore, we’ll discuss various treatment options, ranging from conservative approaches to surgical interventions, and highlight the importance of preventive measures for long-term knee health.
Defining the Problem
Knee pain, particularly in the back of the knee, can be a debilitating condition, often interfering with everyday activities like walking. Understanding the specific nature of this pain, its potential causes, and how it differs from other knee issues is crucial for effective diagnosis and treatment. This detailed exploration will help you better comprehend the various factors contributing to posterior knee pain during ambulation.Pain behind the knee when walking can stem from a multitude of issues affecting different anatomical structures.
It’s important to differentiate between various types of pain in this area. This can range from sharp, stabbing sensations to a dull, aching discomfort, which may intensify with certain movements. The location and intensity of the pain, as well as the accompanying symptoms, offer valuable clues to the underlying cause.
Types of Posterior Knee Pain
The back of the knee houses several crucial structures, and pain here can be indicative of issues affecting any of them. Tendinitis, bursitis, and meniscus tears are among the potential culprits. Ligament sprains or tears, particularly of the posterolateral corner of the knee, can also cause discomfort in the posterior region.
Potential Causes of Pain Behind the Knee During Walking
Various anatomical structures in the back of the knee can be sources of pain during walking. The popliteal fossa, a deep hollow behind the knee, houses important vessels and nerves. Inflammation of the structures within this fossa, such as the popliteal artery or vein, can lead to pain. Additionally, problems with the hamstring tendons, Baker’s cysts, or arthritis in the knee joint itself can also cause discomfort.
That nagging pain in the back of my knee when I walk? It’s definitely something I’ve been struggling with lately. While I’m trying to figure out the cause, I’ve been doing some research, and it’s important to know that certain health disparities exist, like increased risk factors for HIV in Black men. Understanding these risks, and accessing resources like those available at hiv in black men increased risk facts testing resources , is crucial for overall well-being.
Hopefully, addressing this knee pain isn’t connected to any underlying health concerns. I’m just hoping to find a solution soon.
A thorough assessment by a medical professional is crucial to pinpoint the precise cause.
Symptoms and Comparison to Other Knee Ailments
Pain behind the knee during walking should be distinguished from other knee problems. For instance, patellofemoral pain syndrome (runner’s knee) typically manifests as pain around the kneecap, while meniscus tears often present with locking or catching sensations. Anterior knee pain, or pain in the front of the knee, is frequently associated with patellar tracking issues or chondromalacia patellae.
Careful observation of the specific characteristics of the pain, such as its location, intensity, and triggering activities, is essential for differentiating it from other knee conditions.
Possible Diagnoses
The following table Artikels potential diagnoses for pain in the back of the knee during walking, along with associated symptoms, locations, and severity levels. Note that this is not an exhaustive list and individual experiences can vary significantly.
| Diagnosis | Symptoms | Location | Severity |
|---|---|---|---|
| Popliteal Tendinopathy | Sharp, stabbing pain, especially with resisted knee flexion, pain may radiate to the lower leg | Back of knee, along the tendon | Moderate to severe |
| Baker’s Cyst | Aching, dull pain, swelling, a palpable mass in the popliteal fossa | Popliteal fossa | Mild to moderate |
| Meniscus Tear | Sharp, sudden pain, locking or catching sensation, swelling | Medial or lateral aspects of the knee | Moderate to severe |
| Posterior Cruciate Ligament (PCL) Injury | Pain, instability, and giving way sensations, especially with twisting or pivoting movements | Back of the knee, particularly around the PCL | Moderate to severe |
| Arthritis | Aching, dull pain, stiffness, especially in the morning or after periods of inactivity, swelling | Entire knee joint, including the back | Mild to severe |
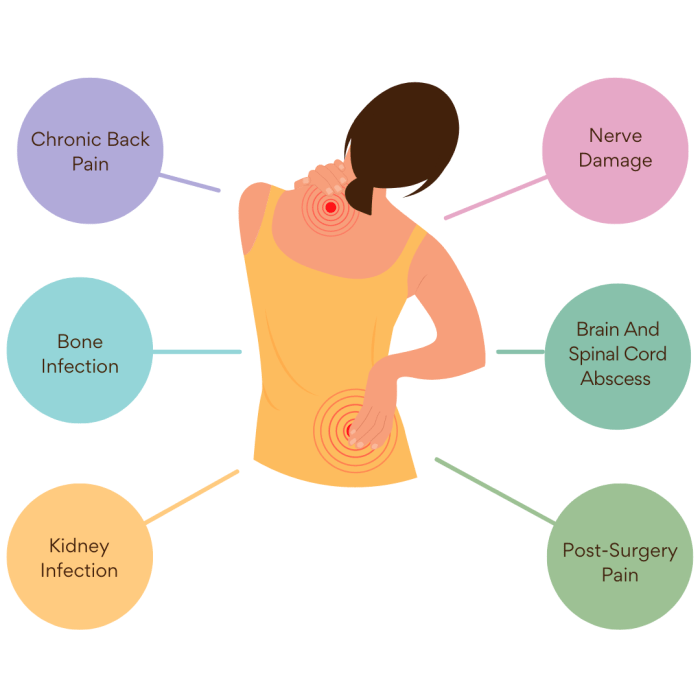
Possible Underlying Conditions
Knee pain, particularly in the back, when walking, can stem from a multitude of sources. Pinpointing the precise cause requires careful consideration of various factors, including lifestyle, medical history, and the specific nature of the pain. This section delves into potential underlying conditions, ranging from common soft tissue injuries to more complex medical issues.Understanding the possible causes of this pain is crucial for effective diagnosis and treatment.
Identifying the root problem allows for targeted interventions, maximizing the chances of a successful recovery and preventing future complications.
Muscle Strains, Sprains, and Soft Tissue Injuries
Muscle strains, often resulting from overuse or sudden movements, can lead to pain in the back of the knee. Similarly, sprains, which involve damage to ligaments, can also cause localized pain and tenderness. Other soft tissue injuries, such as tendinitis or bursitis, can contribute to discomfort in this area, particularly during activities like walking. The pain may be accompanied by swelling, bruising, or limited range of motion.
Joint Conditions: Arthritis and Bursitis
Arthritis, a broad term encompassing various inflammatory conditions affecting joints, can cause pain and stiffness in the knee, often exacerbated by movement. Osteoarthritis, a common form of arthritis, typically develops with age and involves the breakdown of cartilage within the joint. Rheumatoid arthritis is an autoimmune disease that can also impact the knee. Bursitis, inflammation of the bursae (fluid-filled sacs cushioning the joints), can lead to localized pain and tenderness, particularly in the back of the knee.
These conditions can make walking challenging and painful.
Neurological Issues
Neurological conditions, such as nerve compression or sciatica, can sometimes manifest as pain radiating down the back of the leg and into the knee. Nerve impingement can result from various factors, including herniated discs in the spine. The pain may be accompanied by numbness, tingling, or weakness in the affected leg. Proper neurological evaluation is crucial for differentiating these conditions from other potential causes of knee pain.
Table of Potential Conditions, Pain in back of knee when walking
| Condition | Possible Causes | Risk Factors | Symptoms |
|---|---|---|---|
| Muscle Strain | Overexertion, sudden movements, improper warm-up | Prior injury, poor flexibility, repetitive stress | Localized pain, tenderness, swelling, limited range of motion |
| Ligament Sprain | Trauma, sudden twisting or impact | Previous knee injury, weak muscles, improper footwear | Pain, instability, swelling, bruising, difficulty bearing weight |
| Tendinitis | Repetitive stress, overuse | Inadequate rest, improper technique, certain sports | Pain, tenderness, stiffness around the affected tendon, increased pain with activity |
| Osteoarthritis | Cartilage breakdown, aging | Genetics, obesity, joint overuse | Pain, stiffness, creaking, limited range of motion, pain worsening with activity |
| Rheumatoid Arthritis | Autoimmune response | Family history, certain infections | Pain, swelling, stiffness, fatigue, potentially affecting other joints |
| Bursitis | Repetitive stress, direct impact, infection | Previous knee injury, prolonged kneeling, certain medical conditions | Pain, swelling, tenderness over the affected bursa, increased pain with pressure |
| Nerve Compression | Herniated discs, spinal stenosis, tumors | Age, repetitive movements, certain occupations | Pain radiating down the leg, numbness, tingling, weakness, possible loss of reflexes |
Assessment and Diagnosis
Figuring out the precise cause of knee pain behind the kneecap during walking requires a methodical approach. This involves a comprehensive evaluation, combining patient history, physical examination, and potentially, diagnostic imaging. The goal is to pinpoint the underlying issue and guide appropriate treatment.The diagnostic process for knee pain isn’t a simple one-size-fits-all approach. It hinges on a thorough understanding of the patient’s individual situation.
A detailed history of symptoms, lifestyle factors, and any prior injuries significantly impacts the diagnostic path.
Physical Examinations and Tests
A crucial first step is a thorough physical examination. This involves palpating (feeling) the affected area to identify tenderness, swelling, or any unusual warmth. Range of motion tests assess the joint’s flexibility and potential limitations. Specific tests, such as the McMurray test (for meniscus tears) or the Thessaly test (for instability), help pinpoint potential issues within the knee joint.
These tests are vital in identifying the source of pain and any associated impairments. Muscle strength and reflexes are also evaluated to ascertain if nerve impingement or muscular imbalances contribute to the problem.
Medical Imaging
Diagnostic imaging plays a pivotal role in evaluating the knee. X-rays are frequently the initial imaging modality. They provide a clear view of the bones, revealing any fractures, dislocations, or significant bone abnormalities. If bone-related issues are ruled out, or if a more detailed soft tissue analysis is needed, magnetic resonance imaging (MRI) might be employed. MRI provides detailed images of soft tissues, such as cartilage, ligaments, and tendons, enabling identification of tears, strains, or other soft tissue injuries.
Ultrasound (US) can also be a useful tool, particularly in evaluating soft tissues and fluid collections. The choice of imaging method depends on the suspected cause of the pain and the clinical findings.
Patient History and Lifestyle Factors
Understanding the patient’s medical history, including past injuries, surgeries, and chronic conditions, is essential. A detailed account of symptoms (e.g., when the pain started, how it feels, what activities worsen or alleviate it) aids in narrowing down potential diagnoses. Lifestyle factors, such as exercise routines, occupation, and any repetitive movements, can significantly influence the development of knee pain.
For instance, runners might experience patellofemoral pain syndrome due to repetitive stress on the kneecap.
Diagnostic Tools and Applications
| Diagnostic Tool | Procedure | Limitations | Typical Results |
|---|---|---|---|
| X-ray | A short-duration procedure using ionizing radiation to produce images of the bones. | Limited ability to visualize soft tissues; exposure to radiation. | Reveals fractures, dislocations, and significant bone abnormalities. |
| MRI | Uses a strong magnetic field and radio waves to create detailed images of soft tissues. | Can be expensive; may not be suitable for individuals with metal implants; can be time-consuming. | Detailed visualization of cartilage, ligaments, tendons, and soft tissues, revealing tears, strains, or other soft tissue injuries. |
| Physical Examination | Assessment of the knee joint by palpation, range of motion tests, and specific tests like McMurray’s test. | Subjectivity in interpretation; may not always identify subtle injuries. | Identification of tenderness, swelling, limited range of motion, and potential structural issues. |
| Patient History | Detailed discussion with the patient about symptoms, activities that trigger or relieve pain, and medical history. | Reliance on patient recall; potential for misinterpretation of symptoms. | Provides valuable insights into the nature and progression of the pain, enabling the identification of potential causes. |
Treatment Options: Pain In Back Of Knee When Walking
Dealing with pain in the back of the knee when walking can be frustrating, but effective treatment options exist. This section explores conservative and surgical approaches, along with the critical role of physical therapy and lifestyle modifications. Understanding these options empowers you to work with your healthcare provider to develop a personalized treatment plan.
Conservative Treatment Options
Conservative treatments aim to alleviate symptoms without surgery. These methods often involve a phased approach, starting with simpler measures and progressing to more intensive strategies if needed.
- Rest and Ice Application:
- Over-the-Counter Pain Relievers:
- Bracing and Support:
- Physical Therapy:
- Injections:
Minimizing activities that exacerbate pain, combined with regular icing, can help reduce inflammation and swelling. Rest periods should be tailored to individual needs and activity levels. Apply ice packs for 15-20 minutes at a time, several times a day, avoiding direct skin contact.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help manage pain and inflammation. Always follow the dosage instructions on the label and consult a doctor if symptoms persist or worsen.
Wearing a knee brace can provide support and stability, reducing stress on the affected area. A doctor or physical therapist can recommend the appropriate type and fit of brace.
A physical therapist can design an exercise program tailored to address the specific cause of the pain. This often involves stretching, strengthening exercises, and improving range of motion. Examples of exercises include hamstring stretches, quadriceps strengthening, and balance exercises.
Corticosteroid injections can reduce inflammation and pain. However, they are typically used as a short-term solution and should be considered in conjunction with other treatments. Their effectiveness and potential side effects should be discussed with a healthcare provider.
Surgical Interventions
In cases where conservative treatments fail to provide significant relief, surgical intervention might be considered. The specific surgical approach depends on the underlying condition.
- Arthroscopy:
- Meniscus Repair or Removal:
- Ligament Reconstruction:
This minimally invasive procedure allows surgeons to visualize and treat damaged knee structures, such as cartilage or ligaments, using small incisions. It’s often used to repair meniscus tears or remove loose fragments.
Experiencing pain in the back of your knee when walking can be frustrating. It’s often tricky to pinpoint the exact cause, but sometimes, it’s related to underlying digestive issues. For example, conditions like Irritable Bowel Syndrome (IBS) can sometimes manifest in unexpected ways, and medications like Bentyl, which you can learn more about in this helpful overview bentyl for ibs an overview , might be a factor.
So, if you’re dealing with this knee pain, it’s always best to consult a doctor to get a proper diagnosis and treatment plan.
If a meniscus tear is severe and interferes with function, surgical repair or removal might be necessary. Repair is preferred when possible, as it preserves the meniscus’s function.
My knee’s been acting up lately – sharp pain in the back when I walk. It’s a real bummer, and I’ve been trying to figure out what’s causing it. While researching, I stumbled upon some interesting info about how to get rid of stretch marks how to get rid of stretch marks , which got me thinking.
Maybe some of those tips could help with my knee pain too, if it’s related to any underlying issues. I’m going to keep researching and try some different things, though I’m hoping to find a solution soon so I can get back to my normal activities.
Severe ligament tears, such as an anterior cruciate ligament (ACL) tear, may require surgical reconstruction to restore stability. This involves replacing the damaged ligament with a graft from another part of the body or a synthetic material.
Role of Physical Therapy and Rehabilitation
Physical therapy plays a vital role in both conservative and post-surgical treatment. A personalized rehabilitation program is essential for regaining strength, flexibility, and function.
- Post-Surgical Rehabilitation:
- Conservative Rehabilitation:
After surgery, physical therapy helps patients regain strength and range of motion in the knee. This typically involves a gradual increase in exercise intensity and activity levels, under the guidance of a therapist.
Even without surgery, physical therapy can be instrumental in managing and alleviating pain. It focuses on strengthening supporting muscles and improving flexibility to prevent further injury and promote recovery.
Lifestyle Modifications
Adopting certain lifestyle changes can complement medical interventions and contribute to long-term recovery.
- Weight Management:
- Proper Footwear:
- Gradual Progression of Activities:
Maintaining a healthy weight reduces stress on the knee joints. Weight loss, if appropriate, can be a crucial factor in managing knee pain.
Wearing supportive shoes with proper cushioning can reduce the impact on the knee joint during walking or running.
Gradually increasing activity levels, avoiding sudden bursts of activity, and listening to the body’s signals are vital for preventing further injury.
Treatment Comparison Table
| Treatment Method | Description | Effectiveness | Potential Side Effects |
|---|---|---|---|
| Rest and Ice | Minimizing activity and applying ice to reduce inflammation. | Generally effective for mild to moderate pain. | Minimal, potential for discomfort. |
| NSAIDs | Over-the-counter pain relievers. | Effective for pain and inflammation. | Gastrointestinal issues, kidney problems (in high doses or long-term use). |
| Bracing | Provides support and stability to the knee. | Can be helpful for mild to moderate instability. | Skin irritation, discomfort, potential for incorrect fit. |
| Physical Therapy | Tailored exercises to strengthen and stretch the knee. | Highly effective for long-term pain management and function. | Muscle soreness, potential for minor discomfort during exercises. |
| Corticosteroid Injections | Reduces inflammation and pain. | Short-term relief, potentially effective. | Infection, skin reactions, cartilage damage (rare). |
| Arthroscopy | Minimally invasive procedure to treat knee structures. | Effective for many conditions, potentially preserving the knee. | Risk of infection, bleeding, nerve damage (rare). |
| Meniscus Repair/Removal | Surgical intervention for meniscus tears. | Effective in relieving pain and restoring function. | Risk of infection, complications during surgery (rare). |
| Ligament Reconstruction | Surgical repair or replacement of damaged ligaments. | Restores knee stability, crucial for high-impact activities. | Risk of infection, complications during surgery, potential for graft failure. |
Prevention Strategies
Knee pain, particularly in the back, can be a frustrating and debilitating issue, especially when walking. Understanding the contributing factors and implementing proactive measures can significantly reduce your risk of experiencing this discomfort. By focusing on preventative strategies, you can actively manage your knee health and maintain a more comfortable and active lifestyle.Preventing pain in the back of the knee during walking involves addressing several key areas, including proper warm-up and cool-down routines, appropriate footwear, maintaining a healthy weight, and engaging in regular stretching and strengthening exercises.
By prioritizing these preventative measures, you can substantially reduce the likelihood of developing or exacerbating existing knee pain.
Proper Warm-up and Cool-down Routines
Effective warm-up and cool-down routines are crucial for preparing your body for physical activity and promoting recovery afterward. A proper warm-up gradually increases blood flow to the muscles, improving flexibility and range of motion. This reduces the risk of strains and tears. Conversely, a cool-down period allows your body to gradually return to its resting state, aiding in the removal of metabolic waste products and reducing muscle soreness.
This preventative approach is essential for long-term knee health.
Appropriate Footwear and Support
Choosing the right footwear is paramount for knee health. Supportive shoes with adequate cushioning and arch support can help absorb impact and distribute pressure evenly across the foot and lower leg. This can help prevent excessive stress on the knee joint, particularly during walking. Properly fitted shoes that align with your foot type are vital for optimal support.
Consider consulting with a podiatrist for personalized recommendations.
Maintaining a Healthy Weight
Maintaining a healthy weight significantly reduces stress on the knee joint. Excess weight puts additional pressure on the cartilage and ligaments, increasing the risk of injury and pain. Even a moderate weight loss can make a substantial difference in alleviating knee pain and preventing future issues. Studies consistently demonstrate a correlation between weight management and reduced knee pain.
Stretching and Strengthening Exercises for Leg Muscles
Regular stretching and strengthening exercises for leg muscles are essential for maintaining knee stability and flexibility. Strengthening exercises, such as hamstring curls and quadriceps stretches, improve muscle support around the knee joint, thereby reducing the risk of injury. Stretching exercises, like calf stretches and hamstring stretches, increase flexibility, allowing for a wider range of motion and preventing stiffness.
Incorporating these exercises into your routine can significantly reduce the likelihood of experiencing knee pain during walking.
Examples of Preventative Measures and their Effectiveness
A consistent warm-up routine, such as light cardio and dynamic stretches, can significantly improve joint flexibility and blood flow, decreasing the risk of injuries during walking. Proper footwear with adequate cushioning and arch support can lessen the impact on the knee joint, reducing stress and potential pain. Maintaining a healthy weight is crucial; a 10-pound weight loss can translate to a 25-30% reduction in knee joint stress.
Regular stretching, focusing on hamstring and quadriceps stretches, can improve knee flexibility and stability, lessening the risk of pain. Strengthening exercises, like calf raises and lunges, build muscle strength around the knee, enhancing stability and protection against injury. These preventative measures, when implemented consistently, contribute to a healthier, more active lifestyle, minimizing the likelihood of knee pain during walking.
Illustrative Cases
Understanding the complexities of back-of-the-knee pain during walking requires exploring real-world examples. These cases highlight the diagnostic process, treatment approaches, and outcomes, providing valuable insights into managing this condition effectively. The specific circumstances of each patient significantly influence the course of treatment and prognosis.
Case Study 1: Patellofemoral Pain Syndrome
This case involved a 28-year-old female runner experiencing sharp, intermittent pain in the back of her knee, worsening with prolonged walking or running. Physical examination revealed tenderness around the patellar region and a slight patellar tracking abnormality. The patient reported a history of recent increases in training intensity.
Diagnosis: Patellofemoral pain syndrome (PFPS) was suspected based on the patient’s history, physical examination findings, and the characteristic location of pain. A clinical diagnosis was confirmed through a combination of patient history, physical examination, and exclusion of other conditions.
Treatment Approach: Treatment focused on reducing pain and inflammation. Initial management included rest, ice, compression, and elevation (RICE). Physical therapy exercises targeting quadriceps strengthening, hamstring flexibility, and patellar tracking were prescribed. The patient was also advised on appropriate footwear and running form to prevent further injury. She was also advised to gradually increase her training load over time to avoid overloading the knee joint.
Outcomes and Lessons Learned: The patient responded well to the conservative treatment approach, experiencing significant pain reduction within 6 weeks. The case highlights the importance of considering overuse injuries, particularly in athletes, and the effectiveness of targeted physical therapy in managing PFPS. Proactive measures like gradual training progression are crucial in preventing recurring episodes.
Anatomical Structures Related to Patellofemoral Pain Syndrome
The patellofemoral joint, formed by the patella (kneecap) and the femur (thigh bone), plays a crucial role in knee extension and flexion. The surrounding muscles, including the quadriceps femoris, hamstrings, and various supporting ligaments, are essential for maintaining knee stability. Dysfunction in any of these structures can lead to pain. This case study specifically focuses on the patellar tracking mechanism and the potential for malalignment or irritation causing pain.

(Image Description: A labeled diagram of the knee joint. The patella, femur, and key ligaments are highlighted, emphasizing the patellofemoral joint’s structure and the surrounding soft tissues. Pointers to areas prone to irritation and inflammation in PFPS are indicated.)
Importance of a Patient-Centered Approach
A patient-centered approach involves understanding the individual patient’s circumstances, lifestyle, and expectations. This means considering factors like the patient’s occupation, hobbies, and goals when developing a treatment plan. For example, a runner might require a different treatment plan than a sedentary office worker. Active patient participation and communication are vital to achieving successful outcomes. By actively listening to the patient’s concerns and actively involving them in the decision-making process, healthcare professionals can tailor the treatment to meet their specific needs and promote adherence.
End of Discussion
Understanding pain in the back of the knee when walking requires a multi-faceted approach, considering potential anatomical structures, underlying conditions, and appropriate diagnostic methods. This guide offers a structured overview of the problem, from its origins to possible solutions. Remember, seeking professional medical advice is crucial for accurate diagnosis and tailored treatment plans. By combining self-care measures with expert guidance, you can effectively manage and prevent this discomfort.