How to keep kidneys healthy is a crucial aspect of overall well-being. Your kidneys are vital organs responsible for filtering waste and maintaining fluid balance in your body. This guide dives deep into the essential aspects of kidney health, offering practical advice and actionable steps you can take today. We’ll explore dietary recommendations, hydration strategies, the role of exercise, managing medical conditions, and lifestyle choices to promote optimal kidney function.
From understanding the importance of a kidney-friendly diet to managing chronic conditions like diabetes and high blood pressure, this guide will provide you with the knowledge and tools you need to protect your kidneys. We’ll delve into specific foods, hydration levels, and exercise routines to help you make informed decisions for long-term kidney health.
Diet and Nutrition
A healthy diet is crucial for managing kidney health, particularly as kidney function declines. Proper nutrition helps control blood pressure, blood sugar, and other factors that can strain the kidneys. A kidney-friendly diet focuses on specific nutrients and food groups to support optimal kidney function and minimize the risk of further damage.A balanced diet, tailored to individual needs and the stage of kidney disease, can significantly impact kidney health.
The dietary approach emphasizes reducing sodium, potassium, phosphorus, and protein intake, while ensuring adequate intake of essential nutrients. This tailored approach prevents the build-up of harmful substances in the blood, which can further damage the kidneys.
Foods to Include in a Kidney-Friendly Diet
A kidney-friendly diet incorporates a variety of nutrient-rich foods. This approach ensures the body receives the necessary vitamins, minerals, and antioxidants while minimizing the burden on the kidneys.
Staying hydrated and eating a balanced diet are key for healthy kidneys. However, it’s also important to consider the crucial role of proper medical care, especially when it comes to conditions like asthma. Finding the right doctor for your specific asthma needs is just as vital as maintaining a healthy lifestyle for your kidneys. For more insights on different types of asthma doctors and how to choose the best one for your needs, check out this helpful guide: types of asthma doctors and choosing the best one.
Ultimately, a holistic approach combining healthy habits and expert medical guidance is the best way to keep your kidneys in top shape.
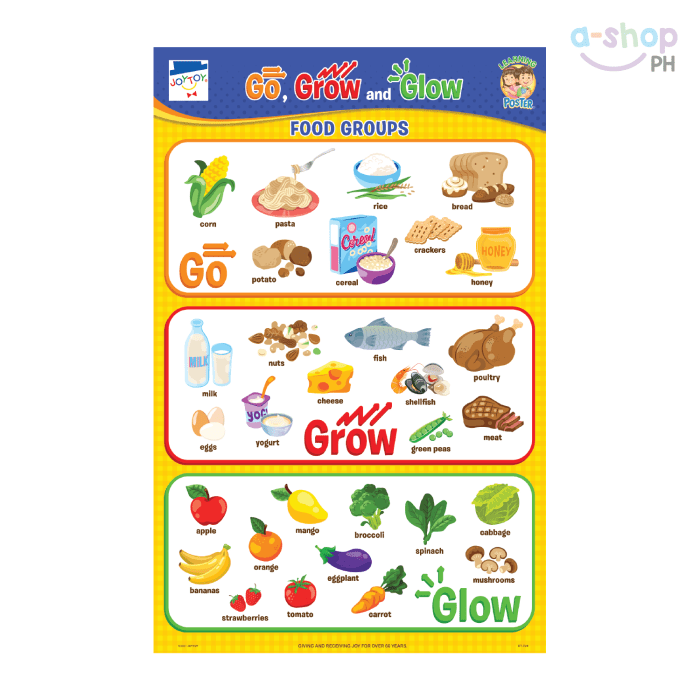
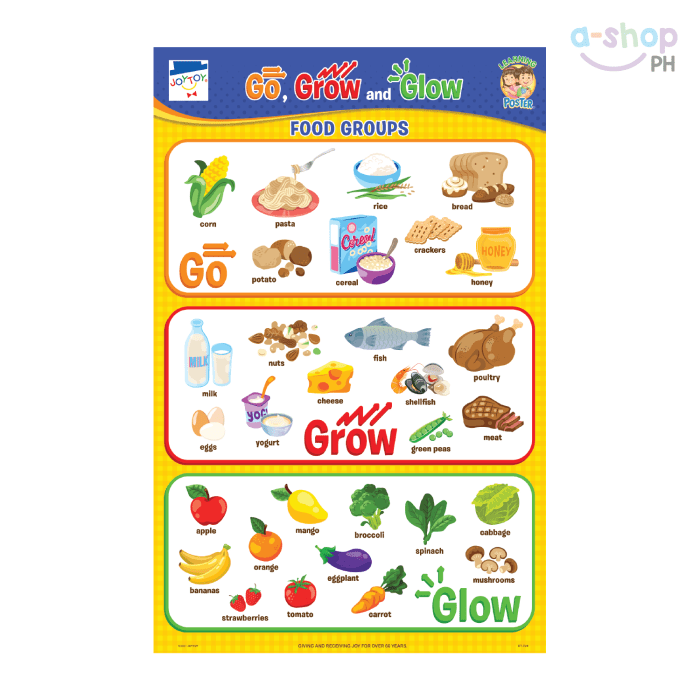
- Fruits and Vegetables: Fruits and vegetables are excellent sources of vitamins, minerals, and fiber. Examples include berries, leafy greens (spinach, kale), broccoli, carrots, and citrus fruits. These foods provide essential antioxidants and help regulate blood pressure.
- Lean Protein Sources: Lean protein is crucial for building and repairing tissues. Examples include skinless poultry (chicken, turkey), fish (salmon, cod), and beans. Choosing lean protein sources limits the intake of phosphorus and other minerals that can strain the kidneys.
- Whole Grains: Whole grains provide fiber and complex carbohydrates, contributing to sustained energy levels. Examples include brown rice, quinoa, oats, and whole-wheat bread. These foods are low in phosphorus and potassium compared to refined grains.
- Low-Fat Dairy Alternatives: Dairy alternatives like unsweetened almond milk, soy milk, or rice milk can provide calcium and protein without the high phosphorus content of cow’s milk. These alternatives are beneficial for maintaining bone health.
Nutritional Components Beneficial for Kidney Health
Understanding the nutritional benefits of these foods is essential for a successful kidney-friendly diet. The specific nutrients help maintain optimal kidney function.
- Antioxidants: Fruits and vegetables are rich in antioxidants, which help protect the kidneys from damage caused by free radicals.
- Fiber: Fiber helps regulate blood sugar and cholesterol levels, reducing strain on the kidneys.
- Potassium: While potassium is essential, individuals with kidney disease may need to limit their intake. It is crucial to consume potassium-rich foods in moderation.
- Protein: Protein is essential, but the amount needed may vary depending on the stage of kidney disease. Moderation and careful selection are important.
Dietary Approaches for Different Stages of Kidney Disease
The recommended dietary approach for kidney disease varies based on the stage and severity of the condition. Tailoring the diet to specific needs is crucial.
- Early-Stage Kidney Disease: Focus on reducing sodium, potassium, and phosphorus intake gradually. Monitor blood tests regularly to adjust the diet accordingly.
- Moderate-Stage Kidney Disease: Stricter limitations on sodium, potassium, phosphorus, and protein intake are often necessary. A registered dietitian or nephrologist should be consulted to create a personalized meal plan.
Sample Meal Plan (One Week)
This sample meal plan provides an example of a healthy kidney-friendly diet. Adjust portions based on individual needs and recommendations from healthcare professionals.
| Food Type | Nutritional Benefits | Serving Size Recommendations | Potential Risks |
|---|---|---|---|
| Fruits (Berries) | Antioxidants, vitamins, low potassium | 1/2 cup | Potential for mild digestive issues in some individuals |
| Vegetables (Leafy Greens) | Vitamins, minerals, low potassium | 1 cup | May contain some oxalates in high amounts |
| Lean Protein (Chicken Breast) | Protein, low phosphorus | 4 oz | May cause digestive issues in some individuals |
| Whole Grains (Brown Rice) | Fiber, complex carbohydrates | 1/2 cup cooked | May cause bloating in some individuals |
Hydration and Fluid Intake
Staying properly hydrated is crucial for overall health, and kidney function is no exception. Adequate fluid intake helps flush out waste products, maintain blood pressure, and support the kidneys’ filtering process. Ignoring hydration can lead to kidney stones, reduced kidney function, and even more serious complications. This section delves into the vital role of hydration in kidney health.Proper hydration is essential for kidney function because it helps to dilute and remove waste products from the blood.
Water is the primary component of urine, and insufficient water intake can lead to concentrated urine, increasing the risk of kidney stones. A well-hydrated body supports the kidneys’ natural filtration processes, preventing the buildup of toxins and maintaining optimal blood pressure.
Recommended Daily Fluid Intake
Daily fluid intake requirements vary based on individual needs and activity levels. Healthy adults generally need to consume approximately 2-3 liters of fluids daily, though this can fluctuate based on factors like climate, activity level, and overall health.For individuals with kidney issues, fluid intake recommendations are often adjusted based on their specific condition and treatment plan. Individuals with kidney disease may have restrictions on their daily fluid intake to manage fluid buildup.
Consult with a nephrologist or registered dietitian for personalized recommendations.
Managing Fluid Intake
Managing fluid intake to prevent excess fluid buildup is critical for individuals with kidney problems. Following a prescribed fluid intake plan is essential to maintain proper kidney function.Monitoring urine output and adjusting intake accordingly is crucial for those with kidney disease. Frequent monitoring allows for adjustments to fluid intake based on individual needs and the progression of the disease.
Maintaining a regular hydration schedule, avoiding excessive intake before bed, and following doctor-recommended guidelines are key strategies for successful management.
Beverage Choices and Kidney Health, How to keep kidneys healthy
The type of beverages consumed also plays a role in kidney health. While water is the most crucial component of a healthy hydration regimen, other beverages can contribute to overall fluid intake.Different beverages offer varying benefits and potential drawbacks. Some drinks contain added sugars, which can contribute to weight gain and potential kidney complications. Others contain high levels of minerals or caffeine, which can influence fluid balance and electrolyte levels.
Consider the impact of each beverage on your overall health and kidney function.
Fluid Content of Beverages
| Beverage Type | Fluid Content (Approximate) | Considerations |
|---|---|---|
| Water | 100% | The ideal choice for hydration. |
| Unsweetened Tea | 99-100% | Many types contain antioxidants, but avoid those with added sugars. |
| Unsweetened Coffee | 99-100% | Caffeine content may affect fluid balance. |
| Milk | 90-95% | Provides protein and calcium, but can be high in sodium in some varieties. |
| Fruit Juices | 90-95% | High in sugar and may not contribute significantly to overall hydration. |
| Soda | 99% | High in sugar, which may impact blood sugar and kidney health. |
Note: These values are approximations. Specific fluid content may vary based on the brand and preparation method.
Exercise and Physical Activity
Staying active is a cornerstone of kidney health. Regular exercise helps manage crucial factors like blood pressure and blood sugar, both of which directly impact kidney function. It also contributes to maintaining a healthy weight, further reducing stress on these vital organs. Consistent physical activity can significantly reduce the risk of developing kidney disease.Exercise plays a vital role in supporting overall kidney function.
It strengthens the body’s ability to filter waste and toxins, thereby reducing the burden on the kidneys. Furthermore, it helps to control blood sugar and blood pressure, two major risk factors for kidney damage.
Benefits of Regular Exercise for Kidney Health
Regular physical activity significantly improves kidney health by enhancing their ability to filter waste effectively. It also plays a crucial role in controlling blood pressure and blood sugar levels, which are major risk factors for kidney disease. Moreover, maintaining a healthy weight through exercise is essential for preventing or managing kidney problems.
Staying hydrated and eating a balanced diet are crucial for healthy kidneys. But did you know that certain conditions, like rheumatoid arthritis, can also impact kidney function? Understanding the signs and symptoms of rheumatoid arthritis, like joint pain and swelling, is important for early diagnosis and management, which in turn can help keep your kidneys healthy. A good diet and regular check-ups are still key for kidney health, no matter what else is going on in your body.
rheumatoid arthritis signs and symptoms This way you can prioritize your overall well-being, ensuring your kidneys stay in tip-top shape.
Recommended Exercises for Healthy Kidneys
A well-rounded exercise program is key for optimal kidney health. This includes aerobic activities, strength training, and flexibility exercises.
- Aerobic Exercises: Activities like brisk walking, jogging, swimming, cycling, or dancing help improve cardiovascular health, which is directly linked to kidney function. These activities increase blood flow, facilitating the removal of waste products from the body.
- Strength Training: Exercises that build muscle mass, such as lifting weights or using resistance bands, help maintain a healthy weight and improve overall body composition. Stronger muscles require more blood flow, promoting better circulation and reducing strain on the kidneys.
- Flexibility Exercises: Stretching and yoga improve joint mobility and flexibility. They can also help reduce stress and improve overall well-being, indirectly contributing to kidney health.
Exercise Routines for Different Fitness Levels and Kidney Conditions
Tailoring exercise routines to individual needs and conditions is essential for safe and effective results. Consult with a healthcare professional before starting any new exercise program, especially if you have kidney disease.
- Beginner Routine: A beginner routine might involve 30 minutes of brisk walking most days of the week, coupled with simple stretching exercises. Gradually increase the duration and intensity as fitness improves.
- Intermediate Routine: This routine could include 45 minutes of moderate-intensity cardio, like jogging or cycling, 2-3 times a week, combined with strength training exercises 2 days a week. Focus on proper form to avoid injuries.
- Advanced Routine: Advanced routines may involve more vigorous cardio, such as running or high-intensity interval training (HIIT), coupled with more challenging strength training. Ensure proper rest and recovery periods are included to avoid overexertion.
- Kidney Disease Specific Routine: Individuals with kidney disease may need to modify their exercise routine based on their specific condition. A healthcare professional can guide the individual on suitable exercises and their appropriate intensity.
Importance of Maintaining a Healthy Weight for Kidney Health
Maintaining a healthy weight is critical for kidney health. Excess weight puts extra strain on the kidneys, making them work harder to filter waste.
Staying hydrated and eating a balanced diet are key for healthy kidneys. It’s also important to manage stress, which surprisingly can impact your overall well-being, including kidney health. Finding ways to manage skin conditions like papulopustular rosacea can also indirectly contribute to a healthier lifestyle. For detailed advice on how to deal with papulopustular rosacea, check out this helpful resource: how to deal with papulopustular rosacea.
Ultimately, prioritizing a holistic approach to your health, from hydration to stress management, will help keep your kidneys functioning optimally.
“Maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce the risk of developing kidney disease.”
How Exercise Controls Blood Pressure and Blood Sugar
Exercise is a powerful tool in managing blood pressure and blood sugar, both critical for kidney health.
- Blood Pressure: Regular physical activity helps lower blood pressure by improving blood vessel function and reducing stress hormones. This reduced pressure prevents damage to the delicate blood vessels in the kidneys.
- Blood Sugar: Exercise improves insulin sensitivity, allowing the body to use blood sugar more efficiently. This is especially beneficial for individuals with diabetes, as it helps control blood sugar levels, preventing further damage to the kidneys.
Managing Medical Conditions
Keeping your kidneys healthy involves more than just diet and exercise. Chronic diseases, such as diabetes and high blood pressure, can significantly impact kidney function. Understanding the connection between these conditions and proactive management is crucial for maintaining long-term kidney health.Effective management of these conditions minimizes the risk of developing kidney disease or slowing its progression. This involves a combination of medication, lifestyle adjustments, and consistent monitoring.
Early detection and prompt intervention are essential for optimal outcomes.
The Link Between Chronic Diseases and Kidney Problems
Chronic diseases like diabetes and high blood pressure are major risk factors for kidney disease. Elevated blood sugar levels in diabetes can damage the delicate blood vessels within the kidneys, leading to impaired filtration and eventually, kidney failure. Similarly, high blood pressure puts excessive strain on these vessels, contributing to their damage and reduced function. Other chronic conditions, including autoimmune diseases and certain infections, can also affect kidney health.
How Effective Management Protects Kidney Health
Effective management of chronic diseases directly translates to better kidney health. When blood sugar and blood pressure are well-controlled, the strain on the kidneys is significantly reduced. This allows the kidneys to function optimally, preserving their filtering capacity and delaying or preventing kidney damage. Furthermore, adherence to treatment plans, including medication and lifestyle modifications, is crucial for achieving and maintaining optimal blood sugar and blood pressure levels.
Importance of Regular Check-ups and Monitoring
Regular check-ups and monitoring are essential for early detection of kidney problems. These check-ups often include blood tests to assess kidney function, such as creatinine and glomerular filtration rate (GFR). Early detection allows for timely intervention, potentially preventing the progression of kidney disease. Patients with chronic diseases, especially those with a family history of kidney problems, should be particularly vigilant about regular check-ups.
These tests can identify potential issues before they cause significant damage. Doctors can then implement appropriate interventions to slow or prevent the progression of the disease.
The Role of Medication and Lifestyle Modifications
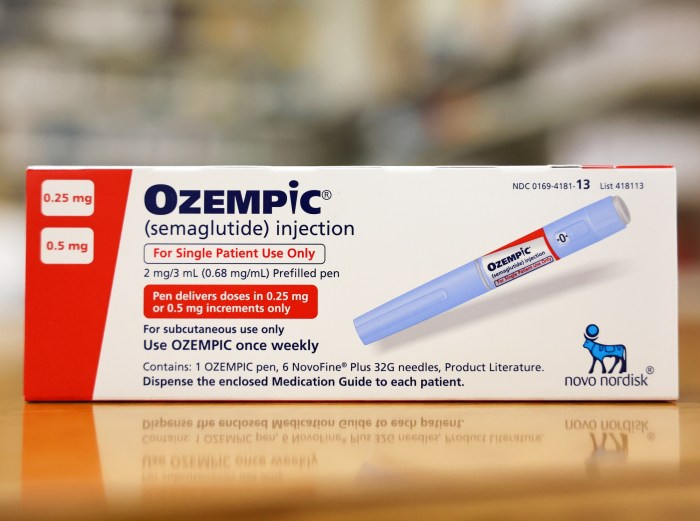
Medication plays a crucial role in managing chronic diseases that affect the kidneys. For example, medications like ACE inhibitors and ARBs are commonly prescribed to control blood pressure and protect kidney function in patients with diabetes or high blood pressure. These medications help relax blood vessels, reducing the strain on the kidneys. Lifestyle modifications, including dietary changes, regular exercise, and stress management, are also critical components of managing chronic diseases and protecting kidney health.
A balanced diet low in sodium and processed foods, combined with regular physical activity, can significantly improve blood pressure and blood sugar control.
Preventative Measures to Mitigate Kidney Disease Risks
Maintaining a healthy lifestyle is key to preventing kidney disease. The following preventative measures can help mitigate risks:
- Maintaining a healthy weight: Obesity is a significant risk factor for various chronic diseases, including kidney disease. Maintaining a healthy weight through a balanced diet and regular exercise can reduce the strain on the kidneys.
- Controlling blood pressure and blood sugar: Regular monitoring and management of blood pressure and blood sugar are essential to prevent kidney damage.
- Following a healthy diet: A diet rich in fruits, vegetables, and whole grains, and low in processed foods and sodium, can significantly improve kidney health. This includes limiting red meat and saturated fats, which can contribute to kidney damage.
- Regular exercise: Regular physical activity helps control blood pressure and blood sugar, reducing the risk of kidney disease.
- Quitting smoking: Smoking damages blood vessels throughout the body, including those in the kidneys. Quitting smoking can significantly reduce the risk of kidney disease.
- Limiting alcohol consumption: Excessive alcohol consumption can negatively impact kidney function. Limiting alcohol intake is an important aspect of maintaining kidney health.
- Managing stress: Chronic stress can increase blood pressure and negatively affect overall health, including kidney function. Practicing stress-reducing techniques, such as yoga or meditation, can be beneficial.
Lifestyle Factors
Maintaining healthy kidneys extends beyond diet and nutrition. Lifestyle choices play a crucial role in preserving kidney function and preventing disease. Stress, sleep, smoking, and alcohol consumption all have significant impacts on kidney health, and proactive management is key. Understanding these connections empowers individuals to make informed decisions for optimal kidney well-being.Stress and inadequate sleep can negatively influence kidney function.
The body’s response to chronic stress releases hormones that can damage blood vessels and increase blood pressure, putting strain on the kidneys. Likewise, insufficient sleep can disrupt the body’s natural regulatory processes, potentially impacting kidney health.
Impact of Stress on Kidney Health
Chronic stress triggers the release of hormones like cortisol and adrenaline. Elevated levels of these hormones can constrict blood vessels, leading to increased blood pressure. Sustained high blood pressure is a major risk factor for kidney disease. Prolonged stress can also weaken the kidneys’ filtering ability, potentially causing damage over time. Individuals experiencing high levels of stress may exhibit reduced kidney function, evidenced by elevated creatinine and blood urea nitrogen (BUN) levels in blood tests.
Impact of Sleep on Kidney Health
Adequate sleep is essential for overall health, including kidney function. Insufficient sleep can disrupt the body’s natural regulatory processes, potentially impacting the kidneys’ ability to filter waste products efficiently. This can lead to an accumulation of toxins in the blood, potentially contributing to kidney damage. Poor sleep patterns may also contribute to the development of high blood pressure and other risk factors for kidney disease.
Studies have shown a correlation between chronic sleep deprivation and an increased risk of developing chronic kidney disease.
Strategies for Managing Stress
Effective stress management is vital for kidney health. Implementing stress-reduction techniques can help mitigate the negative effects of stress on the kidneys. These include:
- Mindfulness and meditation practices can help calm the mind and body, reducing stress hormones.
- Regular exercise can release endorphins, which have mood-boosting effects and help reduce stress.
- Establishing a consistent sleep schedule and practicing relaxation techniques like deep breathing exercises can improve sleep quality and reduce stress levels.
- Seeking support from friends, family, or a therapist can provide emotional relief and practical coping strategies.
Strategies for Improving Sleep Quality
Prioritizing sleep is crucial for overall health, including kidney function. Improving sleep quality involves:
- Creating a relaxing bedtime routine that signals to the body it’s time to sleep.
- Establishing a regular sleep schedule, even on weekends, to regulate the body’s natural sleep-wake cycle.
- Creating a sleep-conducive environment, free from distractions like noise and light.
- Limiting exposure to electronic devices before bed, as the blue light emitted can interfere with sleep.
Avoiding Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption are detrimental to kidney health. Both habits contribute to various health problems that can negatively impact kidney function.
Impact of Smoking on Kidney Health
Smoking damages blood vessels throughout the body, including those in the kidneys. This can lead to reduced blood flow to the kidneys, hindering their ability to filter waste effectively. Smoking also increases the risk of developing high blood pressure, a significant risk factor for kidney disease. Furthermore, the chemicals in cigarettes can directly damage kidney tissues, potentially leading to chronic kidney disease.
Smoking significantly increases the likelihood of developing kidney diseases, particularly among individuals with pre-existing kidney conditions.
Impact of Excessive Alcohol Consumption on Kidney Health
Excessive alcohol consumption can put a considerable strain on the kidneys. The liver and kidneys work together to process alcohol. When excessive amounts of alcohol are consumed, the kidneys are required to work overtime to filter out the toxins, which can lead to damage over time. Chronic alcohol abuse can lead to dehydration, further stressing the kidneys.
Excessive alcohol consumption is linked to an increased risk of developing kidney disease and chronic kidney failure. In some cases, alcohol abuse can even lead to acute kidney injury.
Supplements and Herbal Remedies

Taking supplements and herbal remedies for kidney health can be tempting, but it’s crucial to approach this with caution. While some nutrients play vital roles in kidney function, self-treating with supplements or herbs without professional guidance can be risky. Kidney health is complex, and a personalized approach, guided by a healthcare professional, is always the best strategy.Many vitamins and minerals are essential for overall health, and some play a specific role in kidney function.
However, the amount needed, and whether supplementation is necessary, varies significantly from person to person. Understanding these nuances is critical before adding any supplements to your routine.
Vitamins and Minerals for Kidney Health
Various vitamins and minerals contribute to kidney health. For instance, vitamin C can aid in antioxidant protection, potentially mitigating oxidative stress that can harm the kidneys. Vitamin D is crucial for calcium absorption, which is essential for bone health, and indirectly affects kidney function. Magnesium is involved in numerous metabolic processes, including those in the kidneys. Potassium is important for maintaining electrolyte balance, and a balanced potassium intake is essential for kidney health.
Beneficial Supplements for Kidney Health
Some supplements might be beneficial for kidney health when taken under medical supervision. However, it’s important to consult a doctor before starting any supplementation. This is particularly true for individuals with existing kidney conditions or those taking other medications. Supplements like vitamin D and magnesium, in appropriate dosages, might be beneficial. However, the specific needs depend on individual circumstances.
Potentially Harmful Supplements
Certain supplements can be detrimental to kidney health. For example, high doses of vitamin C can cause kidney stones in susceptible individuals. Herbal remedies, even those seemingly harmless, can interact with medications or have unknown effects on kidney function. Always check with a doctor before using herbal remedies or high-dose supplements. Some herbal remedies, such as those containing aristolochic acid, have been linked to severe kidney damage.
Importance of Consulting a Healthcare Professional
Before taking any supplements or herbal remedies, consulting a healthcare professional is paramount. A healthcare professional can assess your individual needs, evaluate your current health status, and recommend appropriate dosages. This is especially crucial for individuals with kidney disease or other underlying health conditions. They can help determine if supplementation is necessary and if so, what specific supplements are safe and appropriate.
Obtaining Vitamins and Minerals from Food
Many essential vitamins and minerals for kidney health can be obtained through a balanced diet. Fruits, vegetables, whole grains, and lean proteins are excellent sources of various nutrients. A well-rounded diet, rich in fresh produce, can often meet your nutritional needs without the need for supplements. For example, leafy greens are a great source of potassium, while citrus fruits are rich in vitamin C.
Understanding the nutritional content of different foods can help you create a diet that supports your kidney health.
Risks of Self-Treating Kidney Problems with Herbal Remedies
Self-treating kidney problems with herbal remedies is extremely risky. Unregulated herbal remedies may contain hidden or unknown ingredients that could worsen existing kidney conditions or cause unexpected side effects. Herbal remedies are not always as safe as they seem. Some herbal remedies can interfere with prescription medications, leading to dangerous interactions. Always prioritize consulting a healthcare professional before using any herbal remedy or supplement, particularly if you have kidney issues.
Kidney-Friendly Recipes: How To Keep Kidneys Healthy
Nourishing your kidneys doesn’t have to mean sacrificing flavor or variety. This section explores delicious and easy-to-prepare recipes specifically designed to support kidney health. By focusing on low-sodium, low-potassium, and low-phosphorus options, you can enjoy satisfying meals while managing your kidney health.
Breakfast Recipes
Breakfasts should be packed with nutrients to kickstart your day and support kidney function. These recipes emphasize lean protein, complex carbohydrates, and plenty of fruits and vegetables, all while keeping sodium and potassium in check.
- Kidney-Friendly Oatmeal with Berries and Nuts: Cook rolled oats with water or low-sodium broth. Top with fresh berries, a handful of unsalted nuts, and a sprinkle of cinnamon. This provides fiber for digestive health and antioxidants for overall well-being. Adjust portion sizes based on individual potassium limits.
- Scrambled Eggs with Spinach and Whole-Wheat Toast: Whisk eggs with a splash of low-sodium milk or broth. Sauté fresh spinach until wilted. Serve with a slice of whole-wheat toast. This recipe provides protein for satiety and essential vitamins and minerals.
Lunch Recipes
A balanced lunch is crucial for maintaining energy levels and supporting kidney function. These options are designed to be filling and nutritious while managing the key minerals to be mindful of.
- Quinoa Salad with Vegetables and Grilled Chicken: Cook quinoa according to package directions. Combine with chopped cucumber, bell peppers, tomatoes, and grilled chicken breast (ensure low-sodium seasoning). This provides a complete protein source, complex carbohydrates, and essential vitamins and minerals. Adjust portion sizes based on individual potassium and phosphorus limits.
- Kidney-Friendly Leftover Chicken Stir-Fry: Leftovers from the previous night’s dinner can be excellent for lunch, especially if the stir-fry was made with vegetables and lean protein. Make sure to adjust seasonings to avoid excessive sodium and monitor potassium and phosphorus levels.
Dinner Recipes
Dinner is often the most substantial meal of the day. These kidney-friendly options focus on lean protein, plenty of vegetables, and whole grains to promote a healthy and balanced diet.
- Baked Salmon with Roasted Asparagus and Sweet Potatoes: Bake salmon fillets seasoned with herbs and spices. Roast asparagus and sweet potatoes with a drizzle of olive oil. This provides healthy fats, protein, and essential vitamins and minerals. Ensure the salmon is baked and not fried.
- Lentil Soup with Whole-Wheat Bread: This soup is rich in protein and fiber, making it a filling and nutritious choice. Make sure the lentils are cooked with low-sodium broth and avoid high-sodium seasonings.
Snacks
Healthy snacks are essential for maintaining energy levels and preventing hunger between meals. These options are low in potassium, phosphorus, and sodium while being satisfying.
- Fruit Salad (with careful selection): A variety of fruits like apples, berries, and pears can be enjoyed as a snack. Be mindful of potassium content in certain fruits and adjust portion sizes accordingly.
- Plain, Unsalted Popcorn: Air-popped popcorn is a low-calorie, low-sodium snack that provides fiber. Avoid adding butter or other high-sodium seasonings.
Nutritional Comparison Table
| Recipe | Protein (grams) | Potassium (mg) | Phosphorus (mg) | Sodium (mg) |
|---|---|---|---|---|
| Kidney-Friendly Oatmeal | 5 | 50 | 20 | 50 |
| Scrambled Eggs | 10 | 100 | 50 | 80 |
| Quinoa Salad | 25 | 150 | 100 | 75 |
| Baked Salmon | 20 | 120 | 70 | 60 |
Note: Nutritional values are approximate and may vary based on specific ingredients and portion sizes. Always consult with a registered dietitian or nephrologist for personalized dietary recommendations.
Wrap-Up
In conclusion, maintaining healthy kidneys is a multifaceted approach encompassing diet, hydration, exercise, and management of underlying conditions. By adopting a proactive and mindful lifestyle, you can significantly reduce the risk of kidney disease and enjoy optimal kidney function for years to come. Remember that consistency and a holistic approach are key. Consult your healthcare provider for personalized recommendations based on your specific needs and medical history.