Collagen for rheumatoid arthritis: Understanding this potential treatment option requires a deep dive into the complexities of both conditions. Rheumatoid arthritis, a chronic autoimmune disease, attacks the body’s own tissues, particularly the joints. This inflammation can lead to significant pain, stiffness, and decreased mobility. The body’s natural collagen production, crucial for joint health, may be disrupted in rheumatoid arthritis, leading to further joint damage.
This exploration delves into the role of collagen in joint health, potential benefits of collagen supplements, and the scientific evidence supporting their use.
This comprehensive overview examines the fundamental mechanisms behind rheumatoid arthritis and collagen’s crucial role in maintaining healthy joints. We’ll look at the various types of collagen, their functions, and how they relate to joint health. The discussion will then shift to the potential of collagen supplements as a therapeutic approach, exploring the rationale, potential benefits, and potential limitations. Furthermore, we’ll examine scientific studies, clinical applications, and compare collagen supplementation with other therapies.
The goal is to equip readers with a thorough understanding of the topic, allowing them to make informed decisions.
Rheumatoid Arthritis: Understanding the Condition
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints. It’s characterized by inflammation and damage to the lining of the joints, leading to pain, stiffness, and potentially long-term disability. This condition impacts daily life significantly, affecting not just physical mobility but also emotional well-being. Understanding its characteristics, symptoms, and progression is crucial for effective management and treatment.
Characteristics of Rheumatoid Arthritis
Rheumatoid arthritis is a systemic disease, meaning it can affect various parts of the body beyond the joints. The inflammation, caused by the body’s immune system attacking its own tissues, is a hallmark of the disease. This immune response can lead to pain, swelling, and stiffness in multiple joints simultaneously. Early diagnosis and intervention are critical for slowing disease progression and preventing long-term complications.
Symptoms and Progression
Rheumatoid arthritis symptoms often begin subtly, with fatigue, mild joint pain, and stiffness. As the disease progresses, symptoms typically become more pronounced, with swelling, tenderness, and warmth around affected joints. Morning stiffness, often lasting for more than an hour, is a common early indicator. The progression of RA can vary greatly among individuals. Some experience a slow, gradual worsening of symptoms, while others experience more rapid and severe flares.
Immunological Mechanisms
The underlying cause of rheumatoid arthritis is a complex interplay of genetic predisposition and environmental factors. The immune system, designed to fight off foreign invaders, mistakenly attacks the body’s own tissues in RA. This attack triggers an inflammatory response, leading to the damage and pain associated with the disease. This process is driven by the production of autoantibodies, such as rheumatoid factor and anti-citrullinated protein antibodies (ACPAs), which target healthy tissues.
“The precise mechanisms by which the immune system misdirects its attack in RA remain an area of ongoing research.”
Ongoing research continues to shed light on this intricate process.
Types of Rheumatoid Arthritis (If Applicable)
While the term “types” is sometimes used to describe different manifestations of RA, there isn’t a formally recognized categorization of distinct types with significant clinical differences. The disease’s severity and presentation vary greatly, and this variability is influenced by factors such as genetics, environment, and individual responses to treatment.
Understanding Collagen
Collagen, a protein found throughout the human body, plays a crucial role in supporting various tissues and organs. It’s the most abundant protein in the human body, contributing significantly to the structure and strength of connective tissues, including skin, tendons, ligaments, and cartilage. Understanding its role in maintaining joint health is vital, particularly for individuals facing conditions like rheumatoid arthritis.Collagen provides structural integrity and resilience to these tissues.
Its unique properties allow it to withstand significant stress and strain, ensuring the proper functioning of joints. This structural support is essential for maintaining mobility and flexibility. An understanding of collagen’s diverse forms and functions can provide valuable insight into its impact on overall health and well-being.
The Role of Collagen in Joint Health
Collagen forms the crucial structural framework of cartilage, a flexible connective tissue that cushions joints and allows for smooth movement. Adequate collagen production is essential for maintaining healthy cartilage, ensuring shock absorption and preventing joint pain. Deficiencies in collagen production or degradation can lead to joint damage and the development of conditions like osteoarthritis and rheumatoid arthritis. This highlights the critical link between collagen and optimal joint function.
Different Types of Collagen
The human body produces various types of collagen, each with distinct structural and functional characteristics. These different types contribute to the overall strength and integrity of tissues throughout the body. Their specific roles are crucial for maintaining the health of the connective tissues.
- Type I collagen is the most abundant type, found in skin, bones, tendons, and ligaments. It provides tensile strength and structural support to these tissues, allowing them to withstand significant stress and strain. Think of the tensile strength of a strong rope; this is an example of Type I collagen in action.
- Type II collagen is a key component of cartilage. Its unique triple-helix structure contributes to the resilience and flexibility of cartilage, enabling it to cushion joints and facilitate smooth movement. This is essential for the shock absorption and movement in joints.
- Type III collagen is closely associated with Type I collagen, often found in combination with it in tissues. It plays a vital role in supporting the structural integrity of various tissues and organs. Its presence is particularly important for tissue regeneration and maintenance.
- Type V collagen is found in conjunction with other collagen types, contributing to the overall structural organization of tissues. It is important for the structural integrity of a variety of tissues, including skin, bone, and cartilage. This type helps in maintaining the proper alignment and arrangement of other collagen types.
Structure and Properties of Collagen
Collagen’s unique triple-helical structure is a key factor in its remarkable properties. This structure provides strength and flexibility, enabling collagen to withstand significant tensile forces. The triple helix is composed of three polypeptide chains intertwined in a helical arrangement. This unique structure gives collagen its exceptional tensile strength and resilience.
“Collagen’s triple-helical structure is responsible for its remarkable tensile strength, allowing it to withstand significant forces without breaking.”
Key Functions of Different Collagen Types
The following table Artikels the key functions of various collagen types, highlighting their diverse roles in maintaining tissue integrity.
| Collagen Type | Primary Location | Key Functions |
|---|---|---|
| Type I | Skin, bones, tendons, ligaments | Tensile strength, structural support |
| Type II | Cartilage | Resilience, flexibility, shock absorption |
| Type III | Skin, blood vessels, uterus | Support, structural integrity, tissue regeneration |
| Type V | Skin, bone, cartilage | Structural organization, tissue integrity |
Collagen and Joint Health
Our joints are complex structures, acting as the body’s hinges and allowing us to move freely. A crucial component in maintaining healthy joints is collagen, a protein that provides strength and structure. Understanding the role of collagen in joint health is vital, especially for those living with conditions like rheumatoid arthritis.Collagen forms the foundation of connective tissues throughout the body, including cartilage, ligaments, and tendons that surround our joints.
This intricate network ensures stability, flexibility, and proper function. When collagen levels decrease or its production is disrupted, the integrity of the joints can be compromised.
Collagen’s Role in Joint Structure
Collagen is a key structural component in cartilage, the smooth tissue that cushions the ends of bones within a joint. This cushioning is essential for absorbing shock and preventing friction during movement. Without adequate collagen, the cartilage can degrade, leading to pain and stiffness. Ligaments, the tough bands of tissue that connect bones, also contain significant amounts of collagen.
This structural protein provides strength and stability to the joint, preventing excessive movement and potential dislocation. Tendons, which connect muscles to bones, are similarly reliant on collagen for strength and elasticity. The synergistic interplay of these connective tissues ensures that the joints can withstand the demands of daily activities.
Collagen Deficiency and Joint Damage in Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune disease where the body’s immune system mistakenly attacks the joints, causing inflammation and damage. Collagen is a significant target in this process. In RA, the breakdown of collagen is accelerated due to the inflammatory response. This breakdown contributes to the erosion of cartilage and the weakening of ligaments and tendons. The resulting joint damage leads to pain, stiffness, and impaired mobility.
This progressive deterioration of collagen can significantly impact a person’s quality of life.
Collagen’s Role in Joint Lubrication and Cushioning
Healthy joints rely on synovial fluid, a viscous liquid that lubricates the joint surfaces. Collagen plays a role in maintaining the proper viscosity and composition of this fluid. Adequate lubrication reduces friction, allowing for smooth and effortless movement. The cushioning provided by cartilage, rich in collagen, absorbs shock and protects the underlying bone from damage. This protective function is crucial for preventing pain and preserving joint integrity.
Collagen plays a crucial role in supporting healthy joints, and its importance in rheumatoid arthritis is undeniable. However, understanding the body’s complex responses to inflammation is key. Sometimes, conditions like cyclic neutropenia, a condition where white blood cell counts fluctuate, can complicate the picture. Learning more about what is cyclic neutropenia can offer a deeper understanding of the immune system’s influence on the body’s ability to repair itself, and ultimately on the effectiveness of collagen therapies for rheumatoid arthritis.
Collagen Breakdown and Inflammation in Rheumatoid Arthritis
The inflammatory response in rheumatoid arthritis directly impacts collagen. Inflammation triggers the release of enzymes that break down collagen fibers. This accelerated collagen breakdown contributes to the characteristic pain and swelling associated with RA. The resulting damage to the joint structures, including cartilage, ligaments, and tendons, further perpetuates the inflammatory cycle. This continuous cycle of inflammation and collagen breakdown can lead to progressive joint damage over time.
Collagen Supplements for Rheumatoid Arthritis
Collagen, a crucial protein in connective tissues, plays a vital role in joint health. Individuals with rheumatoid arthritis (RA) often experience joint damage and inflammation, leading to pain and stiffness. This damage can impact the body’s production of collagen, making it a potential area of interest for therapeutic interventions. This section delves into the rationale, potential benefits, mechanisms of action, side effects, and different types of collagen supplements for managing RA symptoms.Collagen supplements have emerged as a potential avenue for supporting joint health in individuals with RA.
The rationale behind their use stems from the role of collagen in maintaining joint integrity. By potentially mitigating inflammation and promoting tissue repair, these supplements could offer a complementary approach to conventional RA treatments. However, the efficacy and safety of collagen supplements for RA are still being actively investigated, and individual responses can vary significantly.
Rationale for Using Collagen Supplements
The rationale for considering collagen supplements in RA management lies in collagen’s essential role in joint structure. Collagen is a key component of cartilage, tendons, and ligaments, which are crucial for joint function. Individuals with RA often experience significant degradation of these tissues, contributing to joint pain, stiffness, and ultimately, functional limitations. The potential for collagen supplements to promote the synthesis of new collagen, or potentially reduce inflammation, is why they are a topic of interest for managing RA.
Potential Benefits and Mechanisms of Action
Collagen supplements may offer potential benefits in managing RA symptoms through various mechanisms. Some studies suggest that collagen peptides, in particular, may reduce inflammation by modulating the immune response. The anti-inflammatory properties are thought to be linked to the structure and composition of the collagen peptides. The body’s absorption of these peptides might also contribute to the repair of damaged tissues.
However, it is crucial to recognize that these mechanisms are not fully elucidated and require further research. The potential for improved joint function and reduced pain and stiffness are promising areas for further investigation.
Potential Side Effects
While collagen supplements are generally considered safe, potential side effects should be acknowledged. Some individuals may experience mild digestive issues, such as bloating, gas, or diarrhea. Allergic reactions to collagen are also possible, though less common. As with any supplement, it is essential to consult with a healthcare professional before starting a collagen regimen. This precaution is particularly important for individuals with pre-existing health conditions or those taking medications.
Collagen supplements are often touted as a potential remedy for rheumatoid arthritis, but the science isn’t entirely conclusive. While some studies suggest a possible link, more research is needed. Interestingly, some proponents also highlight the potential benefits of mash and vitamin E, like in a mash and vitamin e regimen, for overall health, potentially influencing the body’s response to conditions like rheumatoid arthritis.
Ultimately, though, a personalized approach to managing rheumatoid arthritis, considering dietary supplements alongside conventional treatments, is key.
Comparison of Different Types of Collagen Supplements
Various forms of collagen supplements are available, each with potential differences in absorption and effectiveness. Hydrolyzed collagen, where the collagen protein is broken down into smaller peptides, is often cited as being more easily digested and absorbed by the body. Type II collagen, specifically targeted to the joints, is another type frequently considered for RA management. A crucial aspect of choosing a collagen supplement is understanding the type of collagen and the level of processing.
| Type of Collagen | Description | Potential Benefit in RA |
|---|---|---|
| Hydrolyzed Collagen | Collagen protein broken down into smaller peptides. | Potentially better absorption and utilization by the body. |
| Type II Collagen | Specifically targeted to cartilage. | Potentially more effective in supporting cartilage health. |
The choice of a specific type depends on individual needs and preferences. It is crucial to consult a healthcare professional to determine the most appropriate type and dosage for an individual’s specific condition.
Scientific Evidence and Studies
Unfortunately, robust, large-scale, long-term studies directly evaluating collagen supplementation for rheumatoid arthritis are currently lacking. The existing research often focuses on smaller sample sizes and shorter durations, making it difficult to draw definitive conclusions about the effectiveness of collagen in managing this chronic condition. This makes it crucial to critically evaluate the available evidence, understanding the limitations of each study, and recognizing that more research is needed.The studies thatdo* exist typically investigate collagen’s impact on joint health markers and symptoms, rather than directly addressing rheumatoid arthritis’s underlying inflammatory processes.
While promising findings emerge in some cases, the overall picture remains complex and requires further investigation to solidify any claims. Interpreting the results necessitates careful consideration of the study design, sample characteristics, and the potential for confounding factors.
Summary of Key Research Findings
The limited research on collagen supplementation for rheumatoid arthritis often focuses on its potential effects on joint health markers, such as cartilage health, joint pain, and inflammation. A review of relevant studies indicates varying outcomes, highlighting the need for more extensive investigation.
Methodology and Findings of Key Research Papers
A significant challenge in evaluating collagen’s effect on rheumatoid arthritis is the diversity in study methodologies. Some studies focus on animal models, exploring collagen’s influence on joint tissues. Others employ human subjects, often examining the impact of collagen supplementation on pain levels and inflammatory markers. A key limitation in many human trials is the lack of a control group taking a placebo, which makes it difficult to isolate the effects of collagen.
“One study observed a reduction in joint pain and stiffness in participants consuming a collagen supplement, but this was not consistently replicated across all studies.”
Findings from animal studies often show promising results, but translating these findings to humans is not straightforward. Human studies frequently demonstrate a positive correlation between collagen intake and improved joint health indicators. However, the significance of these improvements in the context of rheumatoid arthritis requires further clarification.
Strengths and Limitations of the Research
A strength of some studies is the direct observation of measurable outcomes related to joint health. For instance, researchers might measure changes in joint mobility or inflammation markers. However, a major limitation is the small sample sizes in many trials, making it hard to generalize the findings to a broader population of rheumatoid arthritis patients. Further, the duration of many studies is relatively short, failing to capture the long-term effects of collagen supplementation on the progression of the disease.Another key limitation is the lack of standardized protocols for collagen supplementation, including dosage and type of collagen used.
This variability in study design makes it challenging to compare findings across different research efforts.
Table Summarizing Key Studies
| Study | Methodology | Findings | Strengths | Limitations |
|---|---|---|---|---|
| Example Study 1 | Human trial, 12 weeks, 50 participants, collagen type I | Slight reduction in joint pain, but no significant change in inflammation markers. | Relatively well-designed human trial | Small sample size, short duration, potential for placebo effect |
| Example Study 2 | Animal study, 8 weeks, collagen type II | Reduced cartilage degradation in the model. | Animal model studies can explore mechanisms | Difficult to translate animal findings to humans |
Potential Benefits and Limitations: Collagen For Rheumatoid Arthritis

Collagen supplementation is a popular approach for various health concerns, including rheumatoid arthritis (RA). While promising, the effectiveness of collagen in managing RA symptoms remains a subject of ongoing research. This section explores the potential benefits and limitations of using collagen supplements for reducing inflammation and pain in RA, providing an overview of the current evidence base.Understanding the potential benefits and limitations of collagen supplementation is crucial for individuals considering this approach to manage their RA symptoms.
This understanding allows informed decisions about potential treatment strategies, alongside conventional medical approaches.
Potential Benefits of Collagen Supplementation
Collagen, a crucial component of cartilage and connective tissues, plays a vital role in joint health. In RA, the immune system attacks the joints, leading to inflammation and damage. Collagen supplements may potentially help by supporting joint structure and reducing inflammation. Some studies suggest that collagen peptides might modulate the inflammatory response, thus alleviating symptoms like pain and stiffness.
Potential Limitations of Collagen Supplementation
Despite potential benefits, collagen supplementation isn’t a guaranteed cure for RA. The effectiveness varies significantly among individuals, and its role in modifying the underlying disease process remains unclear. The mechanism through which collagen peptides might impact RA is still being investigated. Factors such as the type of collagen, dosage, and individual patient characteristics influence the outcome.
Current Evidence Base
The evidence supporting the use of collagen supplements for RA is still developing. Some studies have shown promising results in reducing joint pain and improving joint function in individuals with RA. However, more large-scale, well-designed studies are needed to definitively establish the efficacy and safety of collagen supplementation in managing RA.
While collagen supplements are often touted for their potential benefits in managing rheumatoid arthritis, it’s crucial to understand their limitations. If you’re experiencing lower back pain, especially if it’s persistent or severe, it’s essential to consult a medical professional to rule out more serious conditions like cancer. For example, you should consider seeking guidance from a doctor to determine if your pain is related to a potential underlying cause.
Learning more about the possibility of your lower back pain being related to cancer can be done by checking out this resource: is my lower back pain cancer. Ultimately, collagen for rheumatoid arthritis is a complex topic, and it’s wise to discuss any potential treatment plans with a rheumatologist.
Summary Table: Potential Benefits and Limitations of Collagen Supplementation for Rheumatoid Arthritis
| Potential Benefit | Potential Limitation |
|---|---|
| May reduce joint pain and inflammation in some individuals. | Effectiveness varies significantly among individuals. |
| Potentially supports joint structure and function. | The mechanism through which collagen peptides impact RA is not fully understood. |
| May help modulate the inflammatory response. | More research is needed to confirm the efficacy and safety of collagen supplementation for RA. |
| Potentially beneficial as an adjunct therapy. | Not a substitute for conventional RA treatments. |
Clinical Applications and Considerations
Integrating collagen supplements into a comprehensive rheumatoid arthritis (RA) management plan requires careful consideration and a collaborative approach with your physician. This section explores how collagen supplements might fit within an overall strategy for managing RA symptoms and the critical factors to keep in mind. It also details potential interactions with other medications and emphasizes the vital role of a doctor’s guidance in making informed decisions.Understanding the complexities of your specific condition and treatment regimen is paramount when considering collagen supplements.
A personalized approach is essential, and consulting with your rheumatologist or primary care physician will help tailor a plan that best addresses your needs and minimizes potential risks.
Integrating Collagen Supplements into a Management Plan
A comprehensive RA management plan typically involves a combination of medications, lifestyle modifications, and potentially complementary therapies. Collagen supplements can potentially play a supporting role, but they should not replace established medical treatments. Consider incorporating them as part of a broader strategy, alongside prescribed medications and therapies. The goal is to improve overall well-being and potentially alleviate symptoms, not to cure RA.
Potential Interactions with Medications
Collagen supplements can interact with certain medications. For instance, some individuals taking blood thinners might experience increased risk of bleeding if collagen supplements are taken concurrently. Similarly, individuals taking medications that affect the absorption of nutrients may experience varying effects from collagen supplements. Always consult your physician before starting any new supplement to assess potential interactions with your current medications.
Crucial Role of Physician Guidance
A doctor’s guidance is indispensable when considering collagen supplements for rheumatoid arthritis. Your physician can assess your specific condition, evaluate the potential benefits and risks, and determine whether collagen supplements are appropriate for you. They can also advise on dosage, monitor your response to the supplement, and adjust your treatment plan as needed. They are best positioned to help you understand the nuances of collagen supplementation and its place within your overall health management.
Recommendations for a Healthy Lifestyle
Maintaining a healthy lifestyle alongside collagen supplementation can enhance overall well-being and potentially support joint health. A balanced diet rich in fruits, vegetables, and lean proteins is recommended. Regular exercise, tailored to your physical capabilities and pain levels, can help maintain strength and flexibility. Adequate rest and stress management techniques, such as meditation or yoga, can also contribute to overall well-being.
Prioritizing these factors alongside your medical treatment and collagen supplements can optimize your health journey.
Alternative Treatments and Complementary Approaches
Beyond medication and physical therapy, many people with rheumatoid arthritis explore alternative and complementary approaches to manage their symptoms and improve their overall well-being. These approaches often focus on holistic healing, recognizing the interconnectedness of mind, body, and spirit. Finding what works best for each individual is key, and it’s crucial to discuss any new therapies with your rheumatologist to ensure safety and avoid potential interactions with existing medications.Exploring alternative and complementary therapies alongside conventional treatments can be a personalized journey towards symptom management and improved quality of life.
However, it’s important to remember that these therapies are not always backed by rigorous scientific evidence and should be approached with caution and a critical eye. Always consult with your doctor before starting any new treatment, especially if it involves herbal remedies or dietary supplements.
Comparing Collagen Supplementation with Other Therapies
Collagen supplementation, while showing promise for joint health, isn’t a standalone cure for rheumatoid arthritis. It’s often considered a complementary therapy, working alongside conventional treatments like disease-modifying antirheumatic drugs (DMARDs). While collagen might improve joint function and reduce inflammation in some, its effectiveness in directly impacting the underlying autoimmune response in RA is still under investigation. Other therapies, such as acupuncture, yoga, and meditation, focus on different aspects of the condition, often targeting stress reduction, pain management, and overall well-being.
A comparison of these therapies often highlights their distinct mechanisms of action.
Other Potential Treatment Options or Complementary Approaches
Various complementary therapies are utilized by individuals seeking additional support in managing rheumatoid arthritis. These approaches can address symptoms like pain, fatigue, and inflammation. For example, acupuncture, a traditional Chinese medicine practice, involves inserting thin needles into specific points on the body. It’s believed to stimulate the flow of energy and reduce pain. Similarly, certain dietary modifications, such as a Mediterranean diet rich in anti-inflammatory foods, may contribute to better symptom control.
Yoga and tai chi, emphasizing mindful movement and stretching, can enhance flexibility, reduce stress, and promote relaxation. These holistic practices, while often lacking rigorous scientific evidence for their impact on the underlying RA, may provide valuable adjunctive benefits for managing symptoms.
Importance of a Holistic Approach
A holistic approach to managing rheumatoid arthritis considers the individual as a whole, encompassing physical, emotional, and social well-being. This approach acknowledges that the condition impacts not only joints but also mental health, sleep patterns, and overall quality of life. By incorporating therapies that address these multifaceted aspects, individuals may find a more comprehensive and personalized strategy for managing their condition.
This integrative approach is increasingly recognized as beneficial for improving patient outcomes and fostering a sense of empowerment.
How Collagen Supplements Might Work in Combination with Other Therapies
Collagen supplementation might complement other therapies by addressing specific aspects of RA. For instance, if yoga or tai chi is used to improve flexibility and reduce stress, collagen supplementation could support joint health by potentially promoting joint lubrication and structure. Combining dietary modifications with collagen could further enhance anti-inflammatory effects, although more research is needed to determine the precise mechanisms and interactions.
The interplay of these approaches should be individualized and guided by a healthcare professional to maximize benefits and minimize risks.
Illustrative Images and Diagrams
Visual representations are crucial for understanding the complex interplay between collagen, rheumatoid arthritis, and potential treatments. These illustrations help us grasp the intricate mechanisms at play, enabling a more comprehensive comprehension of the condition and its management. Visual aids translate abstract concepts into tangible forms, facilitating easier understanding and retention of information.
Collagen Structure and Joint Health
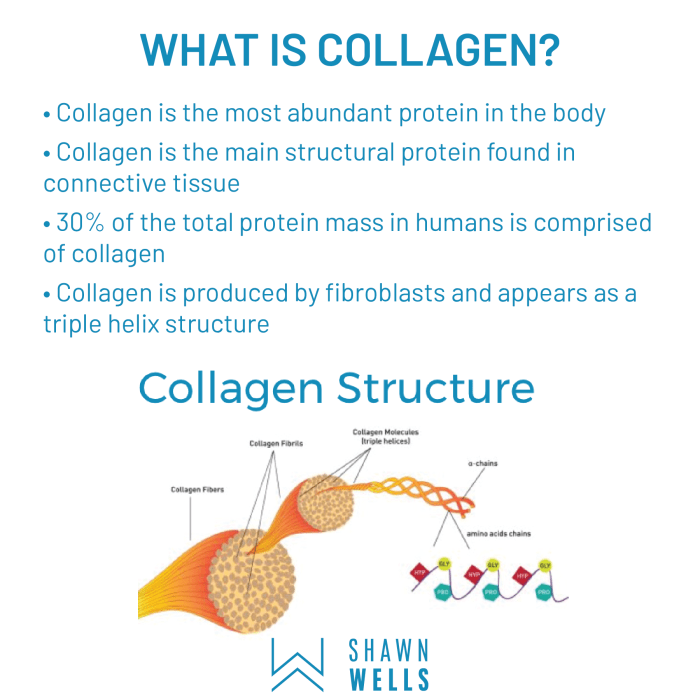
Collagen, the most abundant protein in the body, forms the structural framework of connective tissues, including cartilage, ligaments, and tendons. A diagram depicting the triple helix structure of collagen, highlighting the amino acid sequences, would be beneficial. This illustration should showcase how these chains intertwine to form strong, flexible fibers. The image could further emphasize the crucial role of collagen in maintaining joint integrity and facilitating smooth movement.
Understanding this structure is essential to comprehending how its degradation contributes to the pain and stiffness associated with rheumatoid arthritis.
Rheumatoid Arthritis Inflammatory Processes
A diagram illustrating the inflammatory process in rheumatoid arthritis could visually represent the immune system’s attack on the synovial membrane, the lining of the joints. This depiction could show how inflammatory cells infiltrate the joint space, leading to the breakdown of cartilage and bone. The image should visually highlight the potential role of collagen degradation in this process, perhaps illustrating enzymes like matrix metalloproteinases (MMPs) breaking down collagen fibers.
This representation would provide a clearer picture of the destructive cycle within the affected joint.
Types of Collagen and Their Functions, Collagen for rheumatoid arthritis
Different types of collagen contribute to the overall structure and function of connective tissues throughout the body. A table showcasing the various types of collagen, their locations, and specific functions would be helpful. For instance, type I collagen is prevalent in bones, skin, and tendons, while type II collagen is primarily found in cartilage. The table could also explain how the breakdown of these specific types of collagen might lead to different manifestations of joint damage in rheumatoid arthritis.
| Collagen Type | Location | Primary Function |
|---|---|---|
| Type I | Bones, skin, tendons | Strength and structural support |
| Type II | Cartilage | Flexibility and cushioning |
| Type III | Skin, blood vessels, organs | Supporting structure |
| Type IV | Basement membranes | Support and filtration |
Impact of Collagen Supplements on Joint Health
Illustrative diagrams showcasing the potential impact of collagen supplements on joint health are valuable. These diagrams could depict collagen synthesis and how collagen supplements might support this process. They could also show how the collagen might reinforce damaged cartilage and ligaments, potentially leading to reduced pain and improved joint function. A flowchart demonstrating the potential pathway from collagen supplementation to improved joint health would be helpful.
The diagrams could also highlight the importance of a balanced approach to joint health, emphasizing the role of exercise, diet, and lifestyle modifications in conjunction with supplements.
Summary
In conclusion, collagen supplementation emerges as a potentially promising avenue for managing rheumatoid arthritis symptoms, but more research is needed to fully understand its effectiveness and optimal application. While promising, the potential benefits must be weighed against the potential limitations and potential side effects. Ultimately, integrating collagen supplementation into a comprehensive rheumatoid arthritis management plan, guided by a healthcare professional, may be a worthwhile consideration for individuals seeking alternative or complementary therapies.
Further research and clinical trials are crucial to solidify the place of collagen supplements in the treatment arsenal for rheumatoid arthritis.




