How to check your IUD strings is a crucial aspect of IUD care. This guide provides a comprehensive overview, from understanding the purpose and appearance of IUD strings to identifying potential issues and knowing when to seek professional help. We’ll cover everything from self-assessment techniques to recognizing normal versus abnormal findings, empowering you to maintain your IUD’s proper function and well-being.
This detailed guide walks you through the steps of checking your IUD strings, providing clear instructions and helpful visuals. Learning how to check your IUD strings is a key part of responsible IUD use, allowing you to monitor its placement and condition effectively.
Introduction to IUD Strings
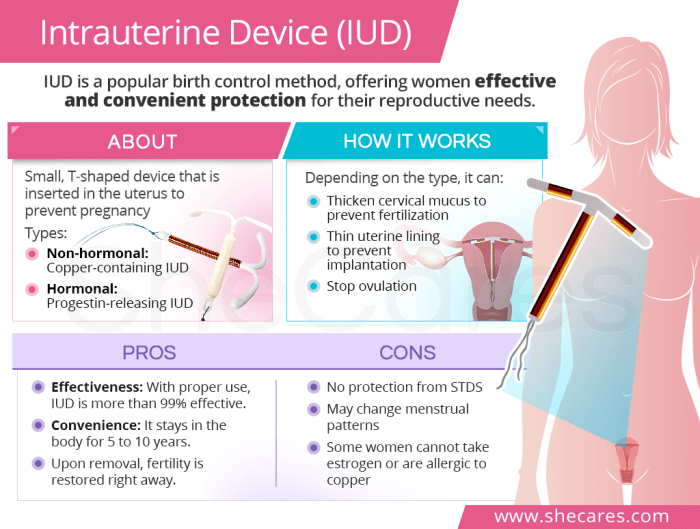
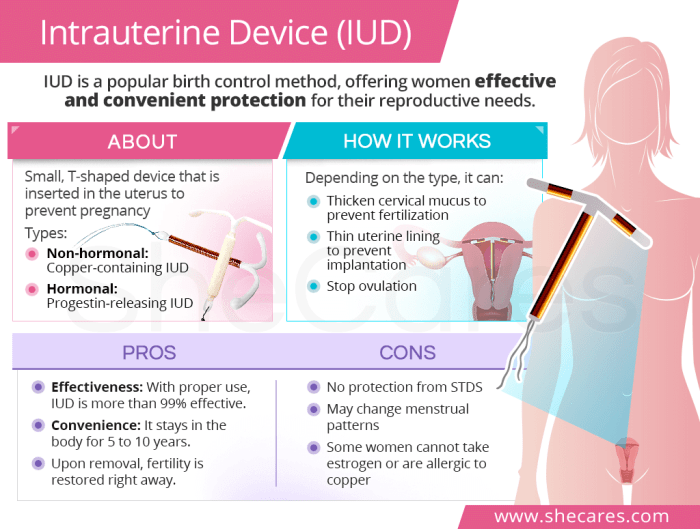
Intrauterine devices (IUDs) are small, T-shaped devices inserted into the uterus to prevent pregnancy. They work by creating a hostile environment for sperm or by preventing implantation of a fertilized egg. A crucial component of IUDs are the strings, thin threads attached to the device. These strings are essential for checking the placement and proper functioning of the IUD.The strings serve as a visual cue for confirming the IUD is in place within the uterus.
They also allow healthcare providers to remove the IUD when desired. Proper understanding of IUD strings is vital for both patients and healthcare professionals to ensure effective and safe contraception.
IUD String Appearance and Characteristics
IUD strings typically range in length and color, varying depending on the type of IUD. They are designed to protrude slightly from the cervix, making them accessible for checking at home. The strings should generally feel smooth and consistent. Any noticeable abnormalities in the strings or discomfort should be reported to a healthcare provider immediately.
Types of IUDs and Their Strings
Understanding the differences in IUD strings helps individuals identify their specific device and monitor its position correctly. Different IUDs have unique characteristics to aid in proper identification and maintenance.
| IUD Type | String Length (approximate) | String Color |
|---|---|---|
| ParaGard (Copper IUD) | 2-4 cm | Thin, light blue |
| Mirena (Hormonal IUD) | 2-4 cm | Thin, light purple |
| Skyla (Hormonal IUD) | 2-4 cm | Thin, light teal |
| Liletta (Hormonal IUD) | 2-4 cm | Thin, light yellow |
| Kyleena (Hormonal IUD) | 2-4 cm | Thin, light green |
Note: String length and color may vary slightly between manufacturers and individual IUDs. Always consult your healthcare provider for specific information about your IUD.
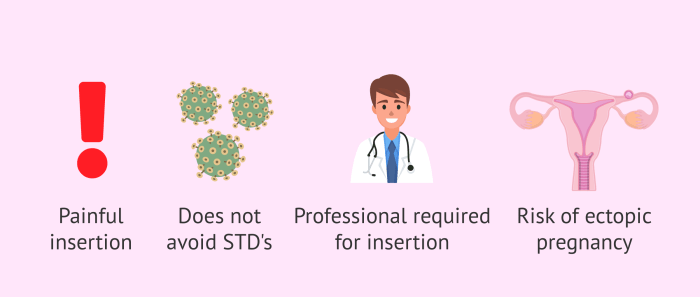
Checking your IUD strings is a straightforward process, but it’s important to remember that sometimes, things aren’t as they seem. For instance, noticing some unusual discharge or pain doesn’t automatically mean infidelity. It’s crucial to understand that STIs aren’t always a sign of infidelity, and getting tested regularly is key. STD’s aren’t always a sign of infidelity.
So, if you’re unsure about your IUD strings, consult your healthcare provider for guidance on proper checking techniques and any potential concerns. Knowing how to check your IUD strings is important for peace of mind and early detection of any problems.
Identifying IUD Strings
Finding your IUD strings is a crucial step in ensuring your device is properly positioned and functioning as intended. This process is typically straightforward, but understanding the steps and potential obstacles can ease any anxieties. Knowing how to locate your strings can help you feel more confident and empowered in managing your reproductive health.Locating your IUD strings should be done with a trusted friend or partner, or ideally, with a healthcare professional, if you feel uncomfortable or unsure.
Never attempt to locate the strings alone if you are not confident in the procedure. This process is about ensuring your well-being, and safety is paramount.
Methods for Locating IUD Strings
Locating IUD strings can be achieved through various methods, each with its own advantages and disadvantages. The most common and usually effective techniques are described below. It’s important to approach each method with care and attention to detail.
Visual Inspection
Visual inspection is often the first method employed. Using a mirror, you can often see the strings in the vaginal canal. The strings usually extend from the cervix and appear as small, thin threads. The lighting and angle of the mirror can significantly impact visibility. Practice in a well-lit area, and if you are still unsure, consult a healthcare professional.
Digital Examination
A digital examination involves gently inserting a finger into the vagina. This method can provide a better feel for the strings, as you can directly locate and trace them with your fingers. The sensitivity of this technique may vary depending on the individual, but with practice, it can be a reliable method. A trusted partner or healthcare provider can assist in this method if you feel uncomfortable performing it alone.
Be sure to keep your finger clean and apply pressure gently.
Comparison Table of Methods, How to check your iud strings
| Method | Advantages | Disadvantages |
|---|---|---|
| Visual Inspection | Simple and often the first step. Relatively easy to perform. | Limited visibility depending on the angle and lighting. May not be effective in all cases. |
| Digital Examination | Provides a more tactile sense of the strings. Allows for direct location and tracing. | May be uncomfortable for some individuals. Requires practice and potential for error if performed without experience. |
Potential Obstacles
Several factors can make locating IUD strings challenging. These include:
- String Position: The strings might be positioned deep within the vagina, or tucked against the cervix, making them difficult to see or feel. Some strings are more easily located than others. It may take practice to find the correct location.
- Vaginal Tightness: If the vaginal walls are tight, it may be harder to visualize or feel the strings. This can be due to various factors, such as anxiety, discomfort, or certain medical conditions. Practice and relaxation techniques can be helpful.
- Discomfort or Pain: If you experience pain or discomfort during the process, stop immediately. It is not worth the risk of causing further discomfort or harm. A healthcare professional can help in such situations.
Safety Precautions
Safety is paramount during the process of locating IUD strings. Follow these steps:
- Cleanliness: Ensure your hands and any tools used are clean before attempting to locate the strings. Hygiene is important to prevent infections.
- Gentle Handling: Avoid forceful or rough handling of the vaginal area. Gentle movements and care are crucial to avoid discomfort and injury.
- Seeking Professional Help: If you are unable to locate the strings, or if you experience any pain or discomfort, contact a healthcare professional immediately.
Checking for String Length and Condition: How To Check Your Iud Strings
Regularly checking your IUD strings is crucial for ensuring your device remains correctly positioned and functioning as intended. This involves assessing both the length and condition of the strings, which can indicate potential issues or displacement. Understanding these aspects empowers you to address any concerns promptly and maintain your reproductive health.Proper string management is essential for early detection of potential problems.
Variations in string length or damage can signal that the IUD has shifted or may be at risk of expulsion. Knowing how to evaluate your strings allows for proactive measures, preventing potential complications and promoting peace of mind.
Determining Appropriate String Length
String length is a vital indicator of the IUD’s position within the uterus. An IUD with properly positioned strings will generally maintain a consistent length, though there may be slight variations. It’s essential to understand the typical range and the potential reasons for deviations. The string length should generally match what was observed during the initial insertion.
Potential Reasons for String Length Variations
Several factors can contribute to variations in string length. The IUD may have shifted slightly within the uterus, or there may be some degree of normal variation depending on the specific type of IUD. Changes in string length can be attributed to factors like body weight, the amount of menstrual flow, or the presence of certain medical conditions.
These factors should be noted and, if any concerns arise, a consultation with a healthcare provider is recommended.
Assessing String Condition
Regularly inspecting the condition of your IUD strings is essential for maintaining its efficacy and identifying any potential problems. Visual examination for cleanliness and signs of damage is key to proactive health management.
Procedure for Assessing String Condition
To assess the condition of the IUD strings, gently grasp the strings and examine them for any signs of damage, such as cuts, tears, or fraying. Look for any signs of unusual discoloration or excessive discharge, which may indicate an infection or other issues. Inspect the strings for cleanliness, ensuring they are free from any visible debris or secretions.
If you notice any irregularities, document them for discussion with your healthcare provider.
Handling Strings That Are Too Short, Too Long, or Damaged
If you find that the strings are significantly shorter than expected, this could indicate the IUD has shifted or is dislodged. Likewise, excessively long strings might also suggest the IUD is not positioned correctly. If the strings appear damaged or dirty, it could signal an infection or other complications. In any of these cases, it’s crucial to consult your healthcare provider immediately for evaluation and appropriate management.
Do not attempt to adjust or remove the IUD yourself.
Checking your IUD strings is a pretty straightforward process. Just gently place one finger inside your vagina and feel around for the strings. You’ll likely find them pretty quickly. Knowing the best time to take collagen supplements can really impact how your body absorbs them, and some people prefer to take them with meals for optimal results.
This article on the best time to take collagen might give you some good tips on that front. Once you’ve found the strings, you can give them a little tug to make sure they’re still secure. Remember, if you have any concerns, it’s always best to consult your doctor.
Understanding Normal vs. Abnormal Findings

Knowing the difference between normal and abnormal IUD string characteristics is crucial for your well-being. Regular checks can help you identify potential issues early, allowing for prompt medical attention if needed. This section will detail the normal appearance of IUD strings and common indicators of problems. It’s essential to understand that this information is for educational purposes only and should not be substituted for professional medical advice.Identifying potential problems early can significantly impact your health and peace of mind.
A simple, regular check can often make the difference between a minor issue and a more serious concern.
Normal IUD String Characteristics
Regular checks for your IUD strings are vital for ensuring your health and safety. Normal IUD strings typically appear as thin, light-colored threads. The length and position of these threads can vary depending on the type of IUD and individual anatomy. Their appearance should generally be consistent with the initial assessment.
Abnormal IUD String Characteristics
Abnormal IUD string characteristics can signal potential problems. These may include noticeable changes in the appearance of the strings or the presence of unusual sensations. It’s important to recognize these indicators and seek medical attention if you observe any concerning signs.
Indicators of Potential Problems
Several indicators may suggest potential issues with your IUD. These could include:
- Strings that are longer, shorter, or have changed in color or texture compared to your previous checks.
- Strings that are visibly dislodged or out of position, potentially indicating IUD displacement.
- Strings that are painful or tender to the touch.
- Strings that appear knotted, or entangled.
- Strings that are accompanied by unusual discharge, pain, or fever.
Importance of Seeking Medical Advice
Any unusual changes or discomfort related to your IUD strings should prompt immediate consultation with a healthcare provider. Don’t hesitate to reach out for clarification. Early intervention can prevent complications and ensure the proper functioning of your IUD.
Comparison of Normal and Abnormal IUD String Conditions
The following table contrasts normal and abnormal IUD string conditions. This table provides a helpful guide to recognizing potential issues.
| Characteristic | Normal | Abnormal |
|---|---|---|
| String Appearance | Thin, light-colored threads, consistent with initial assessment. | Longer, shorter, changed color, texture, knotted, or entangled. |
| String Position | In place, consistent with initial assessment. | Dislodged, out of position, or noticeably shifted. |
| Discomfort | No pain, tenderness, or unusual sensations. | Pain, tenderness, or unusual sensations (e.g., sharp pain, unusual discharge). |
| Discharge | No unusual discharge. | Unusual discharge (e.g., foul-smelling, excessive). |
| Fever | Absence of fever. | Presence of fever. |
Seeking Professional Medical Advice
Knowing your IUD strings is a crucial part of IUD care, but there are times when things aren’t quite right. If you notice any unusual changes or concerns, seeking guidance from a healthcare professional is essential. Ignoring potential issues can lead to complications and discomfort.Professional evaluation is vital for ensuring the well-being of the individual and the proper functioning of the IUD.
A healthcare provider can accurately assess the situation, rule out any underlying problems, and provide personalized recommendations. This is particularly important if you’re experiencing pain, unusual discharge, or if the strings are shorter, longer, or feel different than expected.
Importance of Professional Evaluation
Proper evaluation by a healthcare professional is important for confirming the presence of IUD strings and their proper placement within the uterus. They can also diagnose potential issues, such as infection, perforation, or displacement of the IUD. Addressing concerns promptly is crucial to prevent complications.
Information to Share with Your Doctor
When discussing your IUD strings with your doctor, provide detailed information about your concerns. This includes:
- Specific details about the changes you’ve noticed (e.g., string length, color, feel, presence of discharge, any pain).
- Timing of the changes (e.g., when did you first notice the issue?).
- Any associated symptoms (e.g., pain, fever, unusual discharge).
- Your medical history, including any pre-existing conditions or allergies.
- All medications and supplements you are currently taking.
Accurate and comprehensive information allows your doctor to make an informed assessment and develop an appropriate treatment plan.
Questions to Ask Your Healthcare Provider
Discussing concerns with a healthcare professional is a proactive step in ensuring the well-being of the individual.
- Are the changes in my IUD strings something I should be concerned about?
- What are the possible causes for these changes?
- What are the appropriate steps to take, and what is the best course of action?
- Are there any potential complications or risks associated with the current state of my IUD?
- What are the signs of infection or other issues related to my IUD? What are the appropriate treatment options if I need them?
- What are the expected outcomes and the timeline for resolving the issue?
Prevention of IUD String Issues
Maintaining the proper placement and condition of your IUD strings is crucial for continued safety and effectiveness. Regular checks and preventative measures can minimize potential complications. By understanding the importance of these practices, you can ensure your IUD remains optimally functioning.Understanding potential risks and proactive measures to mitigate them is key to a comfortable and worry-free experience with an IUD.
Checking your IUD strings can be a little tricky, but it’s important for peace of mind. First, find a comfortable position, like lying down or sitting up straight. Gently feel around the cervix for the strings, which should be thin and slightly raised. While you’re learning about IUDs, it’s interesting to see recent studies, like this one on olive oil and dementia risk, which has some fascinating findings.
olive oil and dementia risk study. Ultimately, though, if you’re unsure or have any concerns, always consult your doctor for personalized advice on checking your IUD strings.
This includes knowing how to spot potential problems and how to take preventative steps.
Regular Check-Ups with Healthcare Providers
Regular check-ups with your healthcare provider are essential for the well-being of your IUD. These visits allow for professional assessments of the IUD’s position and the condition of the strings. Early detection of any issues can prevent potential complications. Your healthcare provider can also address any concerns or questions you may have.
Maintaining Proper IUD Placement
Proper IUD placement is vital to prevent string issues. This involves understanding how your IUD is situated within your uterus and how the strings are positioned relative to your cervix. Following your healthcare provider’s instructions regarding activities and avoiding heavy lifting or strenuous exercise immediately after insertion is a crucial step.
Avoiding Potential Complications
Certain activities or behaviors can increase the risk of dislodging the IUD or causing issues with the strings. Avoiding activities that could put excessive pressure on your abdomen, such as heavy lifting or intense exercise shortly after insertion, can help prevent string issues. Additionally, maintaining good hygiene practices around the insertion site can help reduce the risk of infection.
Self-Checking IUD Strings: A Step-by-Step Procedure
Performing a self-check of your IUD strings is an important part of proactive health management. This can be done in the privacy of your own home. It’s important to note that this is not a substitute for professional medical advice. If you notice anything unusual, consult your healthcare provider immediately.
- Gather Supplies: A mirror or a light source (such as a handheld mirror) and a relaxed environment.
- Positioning: Gently lie down or sit in a comfortable position that allows you to see the area clearly.
- Visual Inspection: Use the mirror or light source to carefully examine the strings. Look for any signs of shortening, lengthening, or changes in the strings’ overall condition. Observe the strings for any unusual discharge, discoloration, or pain.
- Record Observations: Note any specific changes or concerns. Keep a record of your observations for future reference and to share with your healthcare provider.
- Consult with Healthcare Provider: If you notice anything unusual, consult your healthcare provider immediately.
Self-Assessment Techniques
Checking your IUD strings at home can provide peace of mind and early detection of potential issues. However, it’s crucial to understand that self-assessment is not a substitute for regular check-ups with your healthcare provider. Accurate identification of IUD string conditions requires a professional evaluation. This section details self-assessment methods, emphasizing the importance of proper technique and limitations.Performing self-assessment of IUD strings requires careful attention to detail and awareness of potential variations.
It is essential to approach this process with respect for your body and a clear understanding of the limitations of home evaluations. Remember, if you experience any discomfort, unusual discharge, or concerns about your IUD, consult your healthcare provider immediately.
Methods for Checking IUD Strings
Proper technique is key to a safe and effective self-assessment. Avoid forceful probing or manipulation. Instead, focus on gentle exploration and observation. The goal is to identify the strings, not to reposition the IUD.
Positions for Self-Assessment
Different positions can offer better access to the IUD strings. Proper positioning ensures visibility and comfort throughout the procedure.
| Position | Description | Advantages | Disadvantages |
|---|---|---|---|
| Lying Down | Lie on your back with your knees bent. This position allows for a clear view of the vaginal area. | Excellent visibility, relaxed muscles. | May require a mirror or other aid to see clearly. |
| Standing or Sitting with Legs Apart | Stand or sit with your legs spread slightly apart. This can provide better access, especially for those with good body awareness. | Easy to perform, accessible to many. | May be more difficult to fully visualize depending on the angle and vaginal anatomy. |
| Using a Speculum (with guidance) | A speculum, when used correctly under the guidance of a healthcare professional, can assist with string visibility. Avoid using a speculum without direct professional guidance. | Provides a clear view, useful for examining other vaginal health conditions. | Requires training and supervision, should only be used under professional guidance. |
Accuracy in Self-Assessment
Proper identification of IUD strings requires patience and attention to detail. Avoid rushing the process. Gentle exploration, with adequate lighting, ensures accurate observation. If you have any doubt about the location or condition of your strings, seek immediate medical advice.
Visual Aids and Illustrations
Understanding your IUD strings visually is crucial for identifying potential problems. This section provides clear visuals and descriptions to help you recognize normal and abnormal string appearances. Knowing these cues empowers you to take proactive steps and seek necessary medical attention if needed.
Finding IUD Strings: Visual Cues
Locating your IUD strings can be easier with the right visual cues. Look for small, thin threads protruding from your cervix. They may be a light or dark color depending on the string material. If you’re unsure of the exact location, try tilting your body slightly forward or leaning back. Good lighting is essential, and a mirror may be helpful for a clear view.
If you still have trouble finding them, consider asking a trusted friend or family member for assistance. Their fresh perspective might help you locate them more easily.
IUD String Conditions: Visual Appearance
Different conditions can affect the appearance of your IUD strings. Normal strings should be smooth, consistent in thickness, and not visibly frayed or knotted. Shortened or significantly thickened strings might indicate a potential problem. Similarly, unusual string colors, like discoloration or an unexpected change, should prompt further evaluation. For example, if your strings appear longer than normal, they may be twisted or tangled.
A sudden change in the length or texture of your strings could be a sign that something is amiss.
Anatomy of the Female Reproductive System with IUD Location
The female reproductive system is complex. The uterus, a pear-shaped organ, is situated in the pelvis. The cervix, a narrow opening at the bottom of the uterus, leads to the vagina. The IUD is placed inside the uterus, often positioned within the uterine cavity. The strings of the IUD extend through the cervix and project into the vagina.
Visualizing the IUD’s position within the uterus can be helpful in understanding string location. Detailed anatomical diagrams can provide a clearer view of the reproductive organs and the IUD’s placement.
IUD String Positions and Potential Problems: Diagram
The following table illustrates different string positions and potential issues:
| String Position | Description | Potential Problems |
|---|---|---|
| Strings extending beyond the vaginal opening | Strings are visibly long and extending outside the vaginal opening. | Possible expulsion of the IUD, or strings may be twisted or tangled. |
| Strings are tangled or knotted | Strings are intertwined or knotted together. | Difficulty in checking the strings and possible expulsion. |
| Strings are noticeably shorter than usual | Strings appear shorter than expected, perhaps unevenly short. | Possible IUD migration or expulsion. |
| Strings are visibly frayed or broken | Strings show visible damage, such as fraying or breakage. | Possible IUD damage, potentially needing removal. |
| Strings are unusually thick or thin | Strings exhibit an unusual thickness compared to their typical appearance. | Potential for IUD damage or displacement. |
Note: These are examples. If you notice any changes, consult your healthcare provider.
Closing Notes
In summary, checking your IUD strings is a vital part of maintaining your reproductive health. This guide has equipped you with the knowledge and steps needed for a safe and effective self-assessment. Remember, regular check-ups with your healthcare provider are essential, and if you have any concerns or notice anything unusual, don’t hesitate to seek professional medical advice.
By following the steps Artikeld here, you can effectively monitor your IUD and ensure its continued proper functioning.