Medications for crohns disease – Medications for Crohn’s disease are a crucial aspect of treatment, and understanding the various options available can be empowering for patients. This guide delves into the different types of medications used, their mechanisms of action, potential side effects, and important considerations for selection. We’ll explore everything from the basics of Crohn’s disease to cutting-edge treatments, offering a comprehensive overview for better understanding and informed decision-making.
Crohn’s disease, a chronic inflammatory condition, affects the digestive tract. Different medications target various aspects of the disease, from reducing inflammation to modulating the immune response. This guide aims to provide a clear and concise overview of these medications, helping you navigate the complexities of treatment options.
Overview of Crohn’s Disease Medications: Medications For Crohns Disease
Crohn’s disease is a chronic inflammatory condition affecting the digestive tract. It can cause a range of symptoms, from mild discomfort to severe complications, impacting quality of life significantly. The inflammation can occur anywhere along the digestive system, from the mouth to the anus, leading to unpredictable and often debilitating symptoms. Understanding the different medications available is crucial for managing this complex disease.Crohn’s disease treatment focuses on controlling inflammation, reducing symptoms, and preventing complications.
Various medications target different aspects of the disease process, with a personalized approach crucial to effective management. The choice of medication often depends on the severity of the disease, the location of inflammation, and the patient’s response to previous treatments.
Managing Crohn’s disease often involves a cocktail of medications, each tailored to individual needs. While researching different treatment options, I stumbled upon an interesting article about how medications like symbicort, dulera, advair, and breo are used to treat asthma. symbicort dulera advair and breo to treat asthma This made me think about the potential overlaps in the way the body responds to these different types of medications, and how that might translate to developing similar treatment approaches for Crohn’s disease in the future.
Ultimately, finding the right medication for Crohn’s is a personalized journey, and more research is always helpful.
Medication Categories for Crohn’s Disease
Different types of medications are used to treat Crohn’s disease, each targeting specific aspects of the inflammatory response. These are broadly categorized based on their mechanism of action. This helps clinicians tailor treatment strategies effectively.
Anti-inflammatory Medications
These medications aim to reduce inflammation in the digestive tract. Corticosteroids, such as prednisone, are potent anti-inflammatory drugs often used to quickly suppress inflammation, but their long-term use can lead to significant side effects. Aminosalicylates, like mesalamine, are frequently used for milder cases, targeting the inflammation directly in the affected areas. These are often used in combination with other medications.
Immunomodulators
These medications work by modulating the immune system, which plays a crucial role in Crohn’s disease. Examples include azathioprine and 6-mercaptopurine. They are typically used for more severe or persistent cases that don’t respond well to other treatments. These medications often take several weeks or months to show their full effect, and their side effects can vary depending on the individual.
Biologics
Biologics are a more recent class of medications targeting specific components of the immune system involved in Crohn’s disease. These include TNF inhibitors (e.g., infliximab, adalimumab) and others targeting specific immune pathways. They are often used for severe cases that haven’t responded to other treatments. Biologics can be very effective in controlling inflammation and improving symptoms but are associated with potential risks, including infections.
Table Comparing Medication Classes
| Medication Class | Mechanism of Action | Typical Dosage Range | Common Side Effects |
|---|---|---|---|
| Corticosteroids (e.g., Prednisone) | Potent anti-inflammatory; suppress immune response. | 5-60 mg/day (initially), tapered gradually. | Increased appetite, weight gain, mood changes, osteoporosis, increased risk of infection. |
| Aminosalicylates (e.g., Mesalamine) | Reduce inflammation directly in the colon. | 1-4 g/day, varying forms (rectal, oral). | Nausea, abdominal pain, headache, allergic reactions. |
| Immunomodulators (e.g., Azathioprine) | Modulate immune response, slow-acting. | 1-3 mg/kg/day. | Nausea, vomiting, diarrhea, liver problems, risk of infections. |
| Biologics (e.g., Infliximab) | Target specific immune components involved in inflammation. | Initial high dose, then maintenance doses. | Infections (including reactivation of latent infections), allergic reactions, injection site reactions. |
Specific Medication Types
Understanding the various medications used in Crohn’s disease management is crucial for patients and healthcare providers. Different medications target specific aspects of the disease, offering tailored approaches to symptom control and disease management. This section will delve into the mechanisms of action and roles of key medication types, including aminosalicylates, corticosteroids, and immunomodulators.
Aminosalicylates
Aminosalicylates are a class of medications that work by reducing inflammation in the digestive tract. They are often the first-line treatment for mild to moderate Crohn’s disease. These drugs, such as mesalamine, work by interfering with the inflammatory process. They primarily target the colon and rectum, though some preparations can be used for the small intestine. Their mechanism of action involves decreasing the production of inflammatory mediators and reducing the infiltration of immune cells into the inflamed tissue.
Aminosalicylates are generally well-tolerated, but some patients may experience side effects like abdominal pain, nausea, or diarrhea.
Corticosteroids
Corticosteroids are potent anti-inflammatory medications that can rapidly suppress inflammation. Their use in Crohn’s disease is primarily for short-term symptom management. They are effective in reducing inflammation and alleviating symptoms like abdominal pain, diarrhea, and fever. Their rapid anti-inflammatory action makes them crucial in managing acute flares or severe disease exacerbations.
Short-Term Effects of Corticosteroids
Corticosteroids can effectively reduce inflammation, leading to a rapid improvement in symptoms. They can help control acute flares, enabling patients to recover more quickly and allowing for other treatment options to be introduced. However, their short-term use does not cure the underlying disease.
Long-Term Effects of Corticosteroids
Long-term use of corticosteroids carries significant risks. These risks include increased susceptibility to infections, osteoporosis, and a higher risk of developing cataracts. Also, prolonged use can lead to the suppression of the body’s natural immune response, making patients more vulnerable to illnesses. Therefore, corticosteroids are typically used for short-term periods and in conjunction with other treatments.
Immunomodulators
Immunomodulators are a category of medications that modify the immune system’s response to inflammation. These drugs are often used for long-term management of Crohn’s disease when other therapies are not effective or when the disease is severe. Their role is to regulate the overactive immune response that contributes to the inflammation in Crohn’s disease. By modifying the immune system’s activity, immunomodulators aim to reduce inflammation and improve disease control.
The specific mechanisms of action vary among different immunomodulators.
Immunomodulator Types and Comparison
| Immunomodulator | Mechanism of Action | Benefits | Risks |
|---|---|---|---|
| Azathioprine | Suppresses immune cell activity. | Effective in maintaining remission, reducing inflammation. | Potential for liver damage, blood disorders, infections. |
| Methotrexate | Inhibits cell growth and immune responses. | May improve symptoms, maintain remission. | Potential for liver damage, lung problems, allergic reactions. |
| 6-mercaptopurine | Interferes with immune cell development and function. | Can be effective in maintaining remission. | Potential for liver damage, blood disorders, infections. |
| Infliximab | Targets TNF-alpha, a key inflammatory molecule. | Highly effective in reducing inflammation and improving symptoms in many cases. | Increased risk of infections, allergic reactions, and potential for reactivation of latent infections. |
Biologics and Targeted Therapies
Biologics and targeted therapies represent a significant advancement in Crohn’s disease treatment. These medications act on specific parts of the immune system, aiming to reduce inflammation and improve symptoms without the broad effects of some older therapies. This approach often leads to better outcomes and fewer side effects in many patients.These medications work by modulating the immune response in a more precise manner than traditional therapies.
This targeted approach often results in fewer side effects and a more favorable therapeutic index. By understanding how these medications work, patients and healthcare providers can make informed decisions about the best treatment strategy for individual needs.
Mechanism of Action of Biologics
Biologics, such as anti-TNF agents, are designed to target specific inflammatory pathways. These proteins, often derived from living organisms, interfere with the activation of immune cells that cause inflammation in the digestive tract. This targeted approach often reduces the severity and frequency of inflammatory flare-ups, leading to improved quality of life. For example, anti-TNF agents, like infliximab, block tumor necrosis factor-alpha (TNF-α), a protein crucial in inflammation.
This blockade reduces the inflammatory cascade, leading to symptom relief.
Specific Examples of Biologics in Crohn’s Disease
Several biologics are approved for Crohn’s disease treatment, each with a slightly different mechanism of action and potential side effect profile. A common class of biologics are anti-TNF agents, which block TNF-α, a key inflammatory molecule. Other biologics target different immune system pathways, like interleukin-12/23 (IL-12/23) inhibitors, or T-cell receptors.
Advantages and Disadvantages of Biologics
Biologics offer several advantages over traditional therapies. Their targeted approach often results in fewer side effects and improved efficacy compared to older treatments. They can effectively reduce inflammation and improve quality of life for many patients. However, biologics are typically more expensive than traditional therapies, and some patients may experience adverse reactions. Furthermore, the need for repeated injections or infusions can be inconvenient for some individuals.
The effectiveness and safety of biologics can vary among patients, and careful monitoring is essential.
Comparison of Biologics
| Biologic | Mechanism of Action | Effectiveness (Typical Outcomes) | Side Effect Profile |
|---|---|---|---|
| Anti-TNF agents (e.g., infliximab, adalimumab) | Block TNF-α, a key inflammatory molecule. | Generally high; effective in inducing and maintaining remission in many patients. | Infusion reactions, increased risk of infections, and rare but serious side effects like demyelinating disorders. |
| IL-12/23 inhibitors (e.g., ustekinumab) | Block IL-12 and IL-23, which play a role in immune cell activation. | Often effective in inducing and maintaining remission. | Injection site reactions, upper respiratory tract infections, and headache. |
| Anti-integrins (e.g., vedolizumab) | Target integrins, which are involved in immune cell migration to the gut. | Effective in reducing inflammation and improving symptoms in many patients. | Injection site reactions, headache, and, less commonly, severe allergic reactions. |
Medication Selection and Considerations
Choosing the right Crohn’s disease medication is a crucial step in managing the condition effectively. It’s not a one-size-fits-all approach, as each individual’s response to different treatments varies significantly. Factors like disease severity, location, and personal health history play a critical role in determining the most suitable medication strategy.Understanding the unique needs of each patient is paramount. A tailored approach, considering the individual’s response to previous treatments and overall health status, is essential for achieving optimal outcomes.
This personalized strategy aims to minimize side effects and maximize the medication’s effectiveness.
Individual Patient Needs and Responses
Individualized treatment plans are essential in Crohn’s disease management. Each patient’s body reacts differently to various medications. Factors like age, pre-existing conditions, and other medications taken concurrently significantly influence the efficacy and safety of a treatment. For example, a patient with kidney disease might require a different dosage or a completely different medication class compared to a younger patient with no other health concerns.
The patient’s response to initial therapy also guides subsequent choices.
Effectiveness of Different Medications for Various Disease Presentations
The effectiveness of a medication depends heavily on the specific presentation of Crohn’s disease. For instance, medications that target specific inflammatory pathways may be more effective in patients with ileal Crohn’s disease, while others might be more suitable for colonic disease. It’s crucial to consider the location and extent of inflammation when selecting a medication. Early intervention and aggressive treatment are often vital for patients with severe disease activity to prevent complications.
Managing Crohn’s disease with medications can be a real challenge, but finding the right approach is key. While dealing with the discomfort of Crohn’s, it’s also important to consider how other conditions might impact your daily life. For example, if you have fibromyalgia, exploring mobility aids like those discussed in this helpful article on mobility aids with fibromyalgia could significantly improve your quality of life.
Ultimately, the right combination of medications and supportive tools is crucial for effectively managing Crohn’s disease symptoms.
Role of Patient Education in Medication Adherence and Management
Patient education plays a vital role in successful medication management. Understanding the purpose, dosage, potential side effects, and importance of adherence to a treatment plan empowers patients to actively participate in their care. Clear communication between patients and healthcare providers regarding any concerns or side effects is essential. This fosters a collaborative approach that enhances medication adherence and improves treatment outcomes.
Potential Drug Interactions and Contraindications
Proper medication selection requires careful consideration of potential drug interactions and contraindications. These interactions can lead to adverse effects or diminish the effectiveness of the treatment. A thorough understanding of potential interactions is crucial for patient safety and optimal treatment outcomes.
| Drug A | Drug B | Potential Interaction | Contraindications |
|---|---|---|---|
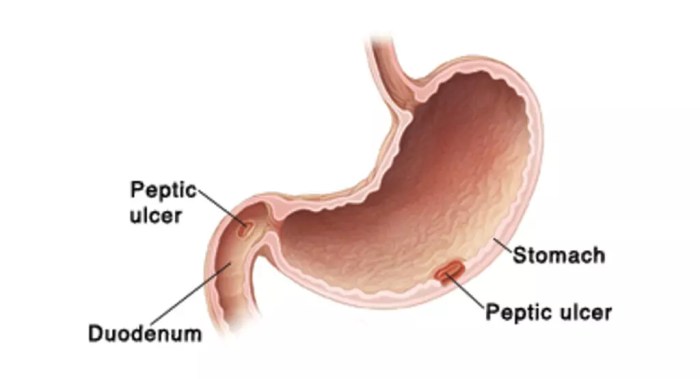
| Aminosalicylates | Corticosteroids | Increased risk of gastrointestinal irritation | Patients with active peptic ulcers or bleeding disorders |
| Methotrexate | Sulfasalazine | Increased risk of liver toxicity | Patients with pre-existing liver disease |
| Biologics | Immunosuppressants | Potential for increased risk of infections | Patients with a history of severe infections |
| Antibiotics | Steroids | Possible interference with steroid metabolism | Patients with known antibiotic allergies |
Potential Side Effects and Management
Living with Crohn’s disease often means navigating a complex landscape of medications, each with its own potential side effects. Understanding these potential reactions is crucial for effective management and communication with your healthcare team. This section will delve into common and severe side effects, strategies for management, and the importance of reporting any adverse reactions promptly.
Common Side Effects and Management Strategies
Managing potential side effects is an integral part of Crohn’s disease medication management. Understanding the spectrum of possible reactions allows for proactive measures to minimize discomfort and optimize treatment outcomes. A proactive approach, involving open communication with your doctor, can make a significant difference.
- Gastrointestinal Issues: Many medications can impact the digestive system, leading to nausea, vomiting, diarrhea, constipation, or abdominal pain. Dietary adjustments, such as avoiding trigger foods, and incorporating probiotics, may help alleviate these symptoms. Over-the-counter medications, like anti-diarrheal products, might be helpful in certain situations, but always consult your doctor first.
- Infections: Some medications, particularly biologics, can temporarily weaken the immune system, increasing the risk of infections. This is especially important to discuss with your healthcare provider to establish preventive measures and monitor for signs of infection.
- Skin Reactions: Skin rashes, itching, or hives are possible side effects. These reactions can range in severity, and prompt medical attention is necessary if they worsen.
- Fatigue: Many Crohn’s medications can cause fatigue as a side effect. Prioritizing rest and maintaining a balanced lifestyle can be helpful.
- Headaches: Headaches, including migraines, can sometimes be associated with some medications. Lifestyle adjustments, such as stress management techniques, and over-the-counter pain relievers, can be helpful, but consult your doctor for severe or persistent headaches.
Severe Side Effects and Reporting Procedures
Recognizing and reporting severe side effects is critical. Prompt intervention can prevent complications and potentially life-threatening situations. Always communicate any concerning symptoms to your doctor immediately.
- Severe allergic reactions (anaphylaxis): Characterized by difficulty breathing, swelling of the face and throat, and a rapid drop in blood pressure. This requires immediate medical attention. A severe allergic reaction is a medical emergency.
- Serious infections: Signs such as fever, chills, persistent fatigue, and unexplained pain can indicate a serious infection. These require immediate medical attention. Report any signs of infection to your doctor.
- Significant Liver or Kidney Issues: Some medications can impact liver or kidney function. Regular monitoring of liver enzymes and kidney function tests is often necessary. Any significant changes in these values should be reported to your healthcare provider immediately.
Table of Common Side Effects
This table provides a summary of common side effects, their severity, and management strategies.
| Side Effect | Severity (Mild, Moderate, Severe) | Management Strategies | Additional Notes |
|---|---|---|---|
| Nausea | Mild | Dietary changes, anti-nausea medications (consult your doctor) | Often temporary and manageable. |
| Diarrhea | Moderate | Dietary adjustments, over-the-counter anti-diarrheal medications (consult your doctor), fluid intake | Can lead to dehydration if severe. |
| Skin Rash | Mild to Moderate | Cooling compresses, over-the-counter anti-itch creams (consult your doctor), avoidance of potential allergens | May require discontinuation of the medication. |
| Fatigue | Mild to Moderate | Prioritize rest, maintain a balanced lifestyle, consider lifestyle changes | Can significantly impact daily life. |
Emerging Therapies and Future Directions
The journey to better Crohn’s disease management is constantly evolving, driven by innovative research and a deeper understanding of the disease’s complexities. New therapies are on the horizon, promising to improve treatment efficacy and minimize side effects for patients. This exploration delves into exciting advancements, from personalized medicine approaches to novel drug targets, and highlights the potential impact on future management strategies.
Promising New Developments
Researchers are actively investigating various novel approaches to treat Crohn’s disease, moving beyond traditional immunosuppressants and biologics. These developments encompass a broader range of targets within the disease’s intricate inflammatory pathways, with the goal of achieving more precise and effective therapies. This is reflected in a shift towards more targeted interventions that specifically address the underlying mechanisms driving inflammation in the gut.
Managing Crohn’s disease often involves a cocktail of medications, each with its own potential side effects. It’s a tough journey, but sometimes, the emotional toll can lead to coping mechanisms like skin picking, which can be linked to underlying autoimmune disorders, like those that can trigger Crohn’s. Understanding the connection between these behaviors and conditions is crucial, as it can inform better management strategies.
For a deeper dive into the interplay between skin picking and autoimmune disorders, check out this informative article: skin picking and autoimmune disorders. Ultimately, finding the right medication balance for Crohn’s disease requires a holistic approach that considers both physical and mental well-being.
Personalized Medicine Approaches
Personalized medicine, tailoring treatment strategies to individual patient characteristics, is gaining traction in Crohn’s disease management. This approach recognizes the heterogeneity of the disease, acknowledging that different patients respond differently to various treatments. Genetic testing and biomarker analysis are increasingly employed to identify specific genetic predispositions or immune system responses that can predict treatment response and potential side effects.
This precision approach aims to maximize efficacy while minimizing adverse events. For example, a patient with a specific genetic variant might be identified as more likely to respond positively to a certain biologic, while another might be better suited to a different therapy.
Impact on Future Management Strategies
The emergence of personalized medicine has the potential to revolutionize Crohn’s disease management. By enabling more accurate treatment selection and dosage adjustments, personalized approaches can lead to more effective therapies, fewer adverse effects, and improved long-term outcomes. This is crucial, as Crohn’s disease often requires lifelong treatment, making the ability to tailor therapy to individual needs a significant advancement.
Emerging Therapies and Their Potential Benefits and Risks
- Anti-inflammatory small molecules: These compounds are designed to target specific inflammatory pathways, potentially offering a more targeted approach compared to broader immunosuppressants. Benefits include the possibility of fewer side effects and improved efficacy. Risks include potential unknown long-term effects, and the need for further research to confirm efficacy and safety. These compounds are still in clinical trials, but their early promise is significant.
An example is a drug targeting a specific enzyme involved in inflammation.
- Immunomodulatory therapies: These therapies work by regulating the immune response, aiming to reduce inflammation without significantly suppressing the entire immune system. Benefits include a potential for improved control of disease activity and fewer side effects than traditional immunosuppressants. Risks are related to the potential for infections and other immune-related complications, but often these risks are mitigated through careful monitoring and appropriate patient selection.
- Novel biologics targeting specific inflammatory pathways: These biologics are designed to target specific inflammatory components within the immune system or gut. Benefits include a potential for more targeted inflammation reduction and fewer side effects compared to traditional biologics. Risks include the potential for rare but serious side effects related to immune system modulation, and the possibility of resistance to the therapy.
Medication Adherence and Patient Support

Taking Crohn’s disease medication as prescribed is crucial for managing symptoms, preventing flare-ups, and maintaining overall health. Consistent medication use helps to control inflammation and can significantly improve quality of life. However, adherence can be challenging for various reasons, including side effects, cost, and lifestyle factors. This section focuses on the importance of adherence, strategies to improve it, and available resources for patients.
Importance of Adherence
Medication adherence is paramount in Crohn’s disease management. Consistent medication use helps to control inflammation, reduce the frequency and severity of flare-ups, and prevent long-term complications. Non-adherence can lead to disease progression, increased hospitalizations, and a diminished response to treatment. This highlights the critical need for proactive strategies to support patients in adhering to their prescribed regimens.
Strategies to Improve Medication Adherence, Medications for crohns disease
Several strategies can help patients stay on track with their medication. Open communication with healthcare providers is essential. Discussing concerns, side effects, and potential barriers to adherence can help develop personalized strategies. Simplifying medication schedules, utilizing reminders (pill organizers, apps), and making the medication easier to take (e.g., liquid forms) can also be beneficial. Addressing cost concerns through financial assistance programs and exploring alternative medication options can also significantly improve adherence.
Resources Available for Patients
Numerous resources are available to support patients with Crohn’s disease and their medication regimens. Patient support groups and online forums provide opportunities to connect with others facing similar challenges. These communities offer emotional support, practical advice, and shared experiences, making the journey less isolating.
Patient Support Resources
- National Institutes of Health (NIH): Provides comprehensive information on Crohn’s disease, including treatment options and support resources.
- Crohn’s & Colitis Foundation of America (CCFA): Offers educational materials, support groups, and a helpline for patients and their families. Their website is a valuable resource for accessing information and support.
- Local Support Groups: Connecting with local support groups offers opportunities to meet people with similar experiences. These groups provide a safe space to share experiences and receive encouragement.
- Patient Advocacy Organizations: Organizations dedicated to Crohn’s disease and other digestive conditions offer resources and support networks.
- Online Forums and Social Media Groups: These platforms can connect patients with others experiencing similar issues, providing emotional support and practical advice.
- Pharmaceutical Companies: Many pharmaceutical companies offer patient assistance programs for medications, addressing cost concerns and improving adherence.
Illustrative Examples of Medication Regimens
Understanding the specific medication regimens for Crohn’s disease is crucial for effective management. Different individuals respond differently to treatments, and tailoring a regimen to the unique needs of each patient is paramount. This section provides illustrative examples of medication regimens, highlighting the rationale behind their use and how to explain them to patients in a clear and compassionate manner.
Typical Regimens for Mild Crohn’s Disease
Initial treatment for mild Crohn’s disease often focuses on lifestyle modifications, diet changes, and medications like aminosalicylates, such as mesalamine. These medications aim to reduce inflammation in the affected areas. For example, a patient with mild, localized ileitis might start with a mesalamine suppository or enema, along with a daily dose of oral mesalamine. This approach allows for a more targeted delivery of the medication to the inflamed area.
Explaining this to a patient should emphasize the potential for symptom improvement and the importance of consistent adherence to the regimen.
Regimens for Moderate Crohn’s Disease
When symptoms persist or worsen, a more intensive approach is needed. In moderate Crohn’s disease, a combination of medications may be necessary. A common regimen might include an aminosalicylate, like mesalamine, alongside a corticosteroid, like prednisone, to control inflammation. The corticosteroid is often used initially to rapidly reduce inflammation, while the aminosalicylate is used to maintain remission.
Patients need clear explanations of why these medications are being used together, the expected duration of corticosteroid use, and the potential for side effects. This approach needs careful monitoring and adjustment based on the patient’s response.
Regimens for Severe Crohn’s Disease
Severe Crohn’s disease, characterized by significant complications and systemic symptoms, often necessitates a more aggressive approach, including immunomodulators and biologics. For example, a patient experiencing severe ileocolitis might be started on an immunomodulator like azathioprine or 6-mercaptopurine in combination with a corticosteroid. If the response to these is insufficient, a biologic therapy, such as infliximab or adalimumab, may be considered.
The rationale behind these regimens needs to be clearly explained, highlighting the potential for significant improvement in symptoms and quality of life, while also addressing the potential for side effects. Close monitoring and communication are essential.
Table of Common Medication Regimens
| Stage/Severity | Medication(s) | Dosage | Rationale |
|---|---|---|---|
| Mild Crohn’s Disease | Mesalamine (oral or rectal) | Variable, based on severity and individual response | Reduces inflammation in the affected area |
| Moderate Crohn’s Disease | Mesalamine + Prednisone | Variable, based on severity and individual response | Reduces inflammation quickly with prednisone, maintained with mesalamine |
| Severe Crohn’s Disease | Immunomodulator (e.g., azathioprine) + Corticosteroid + Biologic (e.g., infliximab) | Variable, based on severity and individual response | Addresses severe inflammation and immune response. Biologics are added when other medications are insufficient. |
Final Summary
In conclusion, the management of Crohn’s disease involves a multifaceted approach, with medications playing a vital role. Understanding the diverse range of medications, their potential benefits and risks, and the importance of individual patient needs is essential. Remember, open communication with your healthcare provider is key to developing a personalized treatment plan that aligns with your specific needs and goals.
Continuous monitoring and adjustments are often necessary for optimal management. This comprehensive guide provides a foundation for informed discussions about medication choices, empowering patients to actively participate in their health journey.