Anti inflammatory diet for psoriasis – Anti-inflammatory diet for psoriasis is a powerful approach to managing this chronic skin condition. It’s not just about avoiding certain foods, but about understanding how your diet directly impacts inflammation and your psoriasis symptoms. This comprehensive guide explores the principles, food choices, and practical strategies to create a personalized anti-inflammatory eating plan. We’ll delve into the science behind the diet, share sample meal plans, and address common challenges, ultimately empowering you to take control of your psoriasis through mindful eating.
This guide will break down the specifics of an anti-inflammatory diet, detailing the impact of various food groups on your body’s inflammatory response. It will explore the connection between diet and psoriasis, providing practical strategies to navigate the complexities of managing the condition through your meals. We’ll examine the role of portion control, hydration, gut health, and stress management in the context of this approach.
Introduction to Anti-Inflammatory Diet for Psoriasis

An anti-inflammatory diet focuses on reducing inflammation throughout the body, which can positively impact various health conditions. It emphasizes whole, unprocessed foods rich in nutrients and antioxidants while minimizing pro-inflammatory ingredients. This approach aims to support overall well-being and potentially alleviate symptoms, especially in chronic conditions like psoriasis.The connection between diet and psoriasis is multifaceted. While the exact mechanisms aren’t fully understood, some studies suggest that certain foods can trigger or exacerbate inflammation in the body.
This inflammation can manifest as psoriasis flares, characterized by skin lesions and discomfort. An anti-inflammatory diet can potentially lessen these flares by reducing the overall inflammatory response.
General Principles of an Anti-Inflammatory Diet
This diet prioritizes nutrient-dense foods and minimizes processed foods, refined sugars, and unhealthy fats. It emphasizes the consumption of fruits, vegetables, whole grains, lean proteins, and healthy fats. Proper hydration is also crucial for overall health and reducing inflammation. By focusing on these principles, individuals can potentially support their body’s natural healing processes and reduce the impact of psoriasis.
Foods to Avoid
Processed foods, sugary drinks, and excessive intake of unhealthy fats are generally discouraged. These items often contain high levels of inflammatory agents, contributing to the overall inflammatory response in the body. Specific examples include refined carbohydrates like white bread and pasta, sugary cereals and snacks, and fried foods high in saturated and trans fats. Red meat, especially in large quantities, and excessive alcohol consumption should also be limited.
Foods to Include
A balanced diet rich in anti-inflammatory foods is essential. Fruits and vegetables are excellent sources of vitamins, minerals, and antioxidants, helping to combat inflammation. Leafy greens, berries, citrus fruits, and colorful vegetables are particularly beneficial. Whole grains provide complex carbohydrates and fiber, supporting digestive health and overall well-being. Lean proteins like fish, poultry, and beans offer essential amino acids without excessive saturated fat.
Healthy fats from avocados, nuts, and seeds are crucial for hormone production and overall health.
Sample Daily Meal Plan
| Meal | Description |
|---|---|
| Breakfast | Oatmeal with berries and nuts, a glass of water |
| Lunch | Grilled chicken salad with mixed greens, vegetables, and a light vinaigrette dressing |
| Dinner | Baked salmon with roasted vegetables (broccoli, carrots, and sweet potatoes) |
| Snacks | Fruits (apple, banana), handful of almonds, a small portion of Greek yogurt |
Specific Food Groups and Their Effects
Understanding the impact of different food groups on inflammation is crucial for managing psoriasis. This section delves into how various dietary components influence inflammation and, consequently, psoriasis symptoms. By identifying foods that promote inflammation and those that offer anti-inflammatory benefits, you can tailor your diet to better control your condition.Dietary choices play a significant role in modulating the body’s inflammatory response.
Certain foods can exacerbate inflammation, leading to increased psoriasis symptoms, while others possess anti-inflammatory properties that can help mitigate the condition. This section will highlight the effects of different food groups on inflammation and how these effects manifest in relation to psoriasis.
Fruits and Vegetables
Fruits and vegetables are rich in antioxidants and micronutrients that can help reduce inflammation throughout the body. They provide essential vitamins and minerals that support overall health, which in turn can positively influence psoriasis. Cruciferous vegetables, like broccoli and cauliflower, are particularly beneficial due to their high content of anti-inflammatory compounds. Berries, rich in antioxidants, are also known to contribute to a reduction in inflammation.
Proteins
Protein is essential for building and repairing tissues, and certain protein sources can impact inflammation. Lean proteins like fish, poultry, and beans are generally considered better choices for managing inflammation compared to processed meats. Fatty fish, such as salmon and tuna, are excellent sources of omega-3 fatty acids, known for their potent anti-inflammatory effects. Red meat, on the other hand, may contribute to inflammation in some individuals.
An anti-inflammatory diet can really help manage psoriasis symptoms. It’s all about reducing inflammation throughout your body, and that can impact everything from skin issues to, say, allergic reactions on your face, like those pesky breakouts. Understanding how certain foods trigger these reactions, as detailed in this article about allergic reaction on face , is key to finding a diet that works for you.
Ultimately, an anti-inflammatory diet is a powerful tool for controlling psoriasis.
Grains
Whole grains, like brown rice and quinoa, offer fiber and nutrients that can help regulate blood sugar and reduce inflammation. Processed grains, often high in refined carbohydrates, can increase blood sugar levels and potentially contribute to inflammation. Choose whole grains over refined grains whenever possible.
Dairy
Dairy products contain calcium and vitamin D, crucial for bone health. However, dairy can trigger inflammation in some individuals, potentially exacerbating psoriasis symptoms. If you suspect dairy is a trigger for your psoriasis, consider limiting or eliminating dairy products from your diet and monitoring the impact on your condition.
Fats
Different types of fats have varying effects on inflammation. Unsaturated fats, particularly omega-3 fatty acids found in fatty fish, are known for their anti-inflammatory properties. Saturated fats, often found in red meat and processed foods, may increase inflammation. Trans fats, present in many processed foods, are also linked to increased inflammation and should be minimized.
| Food Group | Anti-inflammatory Foods | Pro-inflammatory Foods |
|---|---|---|
| Fruits | Berries, Apples, Bananas | Processed fruit juices |
| Vegetables | Leafy greens, Broccoli, Cauliflower | Processed vegetables high in sodium |
| Proteins | Fish, Poultry, Beans | Processed meats, Red meat (in excess) |
| Grains | Brown rice, Quinoa | White bread, Refined pasta |
| Dairy | Plain yogurt, low-fat cheese | Full-fat dairy, processed cheeses |
| Fats | Avocado, Olive oil, Fatty fish | Processed foods, Red meat fat, Trans fats |
Dietary Considerations for Psoriasis Management
Following an anti-inflammatory diet is a crucial aspect of managing psoriasis. Beyond simply choosing the right foods, understanding how these foods are consumed and the overall impact of lifestyle choices is equally important. A balanced approach that considers portion control, hydration, gut health, stress management, and potential supplements can significantly contribute to reducing inflammation and improving overall well-being.
Portion Control and Psoriasis
Controlling portion sizes is a vital component of managing psoriasis through diet. Consuming large quantities of even healthy foods can lead to an imbalance in the body and potentially trigger or worsen psoriasis symptoms. Mindful eating, paying attention to hunger and fullness cues, and using smaller plates can help control portion sizes and contribute to better overall health.
Overeating, regardless of food type, can contribute to inflammation, so it’s essential to be mindful of your body’s signals.
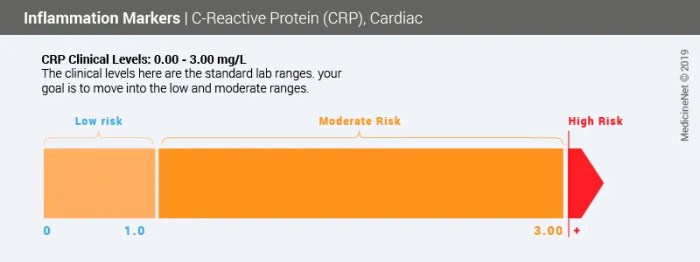
Hydration and Inflammation, Anti inflammatory diet for psoriasis
Adequate hydration plays a significant role in managing inflammation associated with psoriasis. Water is essential for numerous bodily functions, including removing waste products and regulating temperature. Dehydration can contribute to increased inflammation throughout the body, potentially worsening psoriasis symptoms. Aiming for 8 glasses of water a day is a general guideline, but individual needs may vary based on activity levels and climate.
Other hydrating beverages like herbal teas and unsweetened fruit juices can also contribute to daily fluid intake.
Gut Health and Psoriasis
The gut microbiome, the complex community of microorganisms residing in the digestive tract, has emerged as a key player in overall health, including psoriasis management. A healthy gut microbiome is essential for nutrient absorption, immune regulation, and overall well-being. Foods that support a balanced gut microbiome, such as fruits, vegetables, and fermented foods, can contribute to a healthier gut and potentially reduce inflammation associated with psoriasis.
Conversely, a diet high in processed foods, sugar, and unhealthy fats can disrupt the gut microbiome, potentially exacerbating psoriasis symptoms.
Stress Management and Diet
Stress can significantly impact the body’s inflammatory response, potentially worsening psoriasis symptoms. Stress triggers the release of hormones that increase inflammation. Managing stress through techniques like meditation, yoga, and deep breathing exercises can help regulate the body’s inflammatory response and contribute to better psoriasis management. A balanced diet, rich in nutrient-dense foods, can also support stress resilience.
Prioritizing sleep, engaging in regular physical activity, and maintaining social connections can also play a vital role in stress management.
Dietary Supplements for Psoriasis
While diet is crucial, certain supplements may offer additional support for psoriasis management. However, it’s essential to consult with a healthcare professional before starting any new supplement regimen. The following table provides a brief overview of potential supplements, but remember that individual responses can vary.
| Supplement | Potential Benefits | Important Considerations |
|---|---|---|
| Fish Oil | Rich in omega-3 fatty acids, which may have anti-inflammatory properties. | May interact with certain medications. |
| Vitamin D | May help regulate immune function. | Sunlight is a primary source; supplementation may be necessary for deficiencies. |
| Zinc | May help support immune function. | High doses may have adverse effects. |
| Probiotics | May support a healthy gut microbiome. | Choose high-quality probiotics and consider consulting a healthcare professional. |
| Curcumin | A natural compound with potential anti-inflammatory effects. | Effectiveness may vary between individuals. |
Sample Meal Plans and Recipes

Putting the principles of an anti-inflammatory diet into practice requires thoughtful meal planning. This section provides sample meal plans for a week, along with detailed recipes and simple preparation methods. We’ll also demonstrate how to adapt these plans to accommodate various dietary restrictions, making the transition to this lifestyle smoother and more sustainable.
I’ve been exploring anti-inflammatory diets for psoriasis lately, and it’s fascinating how much it can impact overall health. While researching, I stumbled upon the complexities of diagnosis and testing for HER2-positive breast cancer, diagnosis and testing for her2 positive breast cancer , and the importance of early detection. It made me realize that focusing on a healthy diet, including anti-inflammatory foods, is crucial for preventing and managing various health conditions, not just psoriasis.
Sample Weekly Meal Plans
The following meal plans are designed to provide a balanced intake of anti-inflammatory foods while keeping the meals delicious and manageable. These plans can be adjusted to fit individual needs and preferences.
- Monday: Focuses on lean protein, colorful vegetables, and healthy fats. Expect a balance of energy-boosting meals and satisfying snacks to support your day.
- Tuesday: Features a variety of whole grains and plant-based protein sources, emphasizing the importance of fiber for gut health and sustained energy levels.
- Wednesday: Highlights the use of spices and herbs to enhance flavor without relying on processed seasonings or high-sodium ingredients.
- Thursday: Explores recipes using fish as a primary protein source, rich in omega-3 fatty acids, known for their anti-inflammatory properties.
- Friday: Introduces a lighter approach with a greater emphasis on fresh salads and vegetable-based dishes, ideal for those who prefer less heavy meals.
- Saturday: Emphasizes flavorful and satisfying recipes, suitable for meal prepping to avoid last-minute decisions and keep the dietary focus consistent.
- Sunday: Provides a relaxing meal plan with a focus on nourishing and restorative foods, suitable for a more relaxed weekend schedule.
Recipes for Anti-Inflammatory Dishes
The following recipes are designed to be both delicious and supportive of an anti-inflammatory diet. They emphasize fresh ingredients, minimal processing, and a variety of flavors.
- Roasted Salmon with Asparagus and Quinoa: Salmon is rich in omega-3 fatty acids. Asparagus is packed with nutrients and antioxidants. Quinoa is a complete protein and a good source of fiber. Preparation involves simple roasting and is quick to make.
- Lentil Soup with Roasted Vegetables: Lentils are a fantastic source of plant-based protein and fiber. Roasted vegetables, like carrots, celery, and zucchini, add flavor and nutrients. The soup can be easily adapted to various spice preferences.
- Lemon Herb Chicken with Roasted Root Vegetables: Chicken provides lean protein, and root vegetables like sweet potatoes, carrots, and parsnips offer complex carbohydrates and essential vitamins. Herbs like rosemary and thyme add flavor without extra calories.
Simple Preparation Methods
Simplicity is key in an anti-inflammatory diet. These methods help you achieve delicious and healthy meals without excessive time spent in the kitchen.
- Roasting: A quick and healthy method for vegetables and proteins.
- Steaming: Preserves nutrients and minimizes the addition of fats.
- Stir-frying: A fast way to cook vegetables and protein with minimal oil.
Modifying Recipes for Dietary Restrictions
The following examples show how to adapt the recipes to various dietary needs.
An anti-inflammatory diet for psoriasis can really make a difference in managing symptoms. It’s all about focusing on foods that reduce inflammation in the body. Interestingly, some of the same principles can be applied to physical therapy exercises, like using parallel bars in physical therapy parallel bars in physical therapy to improve range of motion and strength.
Ultimately, both approaches aim to minimize inflammation and discomfort, making a significant impact on overall well-being, and the anti-inflammatory diet remains a crucial part of that.
- Gluten-Free: Substitute quinoa with brown rice or other gluten-free grains.
- Vegan: Substitute chicken with tofu or lentils. Ensure that all ingredients are vegan-friendly.
- Dairy-Free: Substitute dairy products with plant-based alternatives, like almond milk or coconut milk.
Recipe Table
| Recipe | Ingredients | Prep Time (minutes) |
|---|---|---|
| Roasted Salmon with Asparagus and Quinoa | Salmon fillets, asparagus spears, quinoa, olive oil, lemon juice, herbs | 20 |
| Lentil Soup with Roasted Vegetables | Lentils, carrots, celery, zucchini, onion, garlic, vegetable broth, herbs | 30 |
| Lemon Herb Chicken with Roasted Root Vegetables | Chicken breasts, sweet potatoes, carrots, parsnips, lemon, herbs, olive oil | 40 |
Potential Challenges and Solutions: Anti Inflammatory Diet For Psoriasis
Embarking on an anti-inflammatory diet for psoriasis can be a rewarding journey, but it’s crucial to anticipate potential obstacles and have strategies in place to navigate them. This section explores common challenges and provides practical solutions to ensure long-term adherence and success. Understanding these hurdles will help you stay motivated and achieve your health goals.
Common Challenges
Successfully transitioning to an anti-inflammatory diet requires a shift in eating habits and lifestyle choices. This shift can present various challenges, including the initial adjustment period, potential food restrictions, and maintaining long-term compliance. It’s important to recognize these hurdles as part of the process and have strategies in place to address them.
- Initial Adjustment Period: The initial transition to a new dietary pattern can be difficult. Familiar foods and recipes may need to be replaced, which can be a significant change for many individuals. This period can involve feelings of hunger, cravings, and even withdrawal symptoms. It’s important to remember that this is a temporary phase, and with patience and the right support system, you can overcome it.
- Food Restrictions: An anti-inflammatory diet often involves limiting processed foods, sugary drinks, and certain types of fats. This can be challenging for individuals who enjoy these foods or have ingrained dietary habits. Finding healthy alternatives and exploring new recipes can help ease this transition.
- Maintaining Long-Term Compliance: Maintaining dietary adherence over the long term can be a significant challenge. Life events, social gatherings, and daily stresses can disrupt adherence to the diet. Developing a sustainable plan and incorporating dietary changes into your daily routine is key to long-term success.
- Social Gatherings and Restaurant Meals: Eating out at restaurants or attending social gatherings can pose a significant challenge for those following a specific diet. Understanding how to navigate these situations and plan ahead is crucial for long-term adherence.
Solutions for Overcoming Challenges
Developing effective strategies to overcome these challenges is crucial for long-term adherence to an anti-inflammatory diet. These strategies should focus on gradual changes, support systems, and realistic expectations.
- Gradual Changes: Instead of making drastic changes overnight, adopt the new dietary approach gradually. Start by incorporating a few new foods or removing a few trigger foods each week. This gradual approach helps to avoid feeling overwhelmed and increases the likelihood of long-term success.
- Support Systems: Enlisting support from friends, family, or a registered dietitian can greatly enhance your ability to maintain a new diet. Sharing your journey and experiences with others can provide motivation and accountability.
- Realistic Expectations: Understanding that dietary changes take time and consistency is crucial. It’s essential to set realistic goals and avoid getting discouraged by occasional setbacks. Focus on progress, not perfection.
- Meal Planning and Preparation: Planning meals and preparing healthy snacks in advance can help you stay on track, especially when faced with busy schedules or unexpected events. This proactive approach reduces the likelihood of making unhealthy choices when time is limited.
- Understanding Dietary Needs: Consulting a registered dietitian can help tailor a personalized meal plan that addresses individual dietary needs, preferences, and any potential allergies or health conditions.
Importance of Professional Guidance
Seeking guidance from a healthcare professional is crucial for anyone considering an anti-inflammatory diet for psoriasis. A doctor or registered dietitian can help tailor the diet to your specific needs and health conditions.
- Personalized Recommendations: Healthcare professionals can provide personalized recommendations based on individual health conditions, allergies, and medical history. This is crucial to avoid potential complications and ensure the diet is safe and effective.
- Monitoring Progress: Healthcare professionals can monitor your progress and adjust the diet as needed. This proactive approach allows for adaptation based on individual response and ensures optimal outcomes.
Practical Strategies for Long-Term Adherence
Developing practical strategies for long-term adherence to an anti-inflammatory diet is essential for sustained improvement in psoriasis.
- Dietary Journaling: Keeping a detailed food diary can help identify patterns and triggers in your diet. This awareness can guide future choices and help you maintain compliance.
- Building Healthy Habits: Incorporating the dietary changes into your daily routine and lifestyle will make it a sustainable part of your life. Focus on making these changes part of your overall well-being.
- Finding Dietary Support Groups: Connecting with others who are following a similar diet can provide support, motivation, and practical advice. Online forums or local support groups can be beneficial.
| Common Challenges | Solutions |
|---|---|
| Initial adjustment period | Gradual changes, support systems, realistic expectations |
| Food restrictions | Finding healthy alternatives, exploring new recipes, support from a registered dietitian |
| Maintaining long-term compliance | Meal planning, preparation, dietary journaling, healthy habits |
| Social gatherings and restaurant meals | Planning ahead, communicating dietary needs, finding restaurant options with suitable choices |
Illustrative Visuals
Bringing the anti-inflammatory diet to life with visuals can significantly enhance understanding and engagement. Visual aids help solidify the connection between food choices, gut health, and psoriasis management. By presenting information in a digestible and compelling way, these visuals will empower individuals to make informed dietary decisions and potentially alleviate psoriasis symptoms.
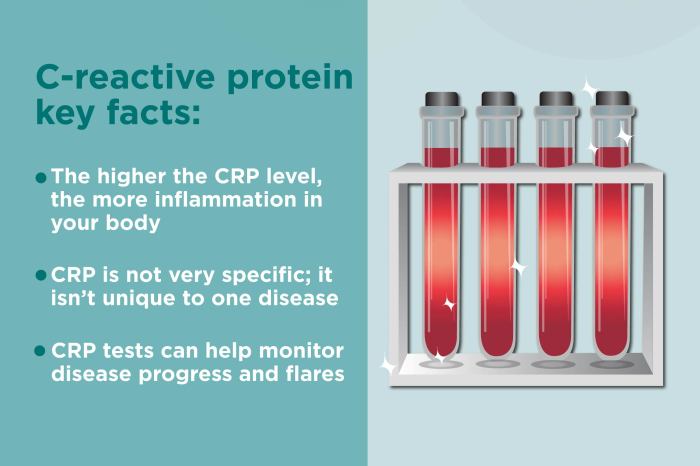
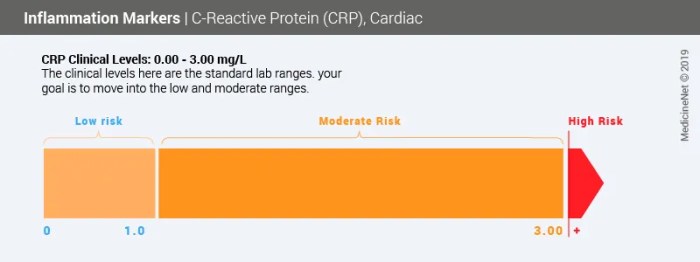
Visual Representation of Food Impact on Inflammation
A colourful infographic, perhaps a series of stacked bar graphs, could effectively demonstrate the impact of different food groups on inflammation levels. Each bar representing a food group (e.g., fruits, vegetables, processed foods) would have a gradient scale showing the level of anti-inflammatory or pro-inflammatory properties. For example, a vibrant green bar for leafy greens would be significantly taller and wider than a reddish-orange bar representing processed meats, visually highlighting the difference in their effects on inflammation.
This visual representation would make it clear which foods contribute to lower inflammation.
Visualizing Diet, Gut Health, and Psoriasis Connection
A diagram illustrating the interconnectedness of diet, gut health, and psoriasis is crucial. A simple flow chart or mind map would be effective. The flow chart could start with dietary choices influencing the gut microbiome. The diagram would then branch out to show how a healthy gut microbiome positively impacts the immune system, leading to reduced inflammation and potentially improved psoriasis symptoms.
A visual depiction of a healthy gut microbiome versus an imbalanced one could be included, with arrows highlighting the impact of diet on each.
Sample Meal Plan Visual
A visually appealing table or a series of images could display a sample meal plan. Each meal would be represented by a picture, or a series of pictures, of the specific foods. The meal plan would be clearly categorized by food groups (e.g., protein, carbohydrates, healthy fats, vegetables). This visual aids in understanding portion sizes and the balance of different food groups within a meal.
For example, a meal might show a portion of salmon, a serving of quinoa, and a large portion of steamed broccoli. This visual representation is vital for practical application and ensures meal planning is accessible.
Visualizing Portion Control
A visual aid, such as a series of progressively larger plates, could be used to demonstrate the importance of portion control. Each plate could represent a progressively larger portion of a particular food. This visualization would illustrate how even healthy foods can contribute to weight gain and potential inflammation if consumed in excessive amounts. For instance, a small plate of brown rice would be contrasted with a large plate of the same rice, making the point of portion size very clear.
The difference in the amount of food on each plate is emphasized, demonstrating the importance of mindful portioning.
Steps to Modify a Recipe for Dietary Restrictions
A step-by-step infographic or flowchart could illustrate how to modify a recipe for dietary restrictions common in psoriasis management. Each step would be accompanied by images or icons. For example, replacing ingredients, adjusting cooking methods, or substituting ingredients. The flowchart could clearly Artikel the steps needed to swap high-fat ingredients for healthier options. This will be highly useful to help users with recipes.
End of Discussion
In conclusion, an anti-inflammatory diet for psoriasis offers a promising path to symptom management and improved overall well-being. By understanding the link between food and inflammation, and incorporating practical strategies like portion control and mindful eating, you can significantly impact your psoriasis journey. Remember, this is a personalized approach. Consult with a healthcare professional before making significant dietary changes, and embrace the journey to a healthier, more comfortable life.