Information and history about vaccination and vaccines sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. We’ll journey through time, examining the groundbreaking scientific advancements, the societal impact, and the ongoing challenges and opportunities in the field of vaccination.
This exploration will cover everything from the early attempts to prevent disease to the cutting-edge research shaping the future of vaccination. We’ll uncover the scientific principles behind vaccines, delve into their safety and efficacy, and examine the role of vaccination programs in global health. Finally, we’ll confront the misinformation surrounding vaccines and discuss strategies to combat hesitancy and promote informed choices.
Historical Overview of Vaccination

Vaccination, a cornerstone of modern medicine, has dramatically altered the course of human history by preventing and controlling infectious diseases. From ancient practices to sophisticated modern techniques, the journey of vaccination reflects humanity’s evolving understanding of immunity and disease. This journey demonstrates a remarkable commitment to improving public health and well-being.The development of vaccination was not a sudden leap but rather a gradual process of observation, experimentation, and refinement.
Early observations of immunity, though lacking a scientific basis, laid the groundwork for future advancements. These early attempts, coupled with increasing scientific knowledge, eventually led to the creation of safe and effective vaccines that we rely on today.
Timeline of Significant Milestones
Early attempts at disease prevention predate the scientific understanding of germs and immunity. This section provides a chronological overview of key milestones in vaccination development. It highlights the evolution of understanding about immunity and the impact of vaccination on the eradication or control of infectious diseases.
| Year | Event | Key Figure(s) |
|---|---|---|
| 1000 AD | Early attempts at variolation in China and other parts of Asia | Various practitioners |
| 1717 | Lady Mary Wortley Montagu observes and introduces variolation to England | Lady Mary Wortley Montagu |
| 1796 | Edward Jenner develops the first vaccine against smallpox using cowpox | Edward Jenner |
| 1885 | Louis Pasteur develops a vaccine against rabies | Louis Pasteur |
| 1955 | Jonas Salk develops the inactivated polio vaccine (IPV) | Jonas Salk |
| 1963 | Albert Sabin develops the oral polio vaccine (OPV) | Albert Sabin |
| 1977 | Global eradication of smallpox | World Health Organization (WHO) and global efforts |
| 1988 | Global eradication of polio initiated | WHO and global efforts |
Progression of Understanding About Immunity and Disease Prevention
The development of vaccination was deeply intertwined with the evolution of scientific understanding of immunity. Early observations, often based on anecdotal evidence, led to the practice of variolation, which involved exposing individuals to material from smallpox patients to build immunity. This practice, while potentially dangerous, foreshadowed the concept of vaccination. Later, the work of Jenner, Pasteur, and others provided a more scientific basis for understanding how vaccines work.
The germ theory of disease, which established the role of microorganisms in causing disease, provided a crucial framework for developing effective vaccines.
Impact of Vaccination on Eradication or Control of Infectious Diseases
Vaccination has had a profound impact on public health. Smallpox, once a devastating global disease, was eradicated through vaccination campaigns. Polio, once a significant threat to children worldwide, is now largely controlled in many parts of the world due to widespread vaccination. Measles, mumps, and rubella, once common childhood illnesses, are now largely preventable through vaccination. These successes highlight the importance of vaccination programs in protecting populations and reducing morbidity and mortality from infectious diseases.
Scientific Principles Behind Vaccination
Vaccination is a cornerstone of modern medicine, dramatically reducing the global burden of infectious diseases. Understanding the scientific principles behind vaccination is crucial for appreciating its effectiveness and safety. This process harnesses the body’s natural immune response to build protection against future infections.The process of vaccination involves introducing a controlled dose of a pathogen or its components into the body.
This stimulates the immune system to develop a specific defense mechanism, creating immunological memory. This memory enables the body to quickly and effectively respond to a future infection with the same pathogen.
Immunological Mechanisms Involved in Vaccination
The immune system, a complex network of cells and proteins, plays a vital role in protecting the body from pathogens. Vaccination leverages the body’s adaptive immune response, specifically involving B cells and T cells. When a vaccine is introduced, it presents antigens – unique molecules found on the surface of pathogens. These antigens trigger the activation of B cells, which produce antibodies, specialized proteins that bind to and neutralize the antigens.
Simultaneously, T cells are activated, which help in eliminating infected cells.
Different Types of Vaccines and Their Mechanisms of Action
Various types of vaccines utilize different approaches to stimulate the immune response. Each type has its own strengths and weaknesses in terms of safety and effectiveness.
- Live Attenuated Vaccines: These vaccines use a weakened form of the live pathogen. The weakened pathogen can still replicate in the body, but it is not capable of causing disease. This triggers a strong and long-lasting immune response, similar to a natural infection. Examples include measles, mumps, and rubella (MMR) vaccines. The advantage lies in long-lasting immunity.
However, they may pose a risk to immunocompromised individuals.
- Inactivated Vaccines: These vaccines use a killed version of the pathogen. The pathogen is unable to replicate, eliminating the risk of infection. However, a stronger immune response may be required compared to live attenuated vaccines, sometimes requiring booster shots. Examples include influenza and polio vaccines. The safety profile is generally high.
- Subunit Vaccines: These vaccines use specific components of the pathogen, such as proteins or polysaccharides. These components are recognized as antigens by the immune system, triggering an immune response without the risk of infection. Examples include hepatitis B and some types of influenza vaccines. They are safer than live attenuated vaccines but may require multiple doses for optimal protection.
- Toxoid Vaccines: These vaccines target toxins produced by bacteria rather than the bacteria themselves. The toxins are inactivated, creating an immune response against them. Examples include tetanus and diphtheria vaccines. They are safe and effective in preventing the harmful effects of bacterial toxins.
Antigens, Antibodies, and the Immune Response in Vaccination
Antigens are the key to the immune response. They are foreign substances, such as proteins or polysaccharides, that trigger the production of antibodies. Antibodies are specialized proteins that bind to antigens, neutralizing or eliminating them. The immune response, involving both cellular and humoral components, is crucial for mounting an effective defense against pathogens.
Comparison of Vaccine Types
| Vaccine Type | Mechanism of Action | Effectiveness | Safety Profile |
|---|---|---|---|
| Live Attenuated | Weakened live pathogen | Generally high and long-lasting | Generally safe, but risks to immunocompromised |
| Inactivated | Killed pathogen | Generally good, may require boosters | Very safe |
| Subunit | Specific components of the pathogen | Good, may require multiple doses | Very safe |
| Toxoid | Inactivated bacterial toxins | High and long-lasting | Very safe |
Vaccination Safety and Efficacy
Vaccination is a cornerstone of public health, dramatically reducing the incidence of infectious diseases. However, concerns about safety and efficacy persist. This section delves into the robust evidence supporting the safety profile of vaccines and the rigorous processes ensuring their effectiveness.The overwhelming scientific consensus unequivocally supports the safety and efficacy of vaccines. Decades of research and real-world data have demonstrated their profound impact in preventing debilitating and often fatal diseases.
Evidence Supporting Vaccine Safety and Efficacy
A vast body of research, spanning multiple independent studies and clinical trials, validates the safety and efficacy of vaccines. These studies consistently demonstrate that vaccines are remarkably safe, with serious adverse events being exceedingly rare. The benefits of vaccination, in terms of disease prevention and overall public health, far outweigh the very low risk of side effects.
Common Side Effects and Their Severity
While most individuals experience only minor side effects, such as soreness at the injection site, mild fever, or fatigue, these are generally short-lived and resolve spontaneously. Serious adverse events are extremely rare. The severity of these side effects is typically mild and transient.
Delving into the history of vaccines is fascinating, showing how far we’ve come in protecting ourselves from illness. While I’m fascinated by how vaccines work, I also wonder about the effectiveness of air purifiers in our homes. Knowing how important clean air is for our health, I recently looked into do air purifiers work and the science behind them.
Ultimately, understanding the history of vaccines, and the science behind their effectiveness, is crucial for making informed decisions about our health.
Rigorous Testing and Evaluation Processes for Vaccines
Vaccines undergo rigorous testing and evaluation processes before licensure. These processes involve multiple phases of clinical trials, with increasing numbers of participants in each phase. These trials assess both safety and efficacy, monitoring for any potential adverse effects. The data collected during these trials is rigorously analyzed and evaluated by regulatory bodies to ensure the vaccine meets established safety and efficacy standards.
The specific phases and criteria are publicly available.
Vaccine Safety Monitoring and Tracking Post-Licensure
Post-licensure, vaccine safety is continuously monitored and tracked through robust surveillance systems. This includes monitoring for rare side effects that may not have been detected in earlier trials. Reporting mechanisms are in place for healthcare professionals to report any potential adverse events. Data from these systems allows for the ongoing evaluation and refinement of vaccine safety profiles.
Risks of Vaccination vs. Risks of Contracting Targeted Diseases
| Vaccination Risks | Risks of Contracting Targeted Diseases | |
|---|---|---|
| Serious Adverse Events | Extremely rare | High risk of severe illness, disability, or death |
| Minor Side Effects | Common but typically mild and temporary | Potential for long-term health complications |
| Disease Prevention | Vaccination prevents the disease | Disease poses a significant health risk |
| Long-Term Impacts | Rare and typically mild | Potentially life-altering or fatal consequences |
“The benefits of vaccination far outweigh the risks.”
The table clearly illustrates the significantly higher risks associated with contracting the diseases vaccines target, compared to the very low risks of adverse events from vaccination. The evidence overwhelmingly supports the safety and efficacy of vaccines.
Diving into the fascinating history of vaccines and vaccination is truly eye-opening. From the early days of inoculation to the modern marvels of mRNA technology, it’s a story of incredible scientific progress. Want to know how many calories you burn powering through a mile? Check out this resource to calculate your individual burn rate how many calories do you burn running a mile.
Ultimately, understanding these advancements in public health is crucial for making informed decisions about your well-being and the health of those around you.
Vaccination Programs and Policies: Information And History About Vaccination And Vaccines
Vaccination programs are crucial for maintaining public health and preventing the spread of infectious diseases. Effective programs rely on well-defined policies, strong public health infrastructure, and community engagement. These policies dictate which vaccines are administered, when, and to whom, ensuring widespread protection and minimizing the risk of outbreaks. The success of these programs hinges on their ability to overcome challenges and ensure equitable access to vaccination.Public health organizations play a pivotal role in shaping and implementing vaccination programs.
They develop and recommend vaccination schedules, provide education and awareness campaigns, and monitor the impact of vaccination policies on public health outcomes. These organizations act as central hubs, coordinating efforts to promote vaccination as a crucial component of public health strategies.
Role of Public Health Organizations
Public health organizations are instrumental in advocating for and implementing effective vaccination programs. They provide essential resources, technical support, and guidelines to governments and healthcare providers. Their role extends to conducting surveillance, monitoring disease trends, and responding to outbreaks, thus influencing policies to address evolving health needs. They also provide critical information to the public, fostering understanding and promoting informed decision-making regarding vaccination.
Implementation of Vaccination Schedules
Vaccination schedules vary across regions, tailored to the specific disease burden and epidemiological context. These schedules often prioritize vulnerable populations, such as infants and children, and incorporate recommended intervals between doses. Factors such as logistical considerations, resource availability, and vaccine cold chain infrastructure impact the implementation process. Countries with robust healthcare systems and well-established infrastructure typically experience smoother implementation and higher vaccination coverage.
However, challenges remain in ensuring equitable access in regions with limited resources.
Impact of Vaccination Policies on Public Health Outcomes
Vaccination policies significantly impact public health outcomes. Policies that mandate vaccination, combined with strong public health campaigns, can dramatically reduce the incidence of vaccine-preventable diseases. Increased vaccination coverage correlates with a decline in morbidity and mortality associated with these diseases. This is clearly seen in the historical decrease in cases of polio and measles following the implementation of vaccination programs.
The impact is not uniform; policies must be adapted to specific contexts and challenges.
Diving into the fascinating world of vaccination history is truly eye-opening. From ancient practices to modern advancements, the journey of immunization is remarkable. Knowing how vaccines work is crucial, but so is understanding what to do if you experience a sharps injury, like a needle prick. For detailed guidance on proper procedures, check out this helpful resource: what to do if you experience a sharps injury.
Ultimately, understanding the science behind vaccination and vaccines is vital for maintaining health and well-being.
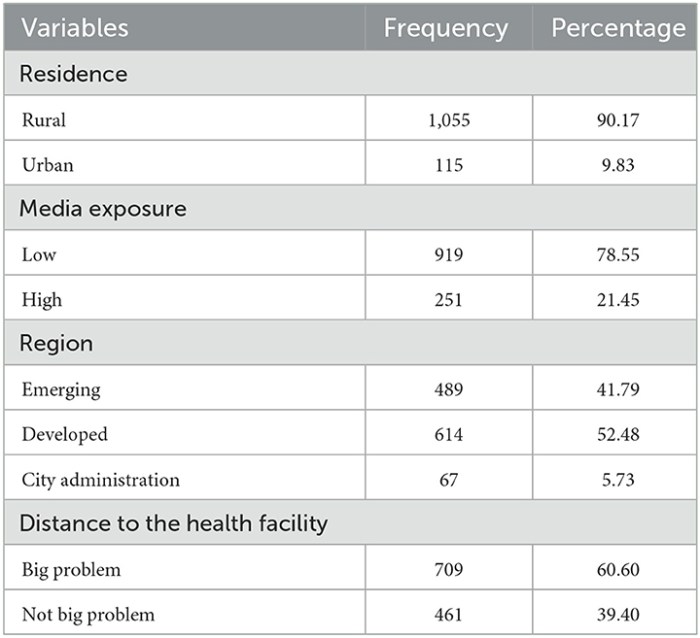
Challenges and Barriers to Vaccination Access and Uptake
Several challenges hinder vaccination access and uptake. These include financial barriers, logistical difficulties in accessing vaccination sites, misinformation, and hesitancy among certain populations. Geographic barriers, particularly in remote areas, can also pose significant obstacles. Addressing these challenges requires a multifaceted approach, encompassing financial assistance programs, improved accessibility, and targeted communication strategies to address misinformation and build trust.
Furthermore, cultural and religious factors can play a role in vaccine hesitancy and require specific strategies for engagement and education.
Summary Table of Vaccination Programs
| Country | Target Populations | Coverage Rates (approximate) |
|---|---|---|
| United States | Children, adolescents, adults | Generally high, with some variability by disease and region |
| United Kingdom | Children, adolescents, adults | Generally high, with ongoing efforts to improve coverage |
| India | Children, pregnant women, high-risk groups | High coverage in some regions, but challenges remain in others |
| Nigeria | Children, adolescents, pregnant women | Lower than global averages, facing specific challenges |
| Brazil | Children, adolescents, adults | High overall, but with regional variations |
Note: Coverage rates are approximate and may vary based on the specific vaccine and year. Data collection methodologies and reporting standards can differ across countries, potentially affecting the accuracy of comparisons.
Misinformation and Public Perception
The widespread availability of information, while a powerful tool, can also be a breeding ground for misinformation. This is particularly true for complex topics like vaccination, where emotions and personal beliefs often outweigh factual data. This section delves into the sources of vaccine misinformation, common misconceptions, and strategies to combat hesitancy. Understanding these issues is crucial for fostering informed public health decisions.Vaccine hesitancy is a complex issue, fueled by a multitude of factors including distrust in institutions, fear of side effects, and the spread of misinformation.
This distrust, often rooted in personal experiences or misinterpreted scientific data, can have severe public health consequences, hindering the effectiveness of vaccination programs and increasing the risk of preventable diseases.
Sources of Vaccine Misinformation
Misinformation surrounding vaccines originates from various sources. These include social media platforms, anti-vaccine websites, and even individuals with personal agendas. The rapid spread of information on social media, often without proper fact-checking, can amplify unsubstantiated claims. The lack of stringent fact-checking processes on some platforms allows false information to circulate widely, leading to widespread public confusion.
Common Misconceptions About Vaccines
Several misconceptions about vaccines persist despite overwhelming scientific evidence to the contrary. These misconceptions often center on safety concerns, effectiveness, and the perceived necessity of vaccination. Addressing these misconceptions requires clear and accessible explanations backed by scientific evidence.
- Vaccines cause autism: Extensive research has consistently refuted the link between vaccines and autism. The original study that sparked this misconception was later retracted and deemed fraudulent. Numerous well-designed studies have demonstrated no causal relationship between vaccines and autism.
- Vaccines contain harmful toxins: Modern vaccines do not contain harmful toxins like mercury or formaldehyde in significant quantities. The small amounts present are either inactive or used as preservatives, and their use is carefully regulated and monitored to ensure safety.
- Vaccines overwhelm the immune system: Vaccines stimulate, rather than overwhelm, the immune system. The antigens in vaccines are carefully chosen and inactivated, or weakened, to elicit an immune response without causing the disease itself. This controlled stimulation helps the body develop immunity.
Strategies to Combat Vaccine Hesitancy
Combating vaccine hesitancy requires a multifaceted approach. This involves providing clear, accessible, and evidence-based information to the public. Open communication, transparency, and addressing concerns directly are crucial.
- Education and Awareness Campaigns: Public health campaigns that highlight the safety and efficacy of vaccines are essential. These campaigns should target diverse communities and use multiple communication channels, including social media, community events, and educational materials. Tailoring messages to specific demographics can increase their effectiveness.
- Building Trust with Healthcare Providers: Strong relationships between healthcare providers and patients are paramount. Open communication about vaccines, addressing concerns, and providing accurate information can build trust and encourage vaccination.
- Promoting Media Literacy: Educating the public on how to critically evaluate information, especially online, is crucial. Helping people identify reliable sources of information can empower them to make informed decisions about their health.
Importance of Accurate and Reliable Information
Accurate and reliable information about vaccines is vital for public health. The spread of misinformation can undermine public confidence in vaccines, leading to decreased vaccination rates and increased risks of preventable diseases. Access to accurate information empowers individuals to make informed decisions about their health and the health of their communities.
Common Myths and Scientific Facts
| Myth | Scientific Fact |
|---|---|
| Vaccines contain harmful chemicals. | Modern vaccines contain carefully regulated components and do not contain harmful chemicals in significant quantities. These components are essential for vaccine function and safety. |
| Vaccines weaken the immune system. | Vaccines stimulate the immune system, prompting it to develop immunity against specific diseases. This controlled stimulation, rather than weakening it, helps build immunity. |
| Vaccines cause more side effects than the diseases they prevent. | The side effects of vaccines are generally mild and temporary, such as soreness or fever. The diseases vaccines prevent often have severe and potentially life-threatening complications. |
Future of Vaccination
The journey of vaccination is far from over. Ongoing research and development promise to enhance vaccine efficacy, safety, and accessibility, while emerging challenges require innovative solutions. This exploration delves into the exciting and crucial future of vaccination, examining new frontiers in vaccine technology and their potential impact on global health.
Ongoing Research and Development of New Vaccines
The quest for improved vaccines extends across various disease targets. Scientists are actively pursuing novel approaches, including the development of mRNA vaccines for previously challenging pathogens, exploring the use of different delivery systems like nanoparticles for enhanced efficacy and reduced side effects, and creating more stable and potent subunit vaccines. These advancements aim to tackle a wider range of diseases, from seasonal influenza to emerging viral threats, with the potential to revolutionize vaccine strategies.
Emerging Challenges and Opportunities in Vaccine Technology
Vaccine development faces several hurdles. One key challenge is the need for faster and more adaptable vaccine production to respond rapidly to emerging infectious diseases. This necessitates developing more efficient and cost-effective manufacturing processes. Another important consideration is the equitable distribution of vaccines globally, addressing the challenges of accessibility and affordability in resource-limited settings. Opportunities lie in leveraging innovative technologies for vaccine delivery, like mucosal vaccines for improved immune responses, or targeted adjuvants to boost vaccine efficacy.
Potential Future Trends in Vaccination Strategies
Several promising trends are shaping the future of vaccination strategies. The integration of genomics into vaccine development allows for the identification of conserved epitopes for broader protection against pathogen variants, leading to more effective and long-lasting immunity. Personalized vaccine strategies based on individual genetic profiles and prior immune responses are also gaining traction, potentially maximizing vaccine efficacy and minimizing adverse reactions.
Furthermore, the development of combination vaccines for multiple diseases is likely to continue, simplifying vaccination schedules and increasing compliance.
Role of Vaccines in Addressing Emerging Infectious Diseases
Emerging infectious diseases represent a significant threat to global health. Vaccines play a crucial role in preventing their spread and mitigating their impact. For example, the development of vaccines for emerging coronaviruses, such as SARS-CoV-2, highlights the need for rapid vaccine development and deployment to combat pandemic threats effectively. The need for adaptable vaccine platforms that can be modified quickly to address emerging viral variants is critical to effectively combating new pathogens.
Use of Innovative Technologies in Vaccine Development and Delivery
Innovative technologies are revolutionizing vaccine development and delivery. mRNA vaccines, for example, are rapidly transforming the field by allowing for rapid production and adaptation to new pathogens. This technology enables tailored responses to evolving viral threats, dramatically accelerating the process of vaccine creation. Furthermore, the use of nanotechnology for vaccine delivery systems promises improved targeting and reduced side effects.
These advancements offer a powerful toolkit to enhance vaccine effectiveness and accessibility.
Visual Representation of Vaccination Data
Visual representations of vaccination data are crucial for understanding the impact of vaccination programs, identifying areas needing improvement, and effectively communicating the importance of vaccination to the public. Clear and compelling visuals can effectively convey complex information, highlighting the success stories and challenges faced in global vaccination efforts. These tools allow for easy comparison of vaccination coverage across regions and over time, revealing patterns and trends that might otherwise be missed.Visualizations can also help policymakers, public health officials, and researchers track the effectiveness of vaccination campaigns, enabling them to adapt strategies and prioritize resources accordingly.
They empower individuals by showcasing the real-world impact of vaccination on disease prevalence, and helping dispel misinformation and promote informed decision-making.
Global Impact of Vaccination on Disease Prevalence, Information and history about vaccination and vaccines
A line graph displaying global measles cases over time, alongside a parallel line graph showing the number of measles vaccinations administered, visually demonstrates the correlation between vaccination rates and disease prevalence. The graph would clearly illustrate how increasing vaccination rates have directly led to a significant decrease in measles cases globally. Variations in vaccination rates across different regions can also be highlighted with different colored lines, providing a clear picture of regional disparities and the need for targeted interventions.
Success of Specific Vaccination Campaigns
A bar chart illustrating the success of specific vaccination campaigns, such as the polio eradication campaign, would effectively demonstrate the impact of coordinated efforts. The chart could compare the number of cases before and after the campaign, showing the significant reduction in disease prevalence. Data could be broken down by region to highlight regional variations in campaign success and identify areas requiring further support.
This would emphasize the effectiveness of vaccination campaigns in controlling and even eliminating infectious diseases.
Vaccine Development Process
A flowchart illustrating the vaccine development process from research to deployment would provide a clear overview of the steps involved. The flowchart would show the various stages, from initial research and testing in laboratories to clinical trials, regulatory approvals, and finally, the distribution and administration of the vaccine. This would help demystify the process and increase public trust in vaccines.
Benefits of Vaccination
An infographic summarizing the benefits of vaccination would be a powerful tool for educating the public. The infographic could visually represent the key benefits, such as preventing serious illnesses, protecting future generations, and reducing the burden on healthcare systems. It could include icons or illustrations representing each benefit and corresponding text to explain each point in detail. Using a clear, concise, and visually appealing design would maximize its effectiveness.
Interactive Map of Vaccination Coverage
An interactive map highlighting vaccination coverage rates across different regions would provide a dynamic visualization of vaccination rates globally. Users could zoom in on specific countries or regions to see the detailed vaccination coverage rates, and perhaps even the data broken down by specific age groups or populations. This would facilitate the identification of regions with low vaccination coverage and allow for targeted interventions to address specific needs and improve vaccination rates.
Interactive features could allow users to compare vaccination rates across different regions and track changes over time.
Closure

In conclusion, the history and information about vaccination and vaccines reveal a remarkable story of scientific progress and its profound impact on public health. From humble beginnings to modern innovations, vaccines have demonstrably saved countless lives and continue to be a cornerstone of disease prevention. Understanding the science, the history, and the ongoing challenges is crucial for making informed decisions about our health and the health of future generations.