Can allergies cause a fever? This question delves into the intricate relationship between allergic reactions and elevated body temperature. Allergies, encompassing a spectrum of immune responses to foreign substances, often manifest as uncomfortable symptoms like sneezing, itching, and rashes. However, the connection to fever is less straightforward. While a fever is frequently associated with infections,…
Tag: immune system
Why Do I Keep Getting Sick? The Truth
Why do I keep getting sick? This persistent illness can be frustrating, and understanding the underlying causes is key to regaining your well-being. This post delves into potential reasons, from lifestyle choices to underlying health conditions, environmental factors, and nutritional deficiencies. We’ll explore how each element impacts your immune system, offering insights and solutions for…
Does Vitamin C Help With Colds? A Deep Dive
Does vitamin C help with colds? This question has plagued countless individuals throughout history, and the answer, as you might expect, isn’t a simple yes or no. We’ll delve into the science behind vitamin C’s role in the immune system, explore common cold symptoms, examine studies on vitamin C and cold duration, and discuss safe…
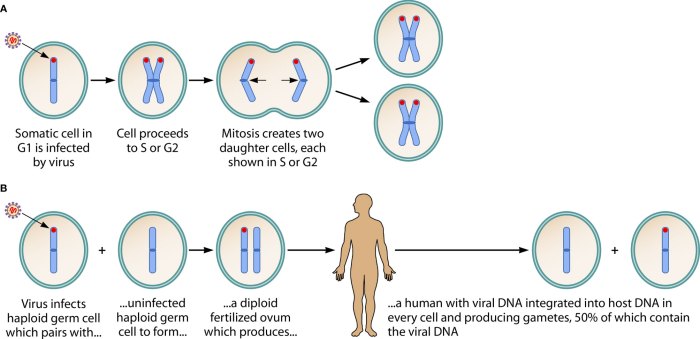
HHV-6 and Its Role in Disease A Deep Dive
Hhv 6 and its role in disease – HHV-6 and its role in disease is a fascinating area of research, exploring the intricate ways this common virus can impact human health. From its subtle presence in childhood infections to potential links with adult conditions, understanding HHV-6 is crucial for better diagnosis and treatment. This exploration…