Kicking off with IBS vs colon cancer, this exploration delves into the often-confusing similarities and differences between these two conditions. Irritable bowel syndrome (IBS) and colon cancer, while both affecting the digestive system, have distinct characteristics. Understanding these differences is vital for accurate diagnosis and effective management. This comprehensive guide will explore the symptoms, diagnostic challenges, treatment approaches, and long-term impacts of each, equipping you with a better understanding of the complexities involved.
From the initial symptoms to the diagnostic process, the comparison highlights the nuances that can easily lead to misdiagnosis. We’ll break down the key distinctions between IBS and colon cancer, examining the specific symptoms, typical progression, and response to treatment. This in-depth analysis will help you navigate the complexities of these conditions and make informed decisions about your health.
Introduction to IBS and Colon Cancer
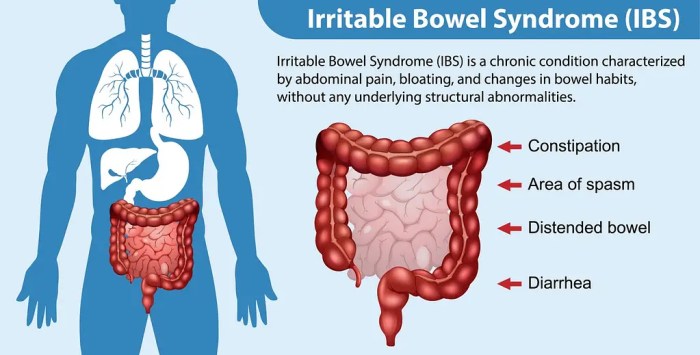
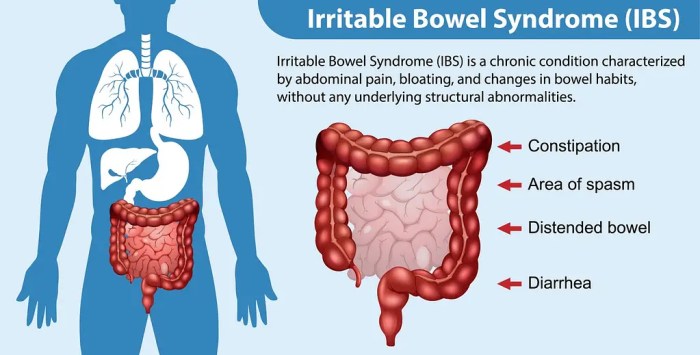
Irritable bowel syndrome (IBS) and colon cancer are two distinct conditions affecting the digestive system, yet they share some overlapping symptoms that can lead to confusion. Understanding the differences in their causes, symptoms, and diagnostic processes is crucial for proper healthcare. This section will Artikel the key characteristics of both conditions to help clarify their unique features.IBS is a common functional disorder of the digestive tract, while colon cancer is a serious malignancy.
While both can cause significant discomfort and disrupt daily life, the underlying mechanisms and potential outcomes are vastly different. Early detection and appropriate treatment are essential for both conditions, and recognizing the distinguishing features is paramount for effective medical intervention.
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a chronic functional disorder of the digestive system characterized by recurring abdominal pain, changes in bowel habits, and other associated symptoms. It’s important to note that IBS does not cause damage to the bowel tissue, unlike some other conditions.Common symptoms of IBS include abdominal pain, bloating, gas, diarrhea, and/or constipation. The pain is often described as cramping and can be influenced by factors like stress, diet, and hormonal changes.
Symptoms may fluctuate in severity and frequency, and periods of remission are possible.
Types of IBS
IBS is categorized into different subtypes based on predominant bowel habits. The most common types are IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), and IBS with mixed bowel habits (IBS-M). The classification helps in tailoring treatment strategies.
Diagnostic Process for IBS
Diagnosis of IBS typically involves a comprehensive evaluation by a healthcare professional. This includes a thorough medical history, physical examination, and often, a review of symptoms and dietary patterns. Specific tests like stool analysis and colonoscopies may be used to rule out other conditions. It’s crucial to note that the diagnostic process for IBS often focuses on excluding other conditions with similar symptoms.
Mechanisms of Colon Cancer Development
Colon cancer arises from the uncontrolled growth of cells lining the colon. This process typically involves several stages, including the development of polyps, which are abnormal growths on the colon lining. Over time, some polyps can develop into cancerous tumors. Genetic mutations and environmental factors can play a role in the development of these polyps and the progression to cancer.
“Early detection of polyps through screening is crucial in preventing the development of colon cancer.”
Figuring out if your gut issues are IBS or something more serious like colon cancer can be tricky. Sometimes, symptoms can overlap, but a key difference lies in the potential for complications. Distal intestinal obstruction syndrome, for instance, can arise from certain conditions, highlighting the importance of seeking medical advice. Ultimately, accurate diagnosis requires a thorough examination, and comparing symptoms of IBS against the risks of colon cancer remains crucial in getting the right care.
Risk Factors for Colon Cancer
Several factors can increase the risk of developing colon cancer. These include age (risk increases with age), family history of colon cancer, a personal history of inflammatory bowel disease (IBD), certain dietary habits, and lifestyle factors like smoking and lack of physical activity.
Comparison of IBS and Colon Cancer Symptoms
| Symptom | IBS Description | Colon Cancer Description | Severity |
|---|---|---|---|
| Abdominal Pain | Cramping, intermittent pain, often relieved by bowel movements | Persistent pain, possibly radiating, may worsen over time | Mild to Moderate |
| Changes in Bowel Habits | Diarrhea, constipation, or alternating patterns | Changes in bowel habits, including blood in stool, can be a sign of advanced stages | Mild to Moderate |
| Bloating and Gas | Common, often associated with pain | Bloating and gas can occur but are not primary symptoms | Mild to Moderate |
| Fatigue | May occur but is not a primary symptom | Can be a symptom of advanced stages or related to anemia | Mild to Moderate |
Similarities and Differences

Understanding the nuances between Irritable Bowel Syndrome (IBS) and colon cancer is crucial for accurate diagnosis and effective treatment. Both conditions can manifest with similar gastrointestinal symptoms, leading to potential misdiagnosis. However, critical differences exist in their underlying causes, symptom progression, and response to treatment. This section will delve into the overlapping and distinct characteristics of these conditions.Differentiating IBS from colon cancer requires careful consideration of symptom patterns, duration, and accompanying factors.
A thorough medical evaluation, including physical examinations and diagnostic tests, is essential to reach a precise diagnosis.
Symptom Overlap and Potential Misdiagnosis
The shared symptoms between IBS and colon cancer can often lead to confusion and misdiagnosis. Both conditions can present with abdominal pain, changes in bowel habits (constipation or diarrhea), bloating, and nausea. This overlap in symptoms underscores the importance of a comprehensive evaluation by a healthcare professional. For example, a patient experiencing intermittent abdominal pain and altered bowel movements might initially be suspected of having IBS, but a deeper investigation might reveal signs of colon cancer.
This emphasizes the critical need for further testing to rule out more serious conditions.
Distinguishing Symptoms
While some symptoms overlap, key differences exist in the nature and progression of symptoms. In IBS, symptoms are typically intermittent and fluctuate in intensity. They often respond to dietary changes and stress management techniques. In contrast, colon cancer symptoms frequently progress over time, and symptoms may become more persistent and severe. An individual experiencing persistent and worsening abdominal pain, blood in the stool, unexplained weight loss, or a significant change in bowel habits warrants immediate medical attention to rule out colon cancer.
Symptom Progression
The progression of symptoms differs significantly between IBS and colon cancer. IBS symptoms often fluctuate, coming and going with periods of remission. Colon cancer, on the other hand, usually develops gradually, with symptoms often worsening over time. Early detection is critical, as the longer colon cancer goes undetected, the more advanced it becomes, and the more severe the symptoms and potential complications become.
Response to Treatment
The response to treatment also varies. IBS is typically managed with lifestyle modifications, dietary changes, stress reduction techniques, and medications to alleviate symptoms. Colon cancer, however, necessitates a multifaceted approach, including surgery, chemotherapy, radiation therapy, and targeted therapies, depending on the stage of the disease.
Key Differences Table
| Feature | IBS | Colon Cancer | Implications |
|---|---|---|---|
| Symptoms | Intermittent abdominal pain, altered bowel habits (constipation or diarrhea), bloating, gas | Persistent abdominal pain, blood in the stool, unexplained weight loss, change in bowel habits, fatigue, anemia | Symptoms can overlap, necessitating careful evaluation. |
| Symptom Progression | Symptoms fluctuate, periods of remission | Symptoms gradually worsen over time | Early detection is crucial for colon cancer. |
| Treatment | Lifestyle modifications, dietary changes, stress management, medications | Surgery, chemotherapy, radiation therapy, targeted therapies | Treatment approaches differ dramatically. |
| Underlying Cause | Complex interplay of factors including genetics, diet, and stress | Uncontrolled cell growth in the colon | Different root causes lead to different treatment strategies. |
Diagnostic Challenges
Distinguishing between Irritable Bowel Syndrome (IBS) and colon cancer can be notoriously difficult. Both conditions can present with similar symptoms, making accurate diagnosis a crucial step in appropriate treatment. This complexity often necessitates a multi-faceted approach, combining detailed medical history, physical examinations, and various diagnostic tests.Early and precise diagnosis is paramount in cases of colon cancer, as early detection significantly improves treatment outcomes.
Figuring out if your tummy troubles are IBS or something more serious like colon cancer can be tricky. While diet plays a role in both, understanding if foods like strawberries are good for your gut health can be helpful. A recent study I’ve been looking into suggests that certain fruits, like are strawberries good for you and their impact on gut bacteria, might be key to preventing inflammation.
Ultimately, if you’re concerned, consulting a doctor is the best way to differentiate between these conditions.
Conversely, misdiagnosis of colon cancer as IBS can lead to delayed intervention and potentially more severe health consequences. Therefore, healthcare providers must carefully consider all available information to arrive at an accurate diagnosis.
Difficulties in Distinguishing Symptoms
The overlapping symptoms between IBS and colon cancer pose significant challenges for clinicians. Abdominal pain, bloating, changes in bowel habits, and blood in the stool can be present in both conditions. This similarity often necessitates further investigation to determine the underlying cause. Careful symptom analysis and detailed medical history are essential in differentiating between the two.
Figuring out if your tummy troubles are IBS or something more serious like colon cancer can be tricky. Understanding the different symptoms is key, but sometimes it’s the subtle things, like what foods make you feel full, that can help. Knowing which foods fill you up longer and are easy on your digestive system could help pinpoint potential issues.
For example, discovering foods that promote satiety and comfort can be a crucial step in managing IBS symptoms and preventing any potential discomfort or problems. Learning more about these foods can be a good starting point to better understand your body and its needs, helping you make informed choices about your diet and potentially differentiating IBS from colon cancer.
You can find some great ideas on foods that make you feel full that might be helpful.
Limitations of Current Diagnostic Methods
Currently available diagnostic methods for differentiating IBS from colon cancer are not foolproof. Some tests may yield inconclusive results or show non-specific findings. For instance, some blood tests may indicate inflammation, but inflammation can be associated with various conditions, including both IBS and colon cancer. This ambiguity underscores the importance of a comprehensive approach to diagnosis.
Importance of Thorough Medical History
A comprehensive medical history plays a critical role in the diagnostic process. A detailed account of symptoms, including their onset, duration, frequency, and any associated factors (such as stress or diet), can provide valuable clues. A detailed family history, including instances of colon cancer or other relevant gastrointestinal conditions, is equally important. The clinician should meticulously document the patient’s history to better understand the nuances of their symptoms and potentially identify risk factors.
Role of Imaging Techniques
Imaging techniques, such as CT scans, colonoscopies, and MRI scans, play a significant role in the diagnostic process. A CT scan can reveal abnormalities in the colon or abdomen, while colonoscopies allow direct visualization of the colon’s lining, potentially identifying cancerous polyps or tumors. These imaging modalities can provide crucial anatomical information, aiding in the differentiation between IBS and colon cancer.
However, imaging alone may not always be conclusive and must be interpreted alongside other diagnostic data.
Tests to Rule Out Colon Cancer in IBS Patients
Several tests are commonly employed to rule out colon cancer in patients presenting with IBS symptoms. These tests help identify potential indicators of cancerous growths or other concerning abnormalities. A key goal is to avoid unnecessary anxiety while still ensuring thorough evaluation.
- Colonoscopy: A colonoscopy is a procedure that allows direct visualization of the colon’s lining. This is a vital tool for identifying polyps, tumors, or other abnormalities that might be indicative of colon cancer.
- Barium Enema: This X-ray procedure involves injecting barium into the colon to visualize its structure and identify any structural abnormalities. While less common than colonoscopy, it can still be a valuable tool in the diagnostic process.
- Stool Tests: Various stool tests, including occult blood tests, can detect the presence of blood in the stool, a potential sign of colon cancer. These tests are frequently used as a screening tool.
- Blood Tests: Certain blood tests can help assess inflammation or other markers that might be indicative of a more serious condition like colon cancer.
- CT Scan: A CT scan can provide cross-sectional images of the abdomen and pelvis, allowing visualization of the colon and surrounding tissues. This imaging technique can help identify potential abnormalities or masses.
Diagnostic Tests Table
| Test | Purpose | IBS Relevance | Colon Cancer Relevance |
|---|---|---|---|
| Colonoscopy | Visualize the colon lining | Can detect IBS-related inflammation or abnormalities | Identifies polyps, tumors, and cancerous lesions |
| Barium Enema | Visualize the colon structure | Can identify IBS-related structural abnormalities | Can reveal tumors or masses |
| Stool Tests (Occult Blood) | Detect blood in the stool | May be positive due to inflammation | Crucial for detecting hidden bleeding, a potential sign of cancer |
| Blood Tests (e.g., CRP) | Assess inflammation | May indicate inflammation associated with IBS | May indicate inflammation associated with cancer |
| CT Scan | Provide cross-sectional images of the abdomen | Can show abnormalities in the colon or abdomen | Can detect tumors, masses, and metastasis |
Treatment Approaches
Understanding the treatment approaches for both IBS and colon cancer is crucial for effective management and improved quality of life. Different strategies are employed depending on the severity and individual characteristics of the disease. Proper diagnosis and tailored treatment plans are essential to achieving the best possible outcomes.
Standard Treatment Approaches for IBS
IBS, a functional disorder, often responds well to lifestyle modifications and symptom-management strategies. Medications are typically reserved for persistent or severe symptoms. Dietary changes, stress reduction techniques, and regular exercise are frequently recommended.
- Dietary Modifications: A key aspect of IBS management involves identifying trigger foods and implementing dietary strategies. Elimination diets, where certain foods are temporarily removed from the diet, can help pinpoint culprits. Low-FODMAP diets, limiting fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, are often beneficial for reducing symptom severity. Regular meals and avoiding large meals can also be helpful.
- Stress Management Techniques: Stress and anxiety can significantly exacerbate IBS symptoms. Techniques like yoga, meditation, and mindfulness exercises can be valuable tools for managing stress and improving overall well-being. Sufficient sleep and regular relaxation practices are also crucial.
- Medications: Various medications can be prescribed to address specific IBS symptoms. Antispasmodics can help reduce abdominal cramps and pain. Laxatives may be used to manage constipation. Antidiarrheals can be effective in controlling diarrhea. Antidepressants can also be beneficial in some cases, especially for managing pain and anxiety associated with IBS.
Treatment Plans for Colon Cancer
Colon cancer treatment is highly individualized and depends on the stage and extent of the disease. A multidisciplinary approach, often involving surgeons, oncologists, and gastroenterologists, is commonly employed.
- Surgical Procedures: Surgical resection, the removal of the cancerous tumor and surrounding tissue, is a cornerstone of colon cancer treatment. The specific surgical approach varies based on the location and extent of the tumor. Colectomy, the surgical removal of part or all of the colon, is a common procedure. The decision of whether to perform a partial or total colectomy is made on a case-by-case basis.
Surgical options include laparoscopic procedures, which minimize incisions and promote faster recovery.
- Chemotherapy: Chemotherapy drugs target rapidly dividing cancer cells, often used in combination with other treatments to reduce tumor size and prevent recurrence. The specific chemotherapy regimen is tailored to the individual patient’s needs.
- Radiation Therapy: Radiation therapy uses high-energy beams to damage cancer cells, often used in conjunction with surgery or chemotherapy to eliminate remaining cancer cells and reduce the risk of recurrence. The type and dosage of radiation therapy are carefully planned to minimize damage to healthy tissues.
- Targeted Therapies: Targeted therapies are designed to specifically attack cancer cells, often used to treat advanced colon cancer or when other treatments have not been effective. These therapies often focus on specific genetic mutations or molecular pathways involved in cancer growth.
Lifestyle Modifications for IBS Management
Lifestyle modifications play a vital role in managing IBS symptoms. Maintaining a healthy diet, regular exercise, and stress reduction techniques can significantly improve quality of life for individuals with IBS.
- Dietary Strategies: Maintaining a balanced diet with adequate fiber intake, avoiding trigger foods, and managing portion sizes are important dietary strategies for managing IBS symptoms.
- Regular Exercise: Regular physical activity is beneficial for IBS management, promoting overall well-being and potentially reducing symptom severity.
- Stress Reduction Techniques: Stress reduction techniques, including yoga, meditation, and mindfulness, can help manage the impact of stress on IBS symptoms.
Comparison of Treatment Efficacy
The efficacy of treatments for IBS and colon cancer differs significantly. IBS treatments primarily focus on symptom management, while colon cancer treatments aim to eradicate the disease and prevent recurrence. The success rates of colon cancer treatments are highly dependent on the stage of the cancer at diagnosis. Early detection and prompt treatment significantly improve survival rates.
| Treatment | IBS Effect | Colon Cancer Effect | Success Rate |
|---|---|---|---|
| Dietary Modifications | Symptom reduction | Improved gut health | Variable |
| Stress Management | Symptom reduction | Improved overall health | Variable |
| Medications (IBS) | Symptom relief | N/A | Variable |
| Surgical Resection (Colon Cancer) | N/A | Tumor removal | High (early stage) |
| Chemotherapy (Colon Cancer) | N/A | Cancer cell destruction | Variable (depends on stage) |
Prevention and Management
Navigating the complexities of both Irritable Bowel Syndrome (IBS) and colon cancer requires a multifaceted approach encompassing preventative measures, symptom management, and early detection strategies. Understanding the interplay between these conditions allows for proactive steps to minimize risk and enhance overall well-being. Proactive measures can significantly impact the trajectory of both diseases.Effective management of these conditions involves a commitment to a holistic lifestyle that integrates dietary adjustments, stress reduction techniques, and regular check-ups.
The key is to identify and address potential triggers for both conditions, fostering a healthier and more balanced life.
Preventative Measures for Colon Cancer
Colon cancer prevention centers on lifestyle choices and regular screenings. A diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, plays a crucial role in reducing the risk. Maintaining a healthy weight and avoiding excessive alcohol consumption are also important factors. Regular screening, such as colonoscopies, is essential for early detection, as early intervention significantly improves treatment outcomes.
Genetic predispositions can also increase the risk, necessitating close monitoring and potentially earlier screening in at-risk individuals.
Strategies for Managing IBS Symptoms, Ibs vs colon cancer
Effective IBS symptom management often involves a personalized approach tailored to individual needs. Dietary modifications are crucial, focusing on identifying and eliminating trigger foods. Stress management techniques, such as meditation or yoga, can help mitigate the impact of stress on IBS symptoms. Over-the-counter medications or prescription therapies, when appropriate, can aid in symptom control. Keeping a detailed symptom diary can help track patterns and identify potential triggers, facilitating more effective management strategies.
Importance of Early Detection for Colon Cancer
Early detection of colon cancer is critical. Early-stage cancers are often easier to treat, with higher rates of successful outcomes. Regular screenings, such as colonoscopies, can detect precancerous polyps, allowing for their removal before they develop into cancerous tumors. This proactive approach significantly improves the chances of successful treatment and a positive prognosis.
Role of Regular Check-ups and Screenings
Regular check-ups and screenings are vital for both overall health and early disease detection. They provide opportunities for preventive care, including discussions about lifestyle modifications and risk factors. For colon cancer, regular screenings, such as colonoscopies, are recommended for individuals at average risk starting at age 45. For those with a family history or other risk factors, earlier and more frequent screenings might be necessary.
This proactive approach can identify potential issues early, allowing for timely intervention and potentially preventing the development of serious conditions.
Managing IBS Triggers
Identifying and managing IBS triggers is paramount for effective symptom control. Keeping a detailed food diary can help pinpoint specific foods or dietary patterns that exacerbate symptoms. Stress management techniques, such as relaxation exercises or mindfulness practices, can help mitigate the impact of stress on IBS symptoms. Furthermore, regular physical activity and a healthy sleep schedule contribute to overall well-being and can reduce the intensity of IBS symptoms.
Working with a healthcare professional to develop a personalized management plan can be beneficial.
Lifestyle Recommendations for Preventing Both IBS and Colon Cancer
| Recommendation | IBS Benefit | Colon Cancer Benefit | Difficulty Level |
|---|---|---|---|
| High Fiber Diet | Improves bowel regularity, reduces bloating and gas | Reduces risk of colon cancer by promoting healthy digestion and preventing constipation | Medium |
| Regular Exercise | Reduces stress, improves digestion, and increases energy levels | Maintains a healthy weight, reduces inflammation, and improves overall health | Medium |
| Stress Management Techniques | Reduces anxiety and stress-related IBS symptoms | Reduces inflammation and stress, which are linked to cancer risk | High |
| Hydration | Improves bowel movements, reduces constipation and bloating | Supports overall bodily functions, crucial for cellular health | Low |
| Limit Processed Foods | Reduces potential IBS triggers | Reduces intake of unhealthy fats and additives | Medium |
| Maintain a Healthy Weight | Reduces abdominal discomfort and bloating | Reduces risk factors for both IBS and colon cancer | High |
Long-Term Impact: Ibs Vs Colon Cancer
Living with IBS or colon cancer significantly impacts a person’s life, extending beyond the immediate diagnosis and treatment. The long-term effects can be physical, emotional, and social, requiring patients to adapt and navigate a new normal. Understanding these impacts is crucial for providing comprehensive care and support.
Long-Term Effects of IBS on Quality of Life
IBS can lead to chronic discomfort and unpredictable symptoms, impacting daily activities and relationships. The fluctuating nature of symptoms can cause anxiety and stress, potentially affecting sleep patterns and overall well-being. Some individuals may experience a reduced ability to participate in social activities due to the unpredictability of their symptoms. Furthermore, the need for frequent bathroom trips can disrupt work and social schedules.
Dietary restrictions and lifestyle modifications can also create adjustments and challenges. Managing IBS effectively often requires ongoing adjustments to diet, stress management techniques, and medical interventions.
Long-Term Effects of Colon Cancer Treatment
Colon cancer treatment, including surgery, chemotherapy, and radiation, can have lasting physical consequences. Fatigue, nausea, and pain are common side effects that can persist for weeks or months after treatment. Some patients experience long-term digestive issues, such as bowel incontinence or changes in bowel habits. Furthermore, treatment can affect the patient’s ability to perform everyday tasks. The emotional toll of a cancer diagnosis and treatment can be significant, leading to anxiety, depression, and feelings of isolation.
Reconstructing a sense of normalcy and adjusting to a new body image can be long and challenging processes.
Psychological Impact of IBS or Colon Cancer Diagnosis
A diagnosis of IBS or colon cancer can trigger a range of psychological responses. Anxiety, fear, and depression are common, often exacerbated by the uncertainty surrounding the conditions. The potential for long-term health issues and the disruption of daily life can lead to feelings of hopelessness and isolation. Patients may also experience body image issues, particularly following cancer treatment.
Maintaining a positive outlook and adapting to a changed lifestyle requires considerable emotional strength and resilience. Support groups and counseling can play a vital role in helping patients cope with these emotions.
Support Systems for Patients
Access to strong support systems is crucial for patients with either condition. Family and friends can offer invaluable emotional support and practical assistance. Support groups provide a safe space for patients to share experiences, offer encouragement, and learn coping strategies from others facing similar challenges. Professional counselors and therapists can offer guidance and strategies to manage stress, anxiety, and other psychological impacts.
Healthcare providers play a critical role in connecting patients with appropriate support services.
Coping Mechanisms
Developing effective coping mechanisms is essential for managing the long-term impacts of IBS or colon cancer. These can include stress-reduction techniques such as meditation, yoga, or deep breathing exercises. Maintaining a healthy diet and regular exercise routine can help improve overall well-being. Connecting with others who understand the challenges can offer invaluable emotional support. Journaling, creative outlets, and maintaining a sense of humor can also contribute to coping strategies.
Potential Long-Term Effects
| Condition | Physical Impact | Psychological Impact | Social Impact |
|---|---|---|---|
| IBS | Chronic abdominal pain, bloating, diarrhea, constipation, fatigue, sleep disturbances, potential for reduced quality of life. | Anxiety, depression, stress, feelings of isolation, difficulty maintaining relationships due to unpredictable symptoms. | Potential limitations in social activities, work, and travel due to symptom unpredictability. Dietary restrictions may affect social gatherings. |
| Colon Cancer | Fatigue, nausea, pain, digestive issues (bowel incontinence, changes in bowel habits), potential for long-term physical limitations, body image issues. | Anxiety, depression, fear, feelings of isolation, emotional distress, body image issues, potential for financial strain. | Potential impact on social activities, relationships, and work due to treatment and potential physical limitations. Changes in daily routines and interactions with others. |
Final Conclusion
In conclusion, while both IBS and colon cancer can cause significant discomfort and concern, their underlying causes, symptoms, and treatment paths differ significantly. This comparison underscores the critical importance of accurate diagnosis and emphasizes the role of early detection and proactive management in both conditions. Armed with a better understanding of the key distinctions, individuals can take informed steps toward improving their health and well-being.
Ultimately, early diagnosis and proactive management are paramount to optimizing outcomes in both IBS and colon cancer.