Thyroid hormones metabolism and weight are intricately linked. This exploration delves into the complex relationship between thyroid hormones, metabolism, and body weight, examining the biochemical pathways involved, the impact of imbalances, and various factors that influence thyroid function. Understanding this connection is crucial for managing weight and overall well-being.
We’ll cover everything from the role of thyroid hormones in regulating basal metabolic rate to the mechanisms by which they influence appetite. Further, we’ll explore the impact of different factors like diet, stress, and lifestyle on thyroid function. Finally, we’ll discuss common diagnostic methods, treatment options, and illustrative cases.
Introduction to Thyroid Hormones and Metabolism

The thyroid gland, a butterfly-shaped organ located in the neck, plays a crucial role in regulating numerous metabolic processes throughout the body. Its primary function is to produce thyroid hormones, which act as chemical messengers, influencing the rate of cellular activity. These hormones are essential for maintaining a healthy basal metabolic rate, impacting everything from energy expenditure to body temperature.Thyroid hormones exert their influence by interacting with specific receptors within cells, ultimately affecting gene expression and cellular function.
This intricate process involves a cascade of biochemical reactions, ensuring precise control over metabolic activity. Understanding these processes is vital for comprehending how thyroid imbalances can impact overall health.
Role of Thyroid Hormones in Regulating Metabolism
Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), are crucial for regulating basal metabolic rate (BMR). Their influence extends to diverse metabolic pathways, impacting protein synthesis, carbohydrate and lipid metabolism, and cellular respiration. A well-functioning thyroid gland ensures optimal energy production and utilization, thereby supporting various bodily functions.
Understanding how thyroid hormones impact weight can be tricky, but it’s often a factor in overall health. Sometimes, other conditions like vitiligo, a skin condition where pigment is lost, can make explaining the connection between hormones and weight to others a little more nuanced. Learning how to explain vitiligo to others can help create a supportive environment for those dealing with the condition, which is key for maintaining a healthy lifestyle, ultimately affecting thyroid hormone metabolism and weight management.
explaining vitiligo to others This is just one piece of the puzzle in managing overall health and well-being.
Thyroid Hormone Synthesis, Transport, and Action
The synthesis of thyroid hormones is a complex process that involves the uptake of iodine from the bloodstream. This iodine is incorporated into tyrosine residues within the thyroid gland, forming the precursor molecules for T3 and T4. These hormones are then released into the bloodstream, where they bind to specific transport proteins, primarily thyroxine-binding globulin (TBG), for delivery to target tissues.
At the cellular level, thyroid hormones bind to intracellular receptors, triggering a cascade of intracellular signaling events that regulate gene expression and metabolic activity. This intricate process ensures a tightly regulated response to the body’s metabolic demands.
Relationship Between Thyroid Hormones and Basal Metabolic Rate
Basal metabolic rate (BMR) is the rate at which the body expends energy at rest. Thyroid hormones directly influence BMR. Increased levels of thyroid hormones lead to a higher BMR, promoting greater energy expenditure. Conversely, decreased levels of thyroid hormones result in a lower BMR, reducing energy expenditure. This relationship highlights the critical role of thyroid hormones in maintaining energy balance within the body.
Types of Thyroid Hormones and Their Functions
| Hormone | Abbreviation | Structure | Primary Function |
|---|---|---|---|
| Thyroxine | T4 | Four iodine atoms | Precursor hormone; converted to T3 |
| Triiodothyronine | T3 | Three iodine atoms | More potent form; directly interacts with receptors |
| Reverse triiodothyronine | rT3 | Three iodine atoms | Inactive form; produced from T4; inhibits T3 action |
Key Enzymes and Proteins Involved in Thyroid Hormone Metabolism
The metabolism of thyroid hormones involves a network of enzymes and proteins. These molecules facilitate the synthesis, transport, and degradation of thyroid hormones. Their precise regulation is crucial for maintaining hormonal balance.
| Enzyme/Protein | Role | Location | Function |
|---|---|---|---|
| Thyroid peroxidase (TPO) | Iodine organification | Thyroid gland | Catalyzes the incorporation of iodine into tyrosine residues |
| Deiodinases (DIO1, DIO2, DIO3) | Conversion of T4 to T3 | Various tissues | Crucial for activating and inactivating T4 and T3 |
| Thyroxine-binding globulin (TBG) | Transport protein | Bloodstream | Binds and transports T4 and T3 |
Thyroid Hormones and Weight Regulation
Thyroid hormones play a crucial role in regulating metabolism, influencing nearly every function in the body, including weight management. Their impact extends beyond simply controlling how quickly your body burns calories; they also affect appetite, energy expenditure, and the way your body stores and utilizes nutrients. Understanding how these hormones affect weight is vital for anyone experiencing fluctuations in their weight or struggling with thyroid-related issues.Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), act as a catalyst for various metabolic processes.
They influence the body’s basal metabolic rate (BMR), which is the number of calories your body burns at rest. When thyroid hormone levels are optimal, the BMR is higher, leading to a faster calorie burn and, in turn, potential weight maintenance or loss. Conversely, imbalances in thyroid hormones can significantly impact weight regulation, sometimes leading to substantial changes in body weight.
Mechanisms of Thyroid Hormone Influence on Weight
Thyroid hormones stimulate the breakdown of fats, carbohydrates, and proteins, accelerating the metabolic rate. This increased metabolic activity directly influences energy expenditure, and subsequently, weight. They also impact the absorption and utilization of nutrients, affecting how efficiently the body converts food into energy. Additionally, thyroid hormones influence the activity of other hormones, including those involved in appetite regulation and fat storage.
The interplay between these hormones is complex, and imbalances can manifest in various ways.
Impact of Thyroid Hormone Imbalances on Body Weight
Disruptions in thyroid hormone levels can have a significant impact on body weight. Hypothyroidism, a condition characterized by insufficient thyroid hormone production, often results in weight gain. Conversely, hyperthyroidism, where the thyroid produces excessive hormones, typically leads to weight loss. These effects are not always straightforward, as other factors such as diet, lifestyle, and underlying health conditions can influence the observed weight changes.
Comparison of Hypothyroidism and Hyperthyroidism Effects on Weight
- Hypothyroidism: Individuals with hypothyroidism often experience a slowing of metabolic processes, resulting in decreased energy expenditure and a tendency to gain weight. The decreased metabolism can make it harder to lose weight even with dietary changes and exercise. A common observation is a gradual increase in body weight over time. Weight gain may be accompanied by other symptoms, such as fatigue, cold intolerance, and constipation.
- Hyperthyroidism: In contrast, hyperthyroidism leads to an accelerated metabolism, which results in increased energy expenditure and a tendency to lose weight, even when dietary habits remain unchanged. Individuals with hyperthyroidism may experience rapid weight loss and often report an increased appetite. This can be a paradoxical symptom, as the increased metabolic rate requires more calories, which is often not met by the appetite.
Other symptoms include anxiety, heat intolerance, and increased heart rate.
Role of Thyroid Hormones in Appetite Regulation
Thyroid hormones play a role in regulating appetite by influencing the production and action of other hormones that control hunger and satiety. These hormones can directly affect appetite-regulating centers in the brain. Dysfunction in this hormonal interplay can result in altered appetites, which in turn can contribute to weight fluctuations. In cases of hypothyroidism, decreased metabolic activity can result in decreased appetite, and in hyperthyroidism, an increased appetite might be observed.
Thyroid hormones play a crucial role in metabolism, and that directly affects weight. Understanding how your thyroid functions is key to effective weight management, but it’s also important to consider how long it takes to see results. Factors like diet, exercise, and your body’s unique response to changes all influence how long it takes to lose weight, how long does it take to lose weight.
Ultimately, a healthy approach to weight loss, incorporating a balanced diet and regular exercise, combined with understanding your thyroid’s influence, is the best strategy for long-term success.
Connection between Thyroid Hormone Levels and Energy Expenditure, Thyroid hormones metabolism and weight
Thyroid hormones directly impact the body’s basal metabolic rate (BMR). A higher level of thyroid hormones results in a higher BMR, meaning the body burns more calories at rest. This increased energy expenditure can lead to weight loss or difficulty in gaining weight. Conversely, lower thyroid hormone levels result in a lower BMR, and the body burns fewer calories at rest, which may lead to weight gain.
Symptoms of Hypothyroidism and Hyperthyroidism Related to Weight
| Symptom | Hypothyroidism | Hyperthyroidism | Description |
|---|---|---|---|
| Weight Change | Gain | Loss | Significant weight fluctuations in either direction |
| Appetite | Decreased | Increased | Change in the desire to eat |
| Energy Levels | Low | High | Differences in energy levels and fatigue |
| Metabolic Rate | Decreased | Increased | Impact on the body’s calorie-burning rate |
Factors Affecting Thyroid Hormone Metabolism and Weight
Maintaining a healthy weight is often intertwined with a well-functioning thyroid gland. Thyroid hormones play a crucial role in regulating metabolism, influencing how the body uses energy and impacting weight. However, various factors can disrupt this delicate balance, leading to fluctuations in thyroid hormone levels and subsequent changes in weight. Understanding these influences is key to effective weight management and overall health.
Factors Disrupting Thyroid Hormone Balance
Several factors can disrupt the delicate equilibrium of thyroid hormone production and function. These disruptions can stem from dietary choices, lifestyle habits, underlying health conditions, and even medications. Identifying these factors can help individuals take proactive steps to support their thyroid health and achieve a healthy weight.
Thyroid hormones play a crucial role in metabolism and, consequently, weight management. However, sometimes unrelated anxieties can unexpectedly impact our well-being. For example, a fascinating phobia, like the fear of cotton balls (sidonglobophobia), might seem completely out of the blue when considering something like thyroid function and weight, but it’s important to remember that mental health is just as significant as physical health when dealing with weight management issues, and understanding the full spectrum of factors affecting our bodies is key.
Further exploration of these less common anxieties can help in a holistic approach to weight management issues. fear of cotton balls sidonglobophobia. Understanding these complex connections is vital for addressing weight-related concerns effectively.
Impact of Diet on Thyroid Function
Diet significantly impacts thyroid function. Iodine, a crucial mineral for thyroid hormone production, is obtained primarily through diet. A diet deficient in iodine can lead to hypothyroidism, hindering the body’s ability to produce adequate thyroid hormones. Conversely, an excessive intake of certain foods, particularly goitrogens (found in foods like cabbage, broccoli, and cauliflower), may interfere with iodine absorption, potentially impacting thyroid function.
A balanced diet rich in essential nutrients, including iodine, is crucial for maintaining optimal thyroid health.
Impact of Stress on Thyroid Function
Chronic stress can negatively affect thyroid function. Stress hormones, such as cortisol, can influence thyroid hormone production and metabolism. Prolonged periods of stress may lead to imbalances in the hypothalamic-pituitary-thyroid (HPT) axis, a crucial regulatory pathway for thyroid hormone production. Stress management techniques, such as exercise, mindfulness, and relaxation, can help mitigate the negative effects of stress on thyroid health.
Role of Nutrient Deficiencies in Thyroid Hormone Production
Nutrient deficiencies can also impair thyroid hormone production. Selenium, zinc, and vitamin A are essential nutrients for optimal thyroid function. Deficiencies in these nutrients can hinder the conversion of thyroid hormone precursors into active thyroid hormones. Ensuring adequate intake of these essential nutrients through a varied diet or supplementation, when necessary, can support thyroid health.
Connection Between Thyroid Hormones and Gut Health
The gut microbiome plays a significant role in overall health, including thyroid function. Research suggests a strong correlation between gut health and thyroid function. Imbalances in the gut microbiome can potentially impact thyroid hormone metabolism and regulation. Maintaining a healthy gut microbiome through a balanced diet rich in fiber, probiotics, and prebiotics can support thyroid health.
Impact of Medications on Thyroid Hormone Levels
Certain medications can interact with thyroid hormones, either by affecting their production or metabolism. For instance, some medications can interfere with iodine absorption or the conversion of thyroid hormones. Individuals taking medications should discuss potential interactions with their healthcare providers to ensure appropriate management of thyroid function.
Common Causes of Thyroid Dysfunction and Their Effects on Weight
| Cause | Mechanism | Effect on Weight | Additional Notes |
|---|---|---|---|
| Iodine deficiency | Reduced thyroid hormone production | Weight gain, fatigue, and cold intolerance. | Common in regions with low iodine in soil. |
| Hashimoto’s thyroiditis | Autoimmune attack on thyroid gland | Weight gain, fatigue, and cold intolerance. | Often associated with inflammation and immune system dysfunction. |
| Grave’s disease | Overactive thyroid | Weight loss, increased appetite, and heat intolerance. | Often associated with autoimmune dysfunction and rapid metabolism. |
| Thyroid nodules | Abnormal growth of thyroid tissue | Weight gain or loss depending on hormone production. | May require further investigation and treatment. |
Diagnosis and Management of Thyroid-Related Weight Issues: Thyroid Hormones Metabolism And Weight
Understanding the intricate link between thyroid hormones and weight regulation is crucial for effective management. Thyroid disorders, whether hypothyroidism or hyperthyroidism, can significantly impact metabolism and, consequently, body weight. Accurate diagnosis and tailored treatment plans are essential for regaining and maintaining a healthy weight.Effective management of thyroid-related weight issues necessitates a comprehensive approach that combines medical interventions with lifestyle modifications.
This involves accurate diagnosis, appropriate treatment of the underlying thyroid condition, and strategies for managing weight effectively.
Common Methods for Diagnosing Thyroid Disorders
Diagnosing thyroid disorders involves a combination of physical examinations, blood tests, and sometimes, imaging techniques. A physical exam often includes checking for any visible signs of thyroid abnormalities, such as a goiter (enlarged thyroid gland). Blood tests are crucial for evaluating thyroid hormone levels.
Evaluating Thyroid Hormone Levels
Evaluating thyroid hormone levels is a critical step in diagnosing thyroid disorders. Blood tests measure the levels of thyroid-stimulating hormone (TSH), thyroxine (T4), and triiodothyronine (T3). An elevated TSH level often indicates hypothyroidism, while a suppressed TSH level can suggest hyperthyroidism. T4 and T3 levels are also assessed to confirm the diagnosis and monitor treatment effectiveness. Understanding the specific levels of these hormones provides valuable insights into the underlying thyroid condition.
Common Treatment Approaches for Thyroid Disorders
Treatment for thyroid disorders focuses on restoring hormonal balance. For hypothyroidism, hormone replacement therapy with levothyroxine (T4) is a common approach. In hyperthyroidism, treatments such as radioactive iodine therapy, anti-thyroid medications, or surgery may be considered, depending on the specific condition and individual circumstances. The selection of treatment depends on factors like the severity of the condition, patient preferences, and potential risks and benefits.
Strategies for Managing Weight in Individuals with Thyroid Imbalances
Managing weight in individuals with thyroid imbalances requires a multifaceted approach that addresses both the underlying hormonal issues and lifestyle factors. Maintaining a balanced diet and regular exercise are crucial. Specific dietary recommendations and exercise routines tailored to individual needs and circumstances can significantly improve weight management outcomes.
Treatment Options for Hypothyroidism and Hyperthyroidism
| Treatment | Mechanism of Action | Potential Side Effects | Typical Duration |
|---|---|---|---|
| Levothyroxine (Hypothyroidism) | Replaces deficient thyroid hormone | Initially, mild nausea, anxiety, or palpitations. Long-term, if dosage is not correct, may cause osteoporosis or cardiac issues. | Lifelong |
| Radioactive Iodine (Hyperthyroidism) | Damages thyroid cells to reduce hormone production | Temporary discomfort in the throat, possible hypothyroidism after treatment. | Short-term |
| Anti-thyroid Medications (Hyperthyroidism) | Inhibit thyroid hormone production | Rash, nausea, fatigue, or liver problems. | Variable, often until remission or symptom control |
| Surgery (Hyperthyroidism) | Surgical removal of part or all of the thyroid gland | Risk of scarring, nerve damage, or hypothyroidism. | Short-term |
Dietary Recommendations for Individuals with Thyroid Conditions
A balanced diet plays a vital role in managing thyroid-related weight issues. Nutritional strategies can support thyroid function and promote healthy weight management.
| Nutrient | Importance | Food Sources | Considerations |
|---|---|---|---|
| Iodine | Essential for thyroid hormone production | Seafood, iodized salt, dairy products | Excessive iodine intake can be problematic |
| Selenium | Supports thyroid function | Brazil nuts, tuna, eggs | Important for antioxidant support |
| Zinc | Crucial for thyroid function and metabolism | Oysters, beef, pumpkin seeds | Adequate intake is necessary |
| Fiber | Promotes satiety and digestive health | Fruits, vegetables, whole grains | Can help with weight management |
Illustrative Cases and Examples
Understanding how thyroid hormone imbalances affect weight requires looking at real-life scenarios. This section presents case studies of individuals with hypothyroidism and hyperthyroidism, highlighting the diverse presentations and complexities of these conditions. It also explores the importance of a holistic approach when managing thyroid-related weight issues.Case studies provide valuable insights into the individual experiences of thyroid disorders. By analyzing the symptoms, physical characteristics, and overall health context, we can better understand the nuances of these conditions and develop more comprehensive management strategies.
Hypothyroidism Case Study: Sarah
Sarah, a 35-year-old woman, presented with increasing fatigue, cold intolerance, and constipation. She also reported experiencing significant weight gain over the past year, despite maintaining a consistent diet and exercise routine. Blood tests revealed a significantly low level of thyroid hormones (TSH elevated, T3 and T4 suppressed). After initiating thyroid hormone replacement therapy, Sarah experienced a gradual improvement in her symptoms, including reduced fatigue, improved digestion, and a steady decline in weight.
This demonstrates the impact of hypothyroidism on metabolism and the positive effects of treatment.
Hyperthyroidism Case Study: David
David, a 45-year-old man, presented with nervousness, tremors, and an increased appetite, accompanied by significant weight loss despite increased caloric intake. He also reported difficulty sleeping and experienced frequent bowel movements. Blood tests revealed elevated levels of thyroid hormones (TSH suppressed, T3 and T4 elevated). Treatment involved anti-thyroid medications to reduce hormone production, which led to a gradual normalization of his symptoms and weight stabilization.
This showcases how hyperthyroidism can disrupt metabolic processes and lead to weight loss.
Comparison of Case Studies
| Characteristic | Sarah (Hypothyroidism) | David (Hyperthyroidism) | Key Differences |
|---|---|---|---|
| Weight | Significant weight gain | Significant weight loss | Directly opposite effects on weight |
| Energy Level | Low energy, fatigue | High energy, nervousness | Opposite effects on energy levels |
| Body Temperature | Cold intolerance | Heat intolerance | Differences in thermal regulation |
| Appetite | Decreased appetite, possibly | Increased appetite | Significant differences in appetite regulation |
| Bowel Movements | Constipation | Diarrhea | Opposite effects on digestive system |
Co-existing Health Concerns and Weight
A patient with hypothyroidism might also have a condition like depression, which could affect appetite and activity levels, influencing weight management. Similarly, a patient with hyperthyroidism might have an underlying condition like celiac disease, which impacts nutrient absorption, further complicating weight control. These examples demonstrate the importance of a holistic approach to managing thyroid-related weight issues, considering the individual’s overall health.
Holistic Approach to Management
Managing thyroid-related weight issues requires a multifaceted approach that addresses both the thyroid condition and any co-existing health problems. A balanced diet, regular exercise, stress management techniques, and appropriate medication are crucial components of a successful treatment plan. A healthcare provider can help design a personalized plan based on the patient’s specific needs and circumstances. This approach recognizes that weight management is a complex issue and that individual factors need careful consideration.
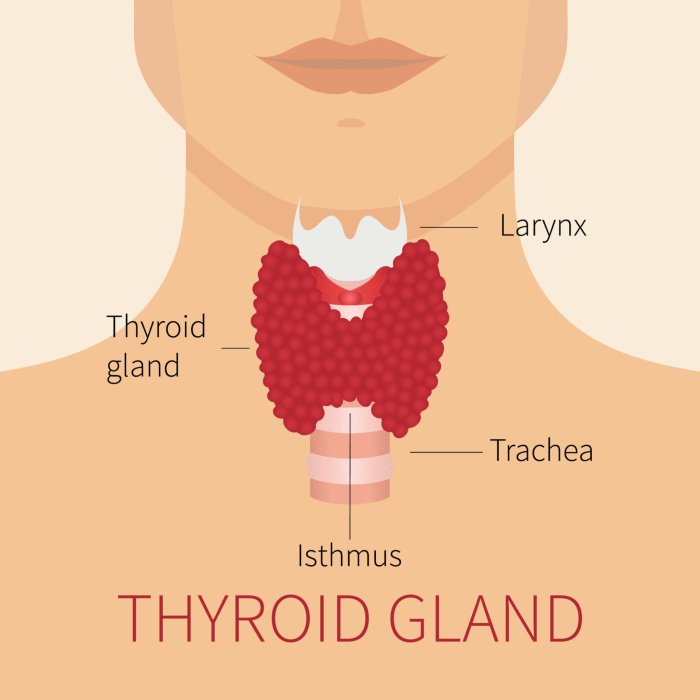
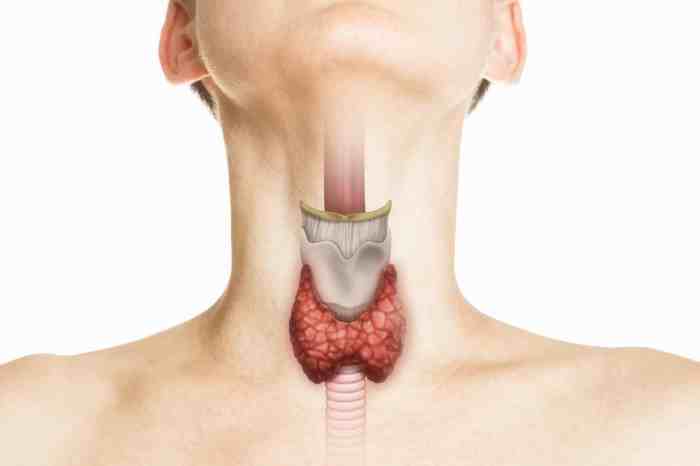
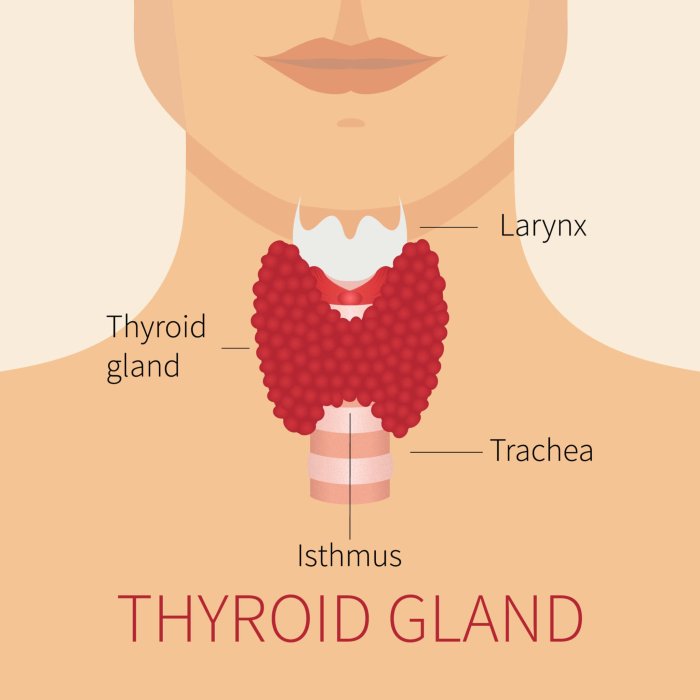
Thyroid Gland Structure
The thyroid gland is a butterfly-shaped gland located in the anterior neck, just below the Adam’s apple. It consists of two lobes connected by a narrow isthmus. The gland’s structure comprises numerous follicles filled with colloid, a protein-rich substance containing the precursor to thyroid hormones. Surrounding the follicles are specialized cells, called parafollicular cells, which produce calcitonin, a hormone involved in calcium regulation.
The intricate structure of the gland plays a vital role in the production and release of thyroid hormones.
Metabolic Pathway of Thyroid Hormones
The metabolic pathway of thyroid hormones involves several steps, beginning with the uptake of iodine from the bloodstream. Iodine is incorporated into tyrosine residues within the thyroid gland, forming thyroglobulin, a large protein. Enzymatic reactions then lead to the production of thyroxine (T4) and triiodothyronine (T3). T4 is converted to T3 in peripheral tissues, the active form of the hormone.
This pathway is crucial for regulating various metabolic processes in the body, including energy expenditure and temperature regulation.
Final Wrap-Up
In conclusion, the intricate dance between thyroid hormones and weight regulation is a complex one. By understanding the intricate mechanisms and factors affecting thyroid hormone balance, we can better address weight issues associated with thyroid imbalances. This in-depth look highlights the importance of a holistic approach to managing thyroid-related weight challenges, emphasizing the role of diet, lifestyle, and appropriate medical interventions.
The interplay between thyroid function and weight is a significant aspect of health, and understanding this connection is essential for informed decisions about health and wellness.