HPV vaccine schedule age is a crucial factor in protecting against human papillomavirus (HPV). Understanding the recommended vaccination schedule for different age groups is essential for maximizing the benefits of this preventative measure. This guide explores the various HPV vaccine types, optimal ages for receiving the shots, and catch-up schedules for those who missed initial doses. We’ll also delve into the reasons behind age-specific schedules, including immune response differences and developmental stages.
Finally, we’ll cover vaccine safety, potential side effects, and additional considerations.
The schedule isn’t a one-size-fits-all approach; it’s tailored to different life stages. Knowing the specific age ranges and recommended dose schedules can significantly impact the effectiveness of the HPV vaccine. This article will provide a detailed breakdown, helping you understand the nuances of the HPV vaccine schedule and make informed decisions about your health.
Introduction to HPV Vaccine Schedules: Hpv Vaccine Schedule Age

The human papillomavirus (HPV) vaccine is a crucial tool in preventing cervical cancer and other HPV-related cancers and diseases. It works by protecting against various types of HPV, which are sexually transmitted infections. Understanding the appropriate vaccination schedules for different age groups is essential for maximizing the vaccine’s effectiveness.Vaccination schedules are tailored to optimize immune response and provide long-term protection.
This tailored approach is vital because the effectiveness of the vaccine can vary depending on the individual’s age and the specific type of vaccine received.
HPV Vaccine Types
Different types of HPV vaccines exist, each targeting a specific set of HPV strains. This targeted approach allows for greater protection against the various forms of HPV. Gardasil, Gardasil 9, and Cervarix are the most commonly used types. Gardasil 9 is the most recent version and is recommended due to its broader coverage of high-risk HPV types.
Recommended Ages for HPV Vaccination
The recommended ages for HPV vaccination vary depending on the individual’s circumstances and whether they have already received prior doses. Ideally, vaccination should occur before the onset of sexual activity, as this significantly reduces the risk of contracting HPV.
HPV Vaccination Schedule Table
The table below Artikels the recommended age ranges and number of doses for various HPV vaccines. This information is essential for parents and healthcare providers to ensure timely and complete vaccination.
| Vaccine Type | Recommended Age Range | Number of Doses |
|---|---|---|
| Gardasil 9 | 9-45 years | 2 or 3 doses |
| Gardasil 9 (previously vaccinated) | Individuals previously vaccinated with a 2-dose regimen should receive a 3rd dose at least 6 months after the 2nd dose | 3 doses |
| Cervarix | 9-45 years | 2 doses |
Vaccine Schedules by Age Group
Understanding the recommended HPV vaccination schedules is crucial for maximizing protection against this potentially serious viral infection. Proper timing and completion of the series are essential for building immunity and preventing future health complications. The schedules are designed to optimize efficacy and safety, taking into account the developing immune systems of different age groups.The schedules are tailored to different age groups, recognizing that the immune response and developmental factors can influence the effectiveness and safety of the vaccine.
This allows for optimized protection and safety for individuals at various stages of development.
Recommended Schedules for Adolescents and Young Adults
The HPV vaccination series is typically most effective when administered before exposure to the virus. For adolescents and young adults, the schedule aims to establish immunity before potential exposure. This is often why the vaccination is recommended for younger individuals.
| Age Group | Recommended Schedule | Catch-up Recommendations |
|---|---|---|
| Adolescents (11-12 years) | Two doses, given 6-12 months apart. | Individuals who start the series later can complete it with the standard two-dose schedule, provided at least six months separate the doses. |
| Young Adults (13-26 years) | Three doses, given over a period of time, typically zero to six months between the first and second dose, and six months to 12 months between the second and third dose. | Individuals who start the series later can complete it with the standard three-dose schedule, with proper time intervals between doses. |
Recommended Ages for Catching Up on Missed Doses
Individuals who have not received the HPV vaccine as recommended can still receive the vaccine. Catching up is important for protecting against HPV infection.Catching up on missed doses is possible, regardless of the age at which the vaccination series is initiated. The crucial factor is ensuring the appropriate time intervals between doses, as per the recommended schedule.
Timing of Doses for Adolescents
The two-dose HPV vaccination series for adolescents is given at least six months apart. The recommended schedule aims to maximize the immune response and provide the best protection possible.The first dose can be given at any time within the recommended age range, typically at 11 or 12 years old. The second dose is administered six months after the first dose.
Comparison of Schedules for Males and Females
The recommended schedules for males and females are the same. Both benefit from receiving the HPV vaccine series. Both genders are susceptible to HPV infection and its potential complications.Both males and females are recommended to follow the same HPV vaccination schedule. This approach is designed to maximize the protection against HPV-related diseases for both genders.
Knowing the HPV vaccine schedule by age is crucial for protection, but did you know that topical treatments like tranexamic acid for skin can help with skin concerns ? While the vaccine is focused on preventing HPV, which can lead to certain cancers, understanding the optimal vaccination schedule for various age groups is key. Ultimately, staying informed about both preventative measures like vaccines and potential skin treatments like tranexamic acid is important for overall well-being, especially as you consider the HPV vaccine schedule for your family.
Recommended HPV Vaccination Schedules by Age Group
| Age Group | Dose 1 | Dose 2 | Dose 3 (if applicable) |
|---|---|---|---|
| 11-12 years | Anytime within the age range | 6-12 months after Dose 1 | N/A |
| 13-14 years | Anytime within the age range | 6-12 months after Dose 1 | N/A |
| 15-26 years | Anytime within the age range | 1-2 months after Dose 1 | 6 months after Dose 2 |
Reasons Behind Age-Specific Schedules
The recommended age ranges for HPV vaccination are not arbitrary; they are carefully determined based on a multitude of factors. Understanding these factors allows for a deeper appreciation of the rationale behind the schedules and the significance of timely vaccination. Age-specific schedules consider various elements, including the effectiveness of the vaccine, the immune response of individuals at different developmental stages, and the potential risks and benefits of vaccination at different ages.The precise timing of HPV vaccination is crucial for maximizing its impact.
This is because the immune system’s ability to respond to the vaccine and generate protective antibodies can differ significantly across different age groups. Moreover, developmental factors play a significant role in shaping the effectiveness of the vaccine, which is why age-specific recommendations are crucial for ensuring optimal protection.
Factors Influencing Recommended Age Ranges
Various factors contribute to the development of age-specific HPV vaccination schedules. These include the immune response differences across age groups, the potential risks and benefits of vaccination at various ages, and the optimal age for maximum immune response. The ideal age for receiving the vaccine is generally considered to be before the onset of sexual activity.
Immune Response Differences Between Age Groups
The immune system’s capacity to mount an effective response to the HPV vaccine varies across different age groups. Children and adolescents often demonstrate a stronger and more robust immune response to vaccination compared to adults. This increased responsiveness leads to a greater likelihood of developing protective immunity against HPV infections. Research indicates that the immune response is often stronger in younger individuals, leading to a higher probability of generating a long-lasting antibody response.
Developmental Stages and Vaccine Effectiveness
Developmental stages significantly influence vaccine effectiveness. The adolescent and pre-adolescent years mark a period of significant physiological and hormonal changes. These changes can affect the immune system’s ability to respond to vaccination. Additionally, the timing of vaccination may be influenced by factors such as school schedules, parental availability, and logistical considerations.
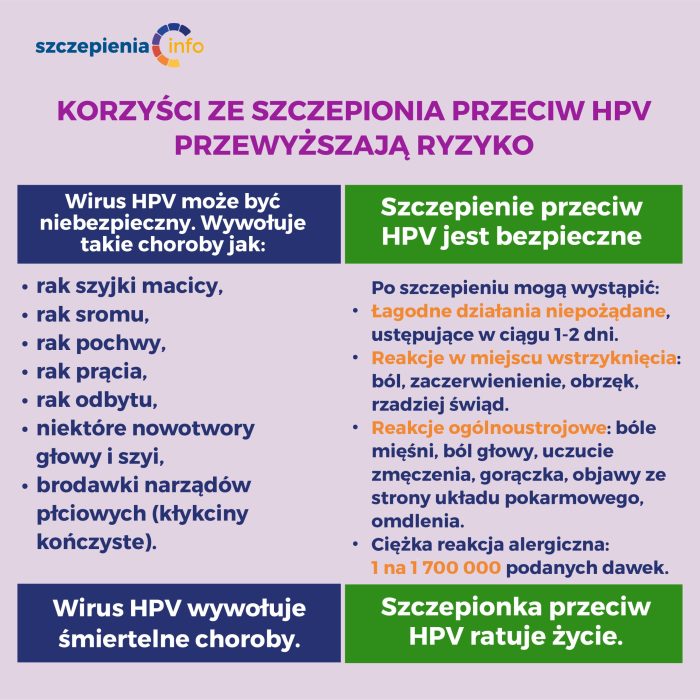
Potential Risks and Benefits of Vaccination at Different Ages
The potential risks and benefits of HPV vaccination vary slightly across different age groups. While the overall risks are low, some individuals may experience mild side effects such as soreness or redness at the injection site. These side effects are typically short-lived and resolve spontaneously. The benefits, however, outweigh the potential risks, particularly when considering the long-term protection against HPV-related cancers and diseases.
Optimal Age for Maximum Immune Response
The optimal age for maximizing the immune response to the HPV vaccine is generally considered to be during pre-adolescence or early adolescence. At these ages, the immune system is typically more responsive to the vaccine, leading to a higher likelihood of developing protective immunity. Early vaccination also provides protection before potential exposure to HPV. For example, studies have shown that adolescents who receive the HPV vaccine before becoming sexually active have a significantly higher rate of developing protective immunity.
Catch-up Vaccination Schedules
Missed the HPV vaccine at the recommended age? Don’t worry, catch-up vaccination schedules are available for individuals who didn’t receive the vaccine during their adolescent years. These schedules allow you to complete the vaccination series later in life, and they’re designed to protect you from HPV-related cancers and diseases. It’s crucial to remember that the catch-up schedule is different from the routine schedule and aims to maximize protection even if vaccination was delayed.Catch-up vaccination schedules provide an opportunity to receive the necessary doses of the HPV vaccine, even if you weren’t vaccinated when you were younger.
Figuring out the HPV vaccine schedule for the right age group can be tricky. It’s important to get the shots on time, and sometimes a bit of research is needed to understand the recommended doses. While we’re on the topic of health concerns, did you know that alcohol can sometimes trigger migraine headaches? For more information on this, check out this helpful resource on alcohol triggers migraine headaches.
Ultimately, staying informed about health guidelines, like the HPV vaccine schedule, is key for overall well-being.
This is an important step to reduce your risk of HPV-related health problems later in life. These schedules are tailored to address the needs of individuals who have missed the recommended vaccination ages.
Catch-up Schedule for Ages 27-45
Individuals aged 27 to 45 who have not been previously vaccinated against HPV can still receive the vaccine. The catch-up schedule for this age group involves a different approach compared to the routine vaccination schedule for younger individuals. This is because the immune response and potential risks might vary.The catch-up vaccination process typically involves receiving the recommended doses of the HPV vaccine, often in a two-dose series, as directed by a healthcare provider.
The exact schedule and number of doses may vary depending on individual circumstances and the specific vaccine brand administered.
Figuring out the HPV vaccine schedule for the right age range can be tricky. It’s crucial to get the shots on time, but sometimes other health issues pop up, like a persistent tickle in my throat. This article about common causes of a tickle in the throat might be helpful if you’re concerned. Ultimately, talking to your doctor about the best HPV vaccination schedule for your situation is key.
Steps to Get Vaccinated Later in Life
The process for getting vaccinated later in life is straightforward. The first step is to schedule an appointment with your healthcare provider. They can assess your medical history and determine if the HPV vaccine is appropriate for you. During the appointment, your healthcare provider will discuss the benefits and potential risks of the vaccine.Once you’ve decided to proceed, your provider will administer the vaccine as per the catch-up schedule.
This usually involves a series of doses over a period of time, following the recommended guidelines for the specific vaccine type. After the vaccination, you may experience some mild side effects, such as pain or redness at the injection site. These are typically temporary and resolve on their own. It’s essential to follow your provider’s instructions regarding aftercare and any potential follow-up appointments.
Comparison of Routine and Catch-up Vaccination Schedules
| Characteristic | Routine Vaccination Schedule (Ages 11-12) | Catch-up Vaccination Schedule (Ages 27-45) |
|---|---|---|
| Number of Doses | Typically 2 doses (with 6-12 months between doses) | May require 2 or 3 doses, depending on individual circumstances and prior vaccination status. |
| Timing | Ideally administered during adolescence | Administered later in life |
| Recommendation | Strongly recommended for adolescents | Recommended for adults who haven’t received the vaccine before. |
| Immune Response | Generally strong immune response in younger individuals. | Immune response may vary and may be less robust compared to younger individuals. |
This table highlights the key differences between routine and catch-up vaccination schedules. The catch-up schedule acknowledges the possibility of a slightly different immune response in adults compared to adolescents. It emphasizes the importance of seeking professional medical advice for personalized guidance.
Vaccine Safety and Side Effects
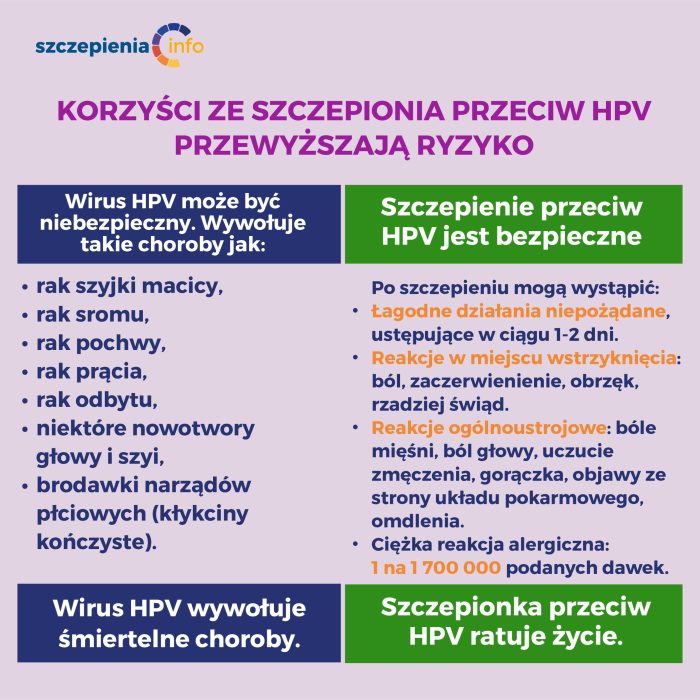
The HPV vaccines are generally considered safe and effective. Rigorous testing and monitoring have been conducted throughout the development and implementation phases to identify potential risks. While some side effects are possible, they are typically mild and temporary. Understanding the safety profile, common reactions, and long-term data is crucial for informed decision-making about vaccination.
Safety Profile of HPV Vaccines
Extensive clinical trials and post-licensure surveillance have consistently demonstrated the safety of HPV vaccines. These vaccines have a strong safety record, with the most common side effects being mild and manageable. The benefits of preventing HPV-related cancers and diseases generally outweigh the potential risks for the vast majority of individuals. The overall safety profile of these vaccines is well-established and aligns with that of other routinely administered vaccines.
Common Side Effects Associated with HPV Vaccination
The most common side effects following HPV vaccination include pain, redness, or swelling at the injection site. These localized reactions are typically mild and resolve within a few days. Other common side effects include fever, fatigue, headache, nausea, and muscle or joint pain. These systemic reactions are also generally mild and temporary. It is important to remember that these reactions are often similar to those experienced after other vaccinations.
Long-Term Safety Data of HPV Vaccines
Long-term safety data collected over several years consistently supports the safety of HPV vaccines. Ongoing surveillance studies and monitoring programs continue to assess the potential for long-term effects. Results to date consistently indicate that the vaccines are safe for use in the recommended age groups. No serious long-term adverse effects have been definitively linked to HPV vaccination.
Management of Potential Side Effects
Mild side effects, such as soreness at the injection site or a low-grade fever, can often be managed at home. Rest, over-the-counter pain relievers (like ibuprofen or acetaminophen), and plenty of fluids can help alleviate discomfort. If symptoms persist or worsen, it’s important to consult a healthcare provider. It is important to note that these are often the same remedies used for other minor ailments.
Importance of Reporting Serious Side Effects
Any serious side effects following HPV vaccination should be immediately reported to a healthcare provider. This includes symptoms such as difficulty breathing, severe allergic reactions (anaphylaxis), or persistent neurological problems. Prompt reporting allows healthcare providers to assess and address any potential issues promptly. The ability to detect and address serious side effects is a critical part of ensuring vaccine safety.
Additional Considerations and Variations
Understanding HPV vaccination schedules requires recognizing that certain medical conditions or circumstances might necessitate adjustments. This section delves into these variations, emphasizing the critical role of healthcare providers in personalized recommendations. Prioritizing patient safety and well-being is paramount in tailoring vaccination strategies to individual needs.Personalizing vaccination schedules is vital to ensure optimal protection against HPV. Medical conditions and individual responses to vaccines can influence the effectiveness and safety of the HPV vaccination series.
Consequently, consulting a healthcare provider before initiating or continuing the vaccination series is crucial.
Variations Based on Medical Conditions
Individual health conditions can impact the HPV vaccination schedule. This necessitates careful consideration and personalized advice from a healthcare professional. The specific needs of each patient should guide the decision-making process.
- Immunocompromised Individuals: Individuals with weakened immune systems, such as those undergoing chemotherapy or with certain chronic illnesses, may require different vaccination schedules or dosage adjustments. The healthcare provider will assess the specific level of immunocompromise and determine the appropriate approach to maximize protection while minimizing potential risks.
- Pregnancy: While the HPV vaccine is generally safe during pregnancy, a healthcare provider may advise delaying vaccination until after delivery. This is to ensure there are no potential risks to the developing fetus and the mother’s health during pregnancy. If a woman becomes pregnant during the vaccination series, she should consult her healthcare provider to discuss the optimal timing for completing the series.
- Allergies: Individuals with a history of severe allergic reactions to any vaccine components or ingredients should inform their healthcare provider. The healthcare provider will assess the severity of the allergy and determine whether vaccination is advisable or if alternative strategies are necessary. In such cases, careful monitoring and alternative vaccination strategies may be required.
Importance of Consulting a Healthcare Provider
A healthcare provider plays a crucial role in tailoring the HPV vaccination schedule to an individual’s specific needs. They possess the knowledge and expertise to assess medical history, potential risks, and benefits, enabling them to provide personalized recommendations.
- Assessing Medical History: A comprehensive medical history is essential to identify potential contraindications or factors that might influence the vaccination schedule. This includes pre-existing conditions, allergies, and any recent illnesses.
- Determining Appropriate Timing: The healthcare provider can determine the optimal timing for the vaccination series, considering the individual’s health status and other scheduled medical procedures. This will ensure the safety and efficacy of the vaccine.
- Providing Personalized Recommendations: Healthcare providers can provide personalized advice on the most suitable vaccination schedule, taking into account the individual’s medical history, current health status, and lifestyle factors. This approach ensures that the vaccination series is safe and effective for each patient.
Potential Contraindications
Certain situations may contraindicate HPV vaccination. Healthcare providers must carefully consider these potential contraindications to ensure patient safety. The decision to vaccinate should always prioritize the well-being of the individual.
- Known hypersensitivity to vaccine components: A history of severe allergic reactions to vaccine components necessitates careful consideration and often prohibits vaccination. This is a significant contraindication that must be taken seriously.
- Severe acute illness: Individuals experiencing a severe acute illness, such as a high fever, should postpone vaccination until they recover to avoid complications. Postponing vaccination during such periods is vital to ensure optimal patient safety.
Role of Healthcare Providers in Personalized Advice
Healthcare providers are essential in providing personalized advice on vaccination schedules. They use their expertise to ensure the safety and efficacy of the HPV vaccination for each individual.
Healthcare providers should thoroughly discuss the risks and benefits of HPV vaccination with each patient, taking into account their unique circumstances and medical history. They must also explain the importance of adhering to the recommended schedule to maximize the effectiveness of the vaccine.
Potential Medical Conditions and Their Influence on Vaccination Schedules
| Medical Condition | Influence on Vaccination Schedule |
|---|---|
| Immunodeficiency | May require adjusted dosage or vaccination schedule, or alternative vaccination strategies |
| Pregnancy | Vaccination is generally safe, but delaying until after delivery is recommended |
| Severe Allergies | Vaccination may be contraindicated or require careful monitoring |
| Active Severe Illness | Vaccination should be postponed until the illness resolves |
| Recent Organ Transplant | May require adjusted vaccination schedule or alternative strategies |
Vaccine Administration and Logistics
Getting your HPV vaccine is a straightforward process, but understanding the logistics involved ensures a smooth and effective experience. Proper administration, storage, and handling procedures are crucial for maintaining vaccine potency and safety. This section delves into the practical aspects of receiving the HPV vaccine.
Administration Procedures
The HPV vaccine is administered by injection, typically into the upper arm. A healthcare professional will use a sterile needle and syringe to inject the vaccine. The injection site will be cleaned with an antiseptic solution before the injection. After the injection, the site may be covered with a bandage. The entire process is generally quick and painless.
Following the injection, the patient should be monitored for any immediate reactions.
Vaccine Location and Process
The HPV vaccine is typically administered at a doctor’s office, a clinic, or a public health center. Trained medical professionals are equipped to administer the vaccine safely and efficiently. The process usually involves a brief consultation with the healthcare provider to discuss the vaccination schedule and any potential health concerns. The patient is then prepared for the injection and closely monitored post-administration for any adverse effects.
Vaccine Storage and Handling
Proper storage and handling of HPV vaccines are essential to maintaining their potency and preventing contamination. HPV vaccines are typically stored in a refrigerator at a specific temperature range to ensure their efficacy. The temperature of the refrigerator should be carefully monitored and maintained within the specified range. Vaccines should be handled with care to avoid any physical damage or contamination.
Dedicated storage areas are usually designated in clinics to ensure optimal storage conditions.
Scheduling HPV Vaccine Appointments, Hpv vaccine schedule age
Scheduling an HPV vaccine appointment is usually straightforward. Patients can contact their healthcare provider’s office directly or utilize online scheduling platforms. Flexibility in scheduling is important to accommodate patient availability. Scheduling considerations include the patient’s age, medical history, and any potential contraindications.
Administration Process Steps
| Step | Description |
|---|---|
| 1 | Patient Registration: Patient provides required information, including medical history and allergies. |
| 2 | Consultation: Healthcare provider reviews patient’s health status and discusses the vaccination schedule. |
| 3 | Site Preparation: Injection site is cleaned with an antiseptic solution. |
| 4 | Vaccination: Trained healthcare professional administers the vaccine injection. |
| 5 | Post-Injection Monitoring: Patient is monitored for any immediate reactions. |
| 6 | Follow-up Instructions: Healthcare provider provides instructions on potential side effects and follow-up care. |
Ending Remarks
In conclusion, the HPV vaccine schedule is designed to provide optimal protection against HPV, a common virus linked to various health issues. This guide has highlighted the importance of adhering to the recommended schedule, whether for routine vaccinations or catch-up doses. By understanding the factors influencing age-specific schedules, potential side effects, and additional considerations, individuals can make well-informed decisions about their health and well-being.
Remember, consulting a healthcare provider is always crucial for personalized advice.