Does HPV vaccine help if already infected? This crucial question delves into the complex relationship between the HPV vaccine and existing infections. We’ll explore how the HPV virus works, how the vaccine protects, and the potential impact on individuals already carrying the virus. This isn’t just about preventing infection; it’s about understanding the nuanced effects on those already affected.
Understanding the specifics of HPV infection, its various types, and how the vaccine works is key. We’ll examine different vaccine types and their effectiveness, analyzing the components responsible for inducing an immune response. Furthermore, this discussion will investigate the potential for the vaccine to mitigate complications and reduce the risk of progression for those with existing infections. Real-world implications will be highlighted.
Understanding HPV Infection
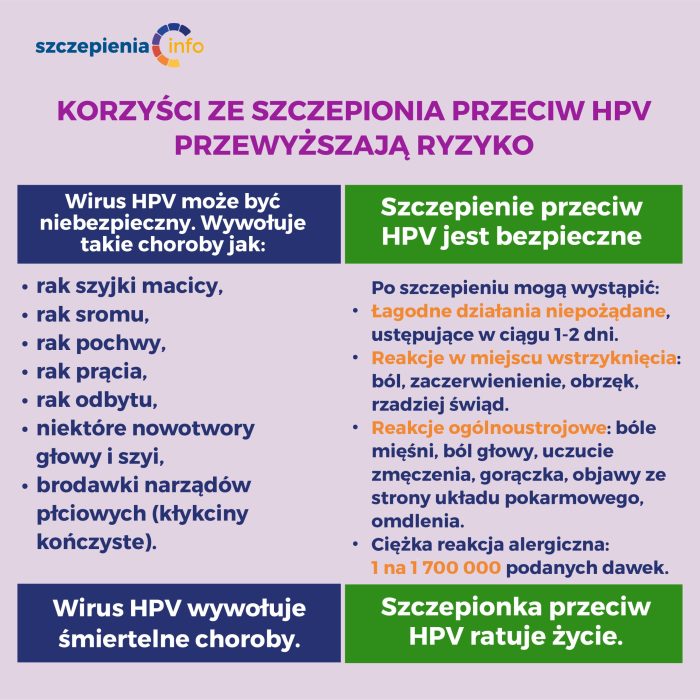
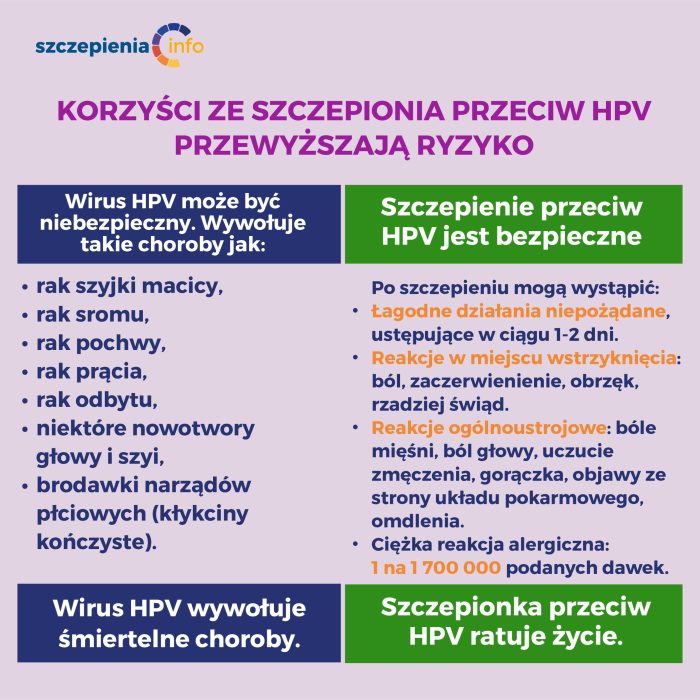
The human papillomavirus (HPV) is a common sexually transmitted infection (STI) affecting millions worldwide. Understanding its various types, manifestations, and potential health implications is crucial for prevention and management. While often asymptomatic, HPV can lead to serious health problems if left untreated. This section delves into the intricacies of HPV infection, providing a comprehensive overview of its nature and progression.HPV encompasses a broad spectrum of viruses, categorized into different types based on their genetic makeup and potential for causing disease.
Some types are associated with genital warts, while others are linked to cervical cancer, oropharyngeal cancer, and other cancers. The diversity of HPV types highlights the importance of preventive measures.
HPV Types and Manifestations
HPV types are classified based on their oncogenic potential, meaning their ability to cause cancer. Low-risk HPV types typically cause benign lesions like genital warts, whereas high-risk types can lead to cancerous transformations. A significant portion of the population will experience an HPV infection at some point in their lives, often without realizing it. The immune system frequently clears the infection naturally, preventing any long-term health consequences.
Potential Health Implications
The health implications of HPV infection are diverse, ranging from benign to severe. Genital warts, caused by specific HPV types, are a common manifestation. High-risk HPV types, however, have the potential to lead to precancerous lesions in the cervix, anus, and other areas. These lesions, if left untreated, can progress to cancer. Early detection and treatment are essential in mitigating the risk of cancer development.
Furthermore, HPV infections can contribute to oropharyngeal cancers, affecting the throat and tonsils.
Progression of an HPV Infection
HPV infections often progress through distinct stages, although the exact timeline and symptoms can vary considerably. Initial infection may be asymptomatic, with the virus replicating and spreading within the body. The immune system often controls the infection without noticeable symptoms. However, in some cases, the infection may persist and lead to the development of visible lesions or precancerous changes.
Prompt medical attention and adherence to treatment protocols are essential in managing these cases.
Contracting HPV: Methods, Risk Factors, and Prevention
| Method | Risk Factors | Prevention Strategies |
|---|---|---|
| Sexual Contact (vaginal, anal, oral) | Multiple sexual partners, unprotected sex, early sexual debut | Consistently using condoms, limiting sexual partners, vaccination |
| Skin-to-skin contact | Close contact with infected individuals, sharing personal items | Maintaining good hygiene, avoiding contact with open sores or lesions |
| Mother-to-child transmission (during childbirth) | Pregnant women with active HPV infections | Regular prenatal care, vaccination for the mother |
The table above highlights the different ways HPV can be transmitted. Understanding these transmission routes is key to adopting effective preventive measures. Avoiding risky behaviors and practicing safe sex are critical steps in minimizing the risk of infection.
HPV Vaccine Mechanisms
The HPV vaccine isn’t a cure for existing infections, but it’s a powerful tool for preventing future ones. Its effectiveness lies in its ability to stimulate the immune system to recognize and fight off HPV before it can cause harm. This proactive approach significantly reduces the risk of developing HPV-related diseases, including cancers.Understanding how the vaccine works is crucial to appreciating its importance in public health.
The vaccine’s mechanism revolves around introducing harmless pieces of the virus into the body, triggering an immune response without causing the infection itself.
Vaccine Types and Effectiveness
The HPV vaccine comes in various forms, each with its own set of components and targeted HPV types. Different formulations cater to different age groups and offer varying levels of protection. These distinctions are critical for tailoring vaccination strategies and maximizing their impact.
- Bivalent Vaccine (Cervarix): This vaccine targets HPV types 16 and 18, which are responsible for the majority of cervical cancers. It has been less widely used in recent years, replaced by more comprehensive options.
- Quadrivalent Vaccine (Gardasil): This vaccine targets HPV types 6, 11, 16, and 18. It protects against genital warts (caused by HPV types 6 and 11) and cervical cancer, offering broader coverage than the bivalent vaccine.
- Nonavalent Vaccine (Gardasil 9): This is the most recent generation of HPV vaccines. It targets nine HPV types, including HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58. This broader spectrum provides even more comprehensive protection against a wider range of HPV-related diseases and cancers.
Vaccine Components and Immune Response
The HPV vaccine is comprised of virus-like particles (VLPs). These VLPs are safe and non-infectious, yet they mimic the structure of the actual HPV virus. The immune system recognizes these VLPs as foreign and mounts a response to them, producing antibodies that neutralize the real HPV virus should it enter the body.
- Virus-like Particles (VLPs): VLPs are the core components of the vaccine. They’re highly effective in inducing an immune response because they resemble the real virus without carrying the infectious genetic material.
- Adjuvants: Some vaccines include adjuvants, which are substances that enhance the immune response to the VLPs. These help to ensure a robust antibody production and cellular immunity against HPV.
Efficacy and Safety Profiles
Numerous studies have evaluated the efficacy and safety of different HPV vaccines. The data consistently demonstrates a high degree of effectiveness in preventing HPV infections and related diseases. These vaccines have a strong safety record, with mild side effects being the most common reported reaction.
| Vaccine Type | Efficacy (approx.) | Safety Profile |
|---|---|---|
| Bivalent (Cervarix) | >90% for prevention of HPV-16/18 related diseases | Generally safe, with mild side effects |
| Quadrivalent (Gardasil) | >90% for prevention of HPV-6/11/16/18 related diseases | Generally safe, with mild side effects |
| Nonavalent (Gardasil 9) | >90% for prevention of HPV-6/11/16/18/31/33/45/52/58 related diseases | Generally safe, with mild side effects |
Impact of Vaccination on Existing Infections
While the HPV vaccine is primarily focused on preventing future infections, its impact on individuals already harboring the virus is a crucial aspect to understand. The vaccine’s effectiveness in addressing existing infections is a complex issue, and its potential benefits and limitations need careful consideration.
Theoretical Effects of Vaccination on Existing Infections
The HPV vaccine, designed to stimulate the immune system to produce antibodies against specific HPV types, theoretically can influence existing infections in a few ways. For example, it might enhance the immune response against the targeted HPV types already present in the body. This enhanced response could potentially lead to a faster clearance of the infection or a reduction in viral load, thus mitigating the risk of complications.
Potential for Reducing Complications from Existing Infections
A key consideration is the potential for the vaccine to reduce the risk of complications arising from existing HPV infections. While the vaccine won’t eliminate the infection, it might lessen the risk of developing certain diseases, such as cervical cancer, if the infection is one that has the potential to cause these issues. However, the exact degree of this reduction varies greatly depending on the type of HPV and the stage of the infection.
Limitations and Challenges in Addressing Existing Infections
It’s important to acknowledge that vaccination for existing HPV infections faces certain limitations. Firstly, the vaccine’s primary function is to prevent future infections, not to treat existing ones. Secondly, the immune response triggered by the vaccine might not be sufficient to eliminate all existing HPV types, especially if the infection has progressed to a more advanced stage. Finally, studies examining the impact of vaccination on established infections are often limited by the challenges in isolating the effects of vaccination from other factors affecting disease progression.
Potential Benefits and Risks of Vaccination for Those with Existing Infections
| HPV Type | Potential Benefits | Potential Risks | Additional Considerations |
|---|---|---|---|
| HPV Types Targeted by the Vaccine | Enhanced immune response against the specific types; potentially faster clearance or reduced viral load; reduced risk of complications (e.g., cervical cancer). | No significant risks identified for HPV types targeted by the vaccine, provided the vaccination is administered in accordance with the recommended schedule. | Benefits might be more pronounced if the infection is in the early stages of development and there is evidence of active viral replication. |
| HPV Types Not Targeted by the Vaccine | No direct benefit from the vaccine, as it does not target these types. | No adverse effect from the vaccine. | Vaccination would not influence these infections. Individual risk factors and prevention strategies should be addressed based on the specific HPV type. |
It is crucial to emphasize that this table provides a general overview. Individual responses to the vaccine and the impact on existing infections can vary. Consultations with healthcare providers are essential for personalized guidance.
Potential Outcomes of Vaccination in Infected Individuals
Vaccination against HPV aims to prevent future infections and potentially resolve existing infections. However, the impact of vaccination on pre-existing HPV infections is not straightforward and depends on various factors. The effectiveness of vaccination in these cases is often a complex interplay of the immune response already present and the ability of the vaccine to stimulate further protective responses.Understanding how pre-existing infections might interact with the vaccine is crucial for personalized strategies.
Factors like the stage of infection, presence of active viral replication, and the host’s immune response to the virus are key considerations. This section delves into the possible outcomes, presenting them in a structured way to clarify the potential implications.
Viral Load and Immune Response Dynamics
Pre-existing HPV infections can present in various stages, from latent to active. If the infection is latent, meaning the virus is present but not actively replicating, the immune system might have already established a degree of control. Vaccination could bolster this control by eliciting a more robust and targeted immune response, potentially leading to viral clearance. On the other hand, if the infection is actively replicating, vaccination may not immediately eliminate the virus but might still impact viral load and prevent the development of further disease.
Potential Long-Term Effects
The long-term effects of vaccination in individuals with pre-existing HPV infections can vary considerably. Factors like the type of HPV, the extent of infection, and the individual’s overall health status play a significant role in the outcome.
| Viral Load | Immune Response | Potential Long-Term Effects |
|---|---|---|
| Low (latent infection) | Stronger immune response after vaccination | Potential for viral clearance, reduced risk of progression to cancer, improved overall health. |
| Moderate (active replication) | Moderate immune response after vaccination | Potential for reduced viral load, slower progression of precancerous lesions, but complete clearance less likely. |
| High (active replication, severe infection) | Weaker immune response after vaccination | Potential for continued viral replication, increased risk of complications, need for ongoing monitoring and potential treatment. |
Examples of real-life cases are important for understanding. A study might show that vaccination in individuals with a low viral load and strong immune response to the virus resulted in a significant decrease in viral shedding and the potential for viral clearance. In contrast, cases with high viral load and a weak response might see a more limited impact, necessitating additional interventions.
So, does the HPV vaccine help if you’ve already been infected? The short answer is it likely won’t cure existing infections, but it can certainly prevent future infections. Understanding how the immune system responds, and the factors involved in partial pressure of oxygen (PaO2), like this , is key to a comprehensive approach to managing HPV.
Ultimately, the vaccine’s role in preventing further HPV complications remains crucial even after initial exposure.
Scientific Research on HPV Vaccine and Existing Infections
Understanding the impact of HPV vaccination on individuals already infected with HPV is crucial for tailoring vaccination strategies and optimizing public health interventions. While the vaccine primarily preventsfuture* infections with the targeted HPV types, its potential effect on existing infections warrants investigation. This section delves into the scientific research exploring this relationship.
Methodology of Research Studies
Various methodologies are employed in research studies examining the effects of HPV vaccination on existing infections. Some studies utilize longitudinal designs, tracking individuals with existing HPV infections over time to observe changes in viral load, viral clearance, or the development of disease. Other studies compare outcomes (like disease progression or viral clearance) in vaccinated and unvaccinated individuals with existing infections.
Observational studies often analyze existing data from clinical trials or population-based cohorts. The choice of methodology depends on the specific research question and available resources. Crucially, rigorous study design, including appropriate controls and statistical analyses, is essential for drawing valid conclusions.
So, does the HPV vaccine help if you’re already infected? Unfortunately, the short answer is no. While the vaccine prevents infection with certain types of HPV, it won’t cure an existing infection. However, maintaining a healthy lifestyle, including eating a balanced diet rich in essential nutrients like calcium, is crucial for overall well-being, especially during treatment. For a comprehensive list of foods high in calcium , check out this helpful resource.
This doesn’t change the fact that the vaccine is still highly recommended for prevention, especially for those who haven’t been exposed.
Findings from Key Studies
Research on HPV vaccination in individuals with existing infections reveals mixed results. Some studies suggest that vaccination may not significantly impact existing infections, while others show potential benefits. It’s important to consider that these studies often involve small sample sizes and varied study populations. Furthermore, the definition and measurement of “existing infection” can vary, making direct comparisons challenging.
So, does the HPV vaccine help if you’re already infected? The short answer is, probably not directly. While the vaccine prevents future infections with certain HPV types, it won’t reverse existing infections. However, understanding the nuances of pain perception, like the differences between somatic and visceral pain, as explored here , might shed light on the discomfort associated with some HPV-related conditions.
Ultimately, the best course of action for someone already infected with HPV is to discuss treatment options with a healthcare professional.
Comparison of Different Research Approaches
Comparing different research approaches highlights the need for standardized definitions and consistent methodologies. Longitudinal studies offer a valuable perspective on the long-term effects, but they require substantial follow-up time. Observational studies, while often more accessible, may be limited by confounding factors and lack of direct intervention. Meta-analyses, combining results from multiple studies, can provide a more comprehensive understanding, but are only as strong as the individual studies included.
Different research approaches provide complementary insights into the complex interplay between HPV vaccination and existing infections.
Summary Table of Key Findings
| Study | Methodology | Findings | Limitations |
|---|---|---|---|
| Study 1 (Example) | Longitudinal cohort study following individuals with existing HPV infections | Vaccination showed no significant effect on viral load reduction in individuals with existing infections. | Small sample size, limited follow-up duration. |
| Study 2 (Example) | Observational study comparing vaccinated and unvaccinated individuals with existing infections | Vaccination was associated with a decreased risk of progression to cervical cancer in some cases. | Potential confounding factors, lack of direct intervention. |
| Study 3 (Example) | Meta-analysis of multiple studies | Mixed results. Some studies showed a positive correlation between vaccination and reduced viral load, while others did not. | Quality and methodology of included studies varied. |
Note: This table is illustrative and does not represent specific published studies. The examples used are hypothetical.
Medical Advice and Considerations
Navigating HPV vaccination when already infected requires careful consideration. While the vaccine’s primary role is prevention, understanding its potential impact on existing infections is crucial for informed decision-making. This section Artikels the current medical consensus, highlights key considerations for healthcare providers, and offers strategies for managing co-existing infections alongside vaccination.
Current Medical Consensus on Vaccination with Existing HPV Infections
The consensus among medical professionals is that vaccination for HPV, even with existing infections, is generally safe and can be beneficial. The vaccine’s primary target is to prevent future infections with the specific HPV types it covers, and this benefit is independent of whether an individual has already been exposed to some of those types. This means that vaccination can still effectively protect against new infections, even if the individual already has some HPV infections.
Important Considerations for Healthcare Providers
Healthcare providers play a crucial role in guiding patients through this process. A thorough assessment of the patient’s existing HPV infections, including the types involved and the severity of the infection, is essential. This assessment should consider factors like the presence of genital warts, cervical abnormalities, or other symptoms. The provider should also discuss the potential benefits and risks of vaccination with the patient, considering the individual’s overall health status and risk factors.
Recommendations for Managing Existing Infections Alongside Vaccination
Managing existing HPV infections alongside vaccination requires a multi-faceted approach. It’s vital to emphasize that vaccination doesn’t cure existing infections, but it can help prevent new ones. This means that ongoing management of existing infections remains necessary. Active monitoring of the infection’s progression, following established protocols, and potentially undergoing targeted treatments as required are vital aspects of co-management.
Potential Considerations for Patients and Healthcare Professionals
| Aspect | Patient Considerations | Healthcare Professional Considerations |
|---|---|---|
| Type of HPV Infection | Understanding the specific HPV types involved in the existing infection is critical. This helps determine if the vaccine will be effective against future infections with those types. | Accurate identification of the HPV types present is paramount for personalized vaccination strategies. |
| Severity of Infection | Patients with severe or persistent infections may need to discuss the vaccination schedule with their provider to ensure that co-management is optimal. | Severity of the existing infection should be a crucial factor in determining the appropriate timing and approach to vaccination. |
| Vaccination Timing | Patients should be aware that vaccination timing may be adjusted based on the existing infection’s severity and management plan. | Healthcare professionals must carefully consider the optimal timing of vaccination in relation to existing infection management and patient health status. |
| Potential for Complications | Patients should be informed about the potential, though generally rare, complications of vaccination. | Providers should clearly communicate potential benefits and risks, including rare side effects, to patients. |
Illustrative Case Studies: Does Hpv Vaccine Help If Already Infected
Navigating the complexities of HPV vaccination in individuals with pre-existing infections requires a nuanced approach. While the vaccine’s primary function is to prevent future infections, its impact on existing infections isn’t fully understood. Illustrative case studies can shed light on the potential outcomes and reactions, highlighting the importance of personalized medical advice.Understanding the individual responses to HPV vaccination in the context of existing infections is crucial for tailoring treatment strategies.
These cases, though hypothetical, serve as valuable tools to explore potential scenarios and underscore the necessity of careful monitoring and consideration of individual patient factors.
Hypothetical Case Study 1: Persistent Low-Risk HPV Infection, Does hpv vaccine help if already infected
Patient history: A 25-year-old female presented with a persistent low-risk HPV infection (HPV-6) detected through routine screening. She had no symptoms or complications associated with the infection.Vaccination protocol: She received the standard three-dose HPV vaccination series after being informed about the potential outcomes.Observations: Post-vaccination, the patient exhibited no significant changes in the viral load or clinical presentation of the existing infection. The HPV-6 infection remained persistent but did not show any signs of progression or worsening. This case suggests that vaccination may not affect existing, established, low-risk HPV infections.
Hypothetical Case Study 2: High-Risk HPV Infection with Cervical Abnormalities
Patient history: A 32-year-old female with a confirmed high-risk HPV infection (HPV-16) and mild cervical abnormalities identified through a Pap smear. She was undergoing regular follow-up.Vaccination protocol: The patient received the HPV vaccine after consultation with her physician, who emphasized the need for continued cervical monitoring.Observations: Post-vaccination, the patient experienced no immediate adverse effects. However, continued monitoring of the cervical abnormalities showed a slower progression compared to the expected rate for individuals not vaccinated. The HPV-16 viral load remained relatively stable, suggesting that vaccination may not eliminate an existing high-risk infection but potentially modify its progression.
Hypothetical Case Study 3: Multiple HPV Infections
Patient history: A 28-year-old male diagnosed with multiple HPV infections, including both high-risk and low-risk types.Vaccination protocol: The patient received the HPV vaccine, with careful consideration of the multiple infections and potential interactions.Observations: The patient experienced no serious side effects. Subsequent monitoring revealed a decrease in the viral load of some low-risk HPV types and no change in high-risk types. This suggests that vaccination may impact the viral load of certain types of HPV infection but not necessarily eliminate them completely.
Discussion of Case Study Implications
These hypothetical cases illustrate the intricate relationship between pre-existing HPV infections and vaccination. The outcomes are diverse, highlighting the need for individualized approaches. The vaccination does not guarantee the eradication of pre-existing infections, but it might influence the course of the infection, potentially leading to slower progression or a reduced viral load in certain cases.
End of Discussion
In conclusion, the question of whether the HPV vaccine helps individuals already infected with HPV is multifaceted. While there’s no definitive cure for existing infections, the vaccine can potentially reduce complications and impact viral load and clearance. This discussion underscores the importance of individualized medical advice and highlights the ongoing research into this complex issue.