HIV mouth sores pictures offer a crucial visual aid for understanding the oral manifestations of HIV. Identifying these sores early is vital for proper diagnosis and treatment. This guide will visually illustrate various types of mouth sores associated with HIV, providing clear images and detailed descriptions. The goal is to empower patients and healthcare providers with a comprehensive understanding of these oral health issues.
From the initial symptoms to treatment options, this comprehensive resource will cover all aspects of HIV-related oral sores. Understanding the visual characteristics, potential causes, and appropriate management strategies is paramount for effective care. We’ll delve into the importance of oral hygiene, the role of antiretroviral therapy, and explore preventative measures. This guide aims to be a reliable source of information for those affected by HIV.
Overview of Oral Health Issues Related to HIV
HIV infection significantly impacts oral health. The weakened immune system allows opportunistic infections and diseases to thrive, often manifesting as oral lesions and sores. Maintaining good oral hygiene is crucial for HIV patients to prevent severe complications and maintain overall well-being. Early detection and prompt treatment of oral health problems are essential for managing the infection effectively.
Relationship Between HIV and Oral Health
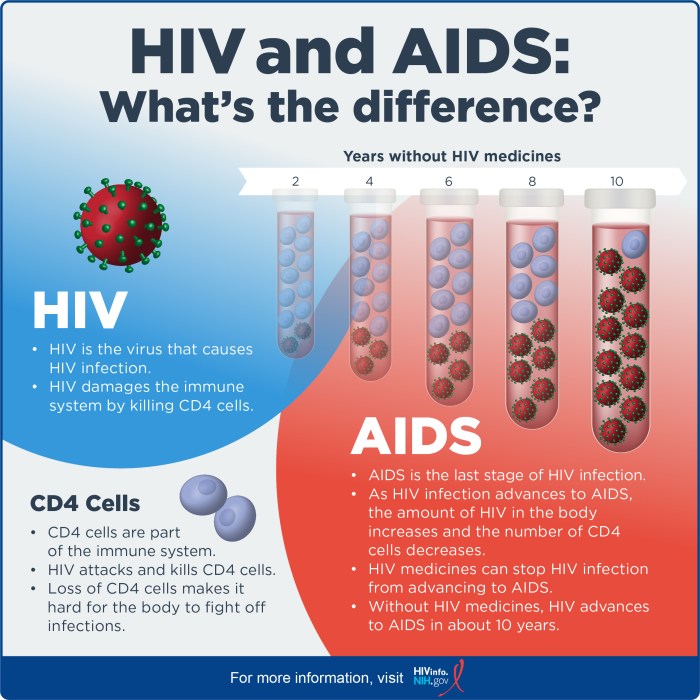
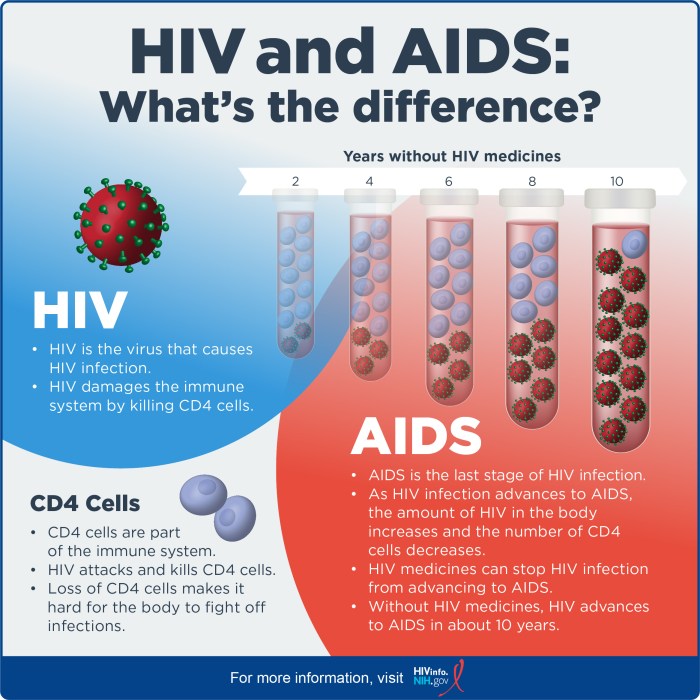
HIV weakens the immune system, making individuals more susceptible to oral infections. This compromised immune response allows various microorganisms to proliferate, leading to a higher incidence and severity of oral diseases. The viral load and CD4 cell count play a significant role in determining the susceptibility to oral health problems. Lower CD4 counts often correlate with increased risk and severity of oral manifestations.
Common Oral Manifestations of HIV Infection
Oral manifestations of HIV infection are diverse and can range from minor discomfort to serious complications. Common examples include oral thrush (candidiasis), hairy leukoplakia, linear gingival erythema, and oral herpes. These conditions can present as white patches, hairy growths, red lesions, or painful sores. The severity and frequency of these manifestations vary depending on the individual’s immune status and overall health.
Importance of Oral Health in HIV Patients
Maintaining good oral hygiene is critical for HIV patients. Regular dental check-ups and proper oral care practices help prevent and manage oral infections, reducing pain, discomfort, and potential complications. Prompt treatment of oral issues is essential for preventing further deterioration of oral health and maintaining overall well-being. Early intervention can often improve the quality of life and overall health outcomes.
Comparison of Oral Sores in General Populations and HIV Patients
| Characteristic | General Population | HIV Patients |
|---|---|---|
| Cause | Various factors, including poor oral hygiene, trauma, or underlying medical conditions. | Weakened immune system allowing opportunistic infections, particularly fungal infections (like Candida albicans). |
| Common Symptoms | Pain, swelling, redness, ulcers. Symptoms may vary depending on the cause. | Similar to general population, but often more frequent, severe, and persistent due to the immune deficiency. Symptoms can be indicative of other opportunistic infections. |
| Frequency | Generally less frequent. | Significantly higher frequency and severity. |
| Treatment | Treatment depends on the cause, ranging from topical antiseptics to antibiotics. | Often requires longer-term treatment with antifungal medications or antiviral therapies. |
| Potential Complications | Potential complications vary depending on the cause. | Higher risk of severe complications due to weakened immune system and opportunistic infections. |
Types of Mouth Sores Associated with HIV
Oral health issues are a significant concern for individuals living with HIV. These issues can range from minor discomfort to serious complications, impacting overall well-being and quality of life. Understanding the different types of mouth sores associated with HIV is crucial for early detection, appropriate management, and improved patient outcomes. This deeper look will help you recognize these potential problems.Oral manifestations of HIV, frequently referred to as oral opportunistic infections, can stem from a weakened immune system, making individuals susceptible to various types of mouth sores.
These sores can manifest in various ways, impacting not just the appearance but also the comfort and overall health of the affected individual.
Types of Oral Ulcers
Oral ulcers, often painful and unsightly, are a common manifestation of various conditions, and HIV is no exception. These lesions, or ulcers, can range from small, shallow sores to larger, deeper ulcers. Their appearance, location, and potential complications can vary significantly depending on the underlying cause. Proper identification and management are key to improving the well-being of those affected.
Candidiasis (Oral Thrush), Hiv mouth sores pictures
Candidiasis, commonly known as oral thrush, is a fungal infection caused by the overgrowth of Candida albicans. It frequently affects individuals with weakened immune systems, including those living with HIV. Characterized by white, cheesy patches on the tongue, inner cheeks, and palate, it can cause discomfort and difficulty eating. The presence of oral thrush can be a sign of a compromised immune response.
Herpes Simplex Virus (HSV) Infections
Herpes simplex virus (HSV) infections, including oral herpes, can lead to painful cold sores or fever blisters. These recurrent sores typically appear as small, fluid-filled blisters that rupture, forming painful ulcers. Location is often on the lips, but they can also appear on the inside of the mouth. Individuals with HIV may experience more frequent or severe outbreaks due to their weakened immune systems.
Linear Gingival Erythema (LGE)
Linear gingival erythema (LGE) is characterized by a red, smooth, and shiny appearance of the gums, typically along the gum margins. This condition is often accompanied by swelling and bleeding. LGE can be a sign of a compromised immune system and may be more prominent in those with HIV. It often appears in conjunction with other oral manifestations, making proper diagnosis crucial.
Kaposi’s Sarcoma (KS)
Kaposi’s sarcoma (KS) is a cancer that can develop in the lining of the mouth and other parts of the body. It typically presents as purplish or reddish-brown lesions, which can be flat or raised. KS is a significant opportunistic infection in individuals with advanced HIV. It can appear in different areas of the mouth, and prompt diagnosis is essential.
Table of Oral Sores Associated with HIV
| Sore Type | Appearance | Location | Potential Causes | Treatment Considerations |
|---|---|---|---|---|
| Candidiasis (Oral Thrush) | White, cheesy patches | Tongue, inner cheeks, palate | Overgrowth of Candida albicans, weakened immune system | Anti-fungal medications |
| Herpes Simplex Virus (HSV) | Small, fluid-filled blisters that rupture to form ulcers | Lips, inside of mouth | Herpes simplex virus, weakened immune system | Antiviral medications, managing outbreaks |
| Linear Gingival Erythema (LGE) | Red, smooth, shiny gums | Gum margins | Weakened immune system, potential opportunistic infections | Managing underlying HIV infection, supportive care |
| Kaposi’s Sarcoma (KS) | Purplish or reddish-brown lesions, flat or raised | Mouth lining and other areas | Opportunistic infection in advanced HIV | Anti-cancer medications, addressing underlying HIV |
Symptoms and Diagnosis of HIV-Related Mouth Sores
Identifying and treating HIV-related oral lesions is crucial for overall health management. Early detection allows for prompt intervention, potentially preventing complications and improving the patient’s quality of life. This section delves into the specific symptoms and diagnostic processes employed for various oral manifestations linked to HIV.Understanding the diverse symptoms and diagnostic approaches is vital for healthcare professionals to provide effective care and support to patients.
Accurate identification of the specific oral condition enables tailored treatment strategies, ultimately promoting oral health and overall well-being.
Typical Symptoms of HIV-Related Mouth Sores
Recognizing the range of symptoms associated with HIV-related mouth sores is essential for early diagnosis and appropriate intervention. These symptoms can vary in presentation and severity depending on the underlying condition and the individual’s immune status. Symptoms may include painful ulcers, white patches, redness, and swelling, potentially affecting any area of the oral cavity.
- Ulcers: Painful sores, often characterized by a shallow crater-like appearance, can range in size from small to larger, depending on the type of infection. These ulcers can be accompanied by discomfort during eating and speaking.
- White Patches: Leukoplakia, a precancerous condition, often presents as thick, white patches within the mouth. These patches may appear on the gums, tongue, or inner cheeks. Careful observation and further evaluation are crucial.
- Redness and Swelling: Inflammation and redness in the oral tissues may indicate an infection or other underlying condition. Swelling, particularly around the gums or palate, could signify an inflammatory process. Such symptoms require immediate medical attention.
Diagnostic Procedures for Identifying Mouth Sores
Precise identification of oral sores associated with HIV is crucial for effective management. This section details the diagnostic procedures used to determine the cause and severity of the condition.
- Medical History Evaluation: Gathering a comprehensive medical history, including details about the patient’s HIV status, current medications, and any recent illnesses, is fundamental. This information provides crucial context for interpreting the oral findings.
- Physical Examination: A thorough visual examination of the oral cavity, including the tongue, gums, palate, and inner cheeks, is necessary. Careful inspection for size, shape, color, and location of lesions is vital. Palpation, or gentle touch, can help identify any underlying tenderness or swelling.
Diagnostic Tools for Various Mouth Sore Types
The choice of diagnostic tool depends on the specific type of mouth sore suspected. This table Artikels various diagnostic methods for different conditions.
| Mouth Sore Type | Diagnostic Tools |
|---|---|
| Ulcers (e.g., herpes simplex virus, aphthous ulcers) | Visual examination, possibly a scraping of the ulcer base for microscopic examination, or testing for viral markers (e.g., herpes simplex virus). |
| White Patches (e.g., leukoplakia, candidiasis) | Visual examination, scraping for microscopic examination (cytology), potassium hydroxide (KOH) preparation to look for fungal elements, and potentially a biopsy for more definitive diagnosis. |
| Redness and Swelling (e.g., gingivitis, oral thrush) | Visual examination, probing of gums for inflammation and bleeding, and possibly cultures to identify the causative agent. |
Visual Representation of HIV-Related Mouth Sores
Understanding the visual presentation of oral lesions associated with HIV is crucial for early diagnosis and effective management. Accurate identification of these sores, often the first noticeable symptoms, allows for prompt medical intervention and potentially prevents further complications. Visual aids play a significant role in this process, providing both clinicians and patients with a clearer picture of the condition.
Finding pictures of HIV mouth sores can be helpful for self-assessment, but it’s crucial to remember that visual aids can’t replace professional medical advice. If you’re experiencing these issues, it’s important to consult a doctor. Similarly, understanding the proper use of assistive devices like a cane for multiple sclerosis, is essential for maintaining mobility and safety.
Fortunately, resources like this guide on cane for multiple sclerosis can offer valuable insights. Ultimately, seeking professional medical attention for potential HIV-related mouth sores is paramount.
Visual Characteristics of Different Types of Mouth Sores
Visual representations, such as photographs and illustrations, are invaluable tools for recognizing various types of oral sores linked to HIV. These visual aids can showcase the diverse appearances, locations, and stages of these lesions. Accurate depictions, emphasizing color and texture, are essential for aiding in the diagnosis process.
Illustrations of Common HIV-Related Mouth Sores
Precise visual representations of oral sores associated with HIV are critical for both clinicians and patients. Illustrations can depict the nuanced variations in appearance, aiding in distinguishing between different types of oral lesions. These visual aids should demonstrate the range of colors, from red and white to grayish-yellow or brown, and the textures, from smooth and flat to bumpy or ulcerated.
- Candidiasis (Oral Thrush): Illustrations should show the characteristic white or yellowish patches on the tongue, inner cheeks, and palate. The patches may appear thick and slightly raised, sometimes resembling cottage cheese. Illustrations should also demonstrate how these patches can vary in size and distribution across the oral cavity. These images would be beneficial to aid patients in recognizing this common HIV-related oral infection.
- Herpes Simplex Virus (HSV) Infections: Illustrations should depict the varying stages of HSV oral lesions. Early-stage lesions may show small, fluid-filled blisters, often clustered together. Later stages could show open sores or ulcers with a yellowish or grayish base. Illustrations should illustrate the location of these sores, including the lips, tongue, and inner cheeks.
- Linear Gingival Erythema: Illustrations should show a bright red, smooth, and slightly swollen appearance along the gum line. The redness may be diffuse or concentrated in specific areas. These illustrations should emphasize the consistent redness and smooth texture, distinguishing it from other oral conditions.
- Kaposi’s Sarcoma (KS): Illustrations should showcase the characteristic lesions, which can appear as reddish-purple, dark-red, or brown macules or plaques. These lesions can vary in size and shape, and illustrations should demonstrate their potential to be flat, raised, or nodular. Illustrations should show the possible locations, including the palate, gums, and tongue. They should also demonstrate the progression of the lesions, from early to advanced stages.
Significance of Visual Representation in Diagnosis
Accurate visual representation is crucial in aiding diagnosis. Clinicians can use illustrations and photographs to compare observed lesions with known patterns associated with specific oral conditions. This comparison process facilitates a quicker and more accurate diagnosis, enabling appropriate treatment strategies. Patients can also benefit from visual aids, enabling them to better understand their condition and participate actively in their care.
Ever wondered about HIV mouth sores pictures? Finding reliable information online can be tricky. Fortunately, if you’re looking for details on medications like Librax, checking out the librax frequently asked questions page can be helpful. While those questions aren’t directly about HIV mouth sores, understanding potential side effects and interactions is crucial for overall health.
Ultimately, though, consulting a medical professional for any health concerns, including pictures of HIV mouth sores, is essential.
Importance of Accurate Depiction of Mouth Sores
Precise illustrations are essential for accurate diagnosis and patient education. Visual aids must accurately represent the color and texture of the sores. Variations in shade and texture can be subtle but significant in differentiating between different conditions. Inaccurate depictions can lead to misdiagnosis or delayed treatment, hindering the patient’s well-being. For example, a depiction of oral thrush that is not correctly colored or textured might lead to it being misidentified as another oral condition.
Treatment and Management of HIV-Related Mouth Sores
Treating mouth sores associated with HIV involves a multifaceted approach, focusing on addressing the underlying infection and promoting oral health. Effective management requires a collaborative effort between the patient, healthcare provider, and dental team. This approach aims to alleviate symptoms, prevent complications, and improve the overall quality of life for individuals living with HIV.Managing oral health in HIV is crucial, not only for symptom relief but also for preventing further complications and maintaining overall well-being.
Finding pictures of HIV mouth sores can be really unsettling, but it’s important to remember that various conditions can cause similar symptoms. Understanding how to test for Hashimoto’s disease, an autoimmune condition that can sometimes present with oral issues, is crucial for accurate diagnosis. How to test for Hashimoto’s disease is a good place to start researching different symptoms and potential causes.
Ultimately, seeking professional medical advice is key when dealing with any unusual oral symptoms, especially if they persist.
Prompt and appropriate treatment can significantly reduce the risk of infection and promote healing. The goal is to create a supportive environment for the body’s natural healing processes.
Treatment Options for Various Types of Mouth Sores
Different types of oral sores associated with HIV necessitate tailored treatment strategies. The choice of treatment depends on the specific type of sore, its severity, and the individual’s overall health. Some sores may respond well to topical medications, while others may require systemic treatment.
Importance of Oral Hygiene in Managing Mouth Sores
Maintaining meticulous oral hygiene is fundamental in managing HIV-related mouth sores. Regular brushing, flossing, and rinsing with an antimicrobial mouthwash are crucial for preventing secondary infections and promoting healing. Proper oral hygiene helps to remove food particles and bacteria, minimizing the risk of further irritation and inflammation. Furthermore, maintaining a healthy oral environment supports the body’s immune response, facilitating the healing process.
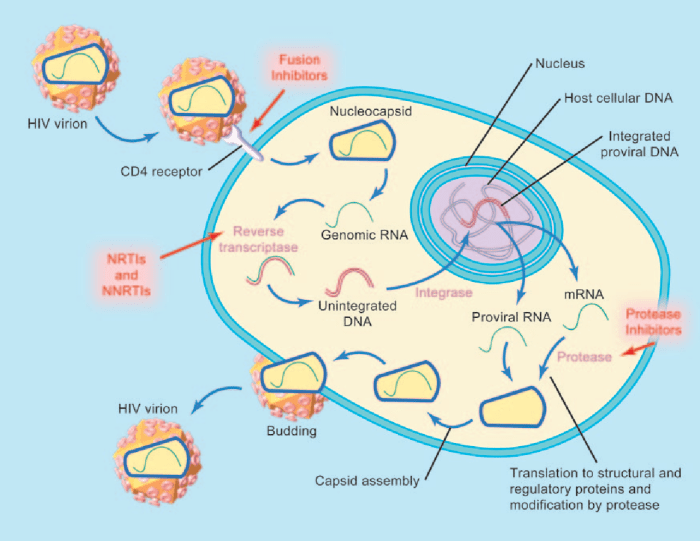
Role of Antiretroviral Therapy (ART) in Preventing and Managing Mouth Sores
Antiretroviral therapy (ART) plays a pivotal role in preventing and managing HIV-related mouth sores. By suppressing the virus, ART helps to bolster the immune system, making the body more resilient to opportunistic infections. As the immune system strengthens, the body’s ability to fight off infections that cause oral sores is enhanced. Consistent adherence to ART regimens is critical for achieving and maintaining viral suppression.
Table of Treatments and Effectiveness
| Treatment | Effectiveness | Medication Name (and Dosage, if applicable) | Potential Side Effects |
|---|---|---|---|
| Topical antifungals (e.g., clotrimazole) | Effective for candidiasis (thrush). | Clotrimazole troches (10mg) 5 times a day | Possible local irritation. |
| Antiviral medications (e.g., acyclovir) | Effective for herpes simplex virus (HSV) infections. | Acyclovir 400mg orally 5 times a day. | Possible gastrointestinal upset, headache. |
| Antibiotics (e.g., metronidazole) | Effective for bacterial infections. | Metronidazole 500mg orally twice a day. | Possible nausea, diarrhea, metallic taste. |
| Oral corticosteroids (e.g., prednisone) | Potentially effective for severe cases or inflammation. | Prednisone 20-40mg orally, gradually tapered. | Potential for increased risk of opportunistic infections, bone loss, diabetes exacerbation. Use with caution and only under the direction of a physician. |
Note: Dosage and treatment regimens should always be determined and supervised by a qualified healthcare professional. This table provides a general overview and is not exhaustive.
Prevention and Risk Factors for HIV-Related Mouth Sores: Hiv Mouth Sores Pictures

Protecting oral health is crucial for individuals living with HIV, as mouth sores can be a significant symptom and complication. Preventing these sores often involves a multi-faceted approach focusing on overall health, immune system support, and proactive oral hygiene. Understanding the risk factors associated with these sores allows for personalized strategies to minimize their occurrence.Maintaining a robust immune system is a cornerstone of preventing HIV-related oral complications.
A strong immune response helps fight off opportunistic infections that can manifest as mouth sores. This is achieved through adherence to antiretroviral therapy (ART), a healthy diet rich in essential nutrients, and regular exercise.
Preventive Measures
Proactive oral hygiene plays a vital role in reducing the risk of oral sores. Regular brushing and flossing, along with using antimicrobial mouthwash, are essential for maintaining a healthy oral environment. This helps prevent the buildup of bacteria and fungi, which can contribute to the development of sores. Furthermore, avoiding smoking and excessive alcohol consumption can significantly reduce the risk of oral issues.
Prompt dental checkups are also important to identify and address any potential oral health problems early.
Risk Factors
Several factors increase the likelihood of developing HIV-related mouth sores. These factors are often interconnected, emphasizing the importance of a holistic approach to health management.
- Low CD4+ T-cell counts: A reduced number of CD4+ T-cells, a key component of the immune system, weakens the body’s ability to fight infections, increasing the susceptibility to oral sores. Individuals with lower CD4+ counts often experience more frequent and severe sores.
- Poorly Controlled HIV: Inadequate management of HIV infection through ART can lead to a compromised immune system, increasing the risk of opportunistic infections that can manifest as mouth sores. Consistent and correct adherence to prescribed medications is vital for effective HIV management.
- Nutritional Deficiencies: A diet lacking essential vitamins and minerals can weaken the immune system and contribute to oral sores. A balanced diet rich in fruits, vegetables, and protein is crucial for overall health and oral well-being.
- Smoking and Alcohol Consumption: Smoking and excessive alcohol use can irritate the oral tissues, making them more susceptible to sores. These habits can also weaken the immune system, further increasing the risk of infections.
Comparison of Risk Factors for Different Types of Mouth Sores
| Type of Mouth Sore | Risk Factors |
|---|---|
| Oral Candidiasis (Thrush) | Low CD4+ counts, poor HIV control, use of certain medications, poor oral hygiene |
| Herpes Simplex Virus (HSV) Infections | Weakened immune system, exposure to the virus, stress, poor oral hygiene |
| Oral Hairy Leukoplakia | Low CD4+ counts, advanced HIV infection, and Epstein-Barr Virus infection. |
| Aphthous Ulcers (Canker Sores) | Genetic predisposition, stress, nutritional deficiencies, and certain medications |
Resources and Support for Patients with HIV-Related Mouth Sores
Navigating the challenges of HIV-related mouth sores can be daunting. Fortunately, a network of support and resources is available to help patients manage these issues effectively. Understanding these resources can significantly improve the quality of life for individuals living with HIV.
Support Groups and Online Communities
Support groups provide a crucial platform for sharing experiences, exchanging information, and offering mutual encouragement. These groups can offer a sense of community and belonging, helping individuals feel less isolated and more empowered to manage their health. Online forums and communities can also serve as valuable resources, connecting individuals with others facing similar challenges. They offer a readily accessible source of support, advice, and practical tips, especially in addressing the complexities of managing oral health issues.
Professional Medical Advice: The Importance of Seeking Help
Seeking professional medical advice is paramount in addressing HIV-related mouth sores. A healthcare provider can accurately diagnose the cause of the sores, rule out other potential conditions, and recommend the most appropriate treatment plan. This personalized approach is essential for effective management and ensures the patient receives the best possible care. Delaying medical attention can lead to complications and potentially worsen the condition.
Role of Dental Professionals in HIV Care
Dental professionals play a vital role in the comprehensive care of HIV patients. Dental exams and cleanings are crucial for maintaining oral health, even more so for individuals with HIV. Dental professionals are uniquely positioned to identify oral health issues early, potentially preventing more serious complications. They can also educate patients on proper oral hygiene practices, tailored to the specific needs of individuals living with HIV.
Regular dental checkups can help prevent the progression of oral health problems.
Support Organizations and Contact Information
Accessing resources from support organizations can be invaluable for patients dealing with HIV-related mouth sores. These organizations offer a range of services, including education, advocacy, and emotional support. They can provide critical information on managing the condition, connect patients with healthcare providers, and assist with navigating the complexities of the healthcare system. This table Artikels some key organizations that provide valuable resources for HIV-related oral health issues.
| Organization | Contact Information | Key Services |
|---|---|---|
| The AIDS Foundation of Chicago | (312) 663-9980 | Comprehensive HIV/AIDS services, including support groups, case management, and educational resources. |
| The National Association of People with AIDS (NAPWA) | (212) 807-6600 | Advocacy, support groups, and educational resources for people living with HIV/AIDS. |
| The Ryan White HIV/AIDS Program | Contact your local health department | Provides medical care, support services, and case management to people with HIV/AIDS. |
| The American Dental Association (ADA) | (312) 440-2500 | Provides information on oral health care and resources for dental professionals. |
Closing Summary

In conclusion, recognizing the visual presentation of HIV-related mouth sores is crucial for early diagnosis and effective treatment. This resource provides a comprehensive overview of the various types of sores, their characteristics, and management strategies. Remember, prompt medical attention is key to preventing complications and maintaining overall well-being. This guide is intended to serve as a valuable resource for both patients and healthcare professionals.