Is blood pressure higher in the morning? Yes, it often is, and understanding why this happens is crucial for managing your overall health. Our bodies have a natural rhythm, or circadian rhythm, that influences many functions, including blood pressure. This morning peak in blood pressure isn’t necessarily a cause for alarm, but knowing the factors behind it can help you take proactive steps toward a healthier lifestyle.
This post delves into the science behind morning blood pressure fluctuations, exploring the factors that contribute to these changes and how to manage them.
We’ll explore the normal diurnal variation of blood pressure, examining the role of stress hormones, sleep quality, medications, and lifestyle choices. Understanding these elements is key to comprehending the potential implications of high morning blood pressure and the strategies to effectively manage it.
Introduction to Morning Blood Pressure

Blood pressure, the force exerted by blood against the walls of blood vessels, isn’t constant throughout the day. It naturally fluctuates, exhibiting a predictable diurnal variation. Understanding these fluctuations is crucial for assessing overall cardiovascular health and identifying potential risks. This pattern is influenced by our internal biological clock, the circadian rhythm, which dictates many bodily functions.
Morning blood pressure spikes are a common thing, but did you know that boosting your metabolism might play a role? Some people find that incorporating healthy lifestyle choices, including a balanced diet and regular exercise, can help manage this. Exploring supplements to boost metabolism, like those found on this site , might offer another avenue for improved overall health, and potentially influencing blood pressure levels throughout the day.
Of course, it’s crucial to consult a doctor before making any significant dietary or supplement changes, especially if you have underlying health conditions. Understanding the underlying factors is key to managing morning blood pressure effectively.
Morning blood pressure often presents a peak, which warrants careful consideration. This section will explore the reasons behind this morning surge and highlight its significance.The circadian rhythm, an internal biological clock, governs numerous physiological processes, including blood pressure. This rhythm is deeply intertwined with our sleep-wake cycle and is largely influenced by environmental cues, particularly light. As we transition from sleep to wakefulness, a cascade of hormonal and neurological changes occurs, which often results in a rise in blood pressure.
This natural rise is a normal physiological response, but understanding its extent and potential implications is important.
Diurnal Variation in Blood Pressure
Blood pressure typically follows a predictable pattern throughout the day. It tends to be lower during sleep and rises gradually as we awaken and become more active. This morning surge in blood pressure is a common phenomenon, and its magnitude can vary from person to person. The precise mechanisms behind this variation are complex, involving intricate interactions between the nervous system, hormones, and the body’s overall physiological state.
Morning Blood Pressure Peak
The morning blood pressure peak is often observed in the period immediately following awakening. This is generally due to a combination of factors, including the body’s shift from the relaxed state of sleep to increased activity, along with hormonal changes. Understanding the factors contributing to this peak allows for more informed strategies for managing blood pressure, especially for individuals prone to hypertension or cardiovascular issues.
Physiological Processes and Blood Pressure Fluctuations
| Time of Day | Typical Blood Pressure Range (mmHg) | Explanation of Underlying Physiological Processes |
|---|---|---|
| Early Morning (immediately after waking) | Higher than other times of the day | Shift from rest to activity, hormonal changes (e.g., cortisol release), increased sympathetic nervous system activity. |
| Mid-morning to Afternoon | Gradually decreases | Metabolic activity and blood flow adjustments in response to ongoing physical and mental activity. |
| Evening | Lower than other times of the day | Relaxation and preparation for sleep, decreased sympathetic nervous system activity, and possible influence of evening meal. |
| Night | Lowest point | Deep sleep, lowest metabolic activity, lowest sympathetic nervous system activity. |
This table highlights the typical blood pressure trends throughout the day. Each time of day experiences distinct physiological changes that affect the circulatory system and thus influence blood pressure levels.
Factors Affecting Morning Blood Pressure
Morning blood pressure often sees a surge, a phenomenon that can be attributed to a complex interplay of physiological and lifestyle factors. Understanding these factors is crucial for individuals seeking to manage their blood pressure effectively and potentially prevent associated health risks. This elevated pressure in the morning is often temporary and resolves throughout the day, but it’s vital to understand the underlying reasons for its occurrence.
Stress Hormones and Morning Blood Pressure
The body’s natural response to waking involves a surge in stress hormones, primarily cortisol. This hormone plays a critical role in regulating various bodily functions, including blood pressure. As the body prepares for the day, cortisol levels increase, contributing to a temporary rise in blood pressure. The magnitude of this response varies significantly from person to person, depending on individual factors such as stress levels and overall health.
High chronic stress can further exacerbate this effect, leading to sustained elevations in morning blood pressure. Chronic stress also weakens the body’s ability to regulate blood pressure effectively.
Sleep Quality and Duration
Adequate sleep is essential for maintaining healthy blood pressure levels. Poor sleep quality and insufficient duration disrupt the body’s natural rhythm, potentially leading to increased morning blood pressure. When sleep is compromised, the body may not have adequate time to repair and restore itself, contributing to higher blood pressure readings. Individuals experiencing sleep apnea, for example, frequently show higher morning blood pressure, as the interrupted breathing patterns affect cardiovascular health.
Studies consistently demonstrate a strong correlation between insufficient sleep and elevated blood pressure readings.
Medications and Medical Conditions
Certain medications, such as decongestants, some anti-depressants, and even some over-the-counter cold remedies, can impact blood pressure. These medications can sometimes lead to elevated blood pressure, especially upon waking. Moreover, underlying medical conditions like kidney disease, thyroid disorders, or certain types of sleep disorders can also affect morning blood pressure readings. For example, individuals with untreated sleep apnea often experience significant fluctuations in blood pressure, with elevated readings frequently observed in the morning.
Proper medical management of these conditions is critical for maintaining healthy blood pressure throughout the day.
Morning blood pressure spikes are a common thing, but did you know that certain medical conditions can also affect blood pressure? For example, if someone is experiencing a seizure, understanding first aid for epilepsy and seizures here is crucial, as this can sometimes cause temporary changes in blood pressure readings. Knowing how to respond to such situations, and remembering that blood pressure can fluctuate throughout the day, is vital for your health and well-being.
Lifestyle Factors
Dietary habits, exercise routines, and overall lifestyle choices can influence morning blood pressure. A diet high in sodium, for instance, can lead to fluid retention, potentially contributing to elevated blood pressure readings. Lack of regular physical activity can also impact cardiovascular health, contributing to increased morning blood pressure. On the other hand, a balanced diet, regular exercise, and stress management techniques are beneficial in maintaining healthy blood pressure levels.
For example, studies show that incorporating regular physical activity, like brisk walking, into daily routines can help regulate blood pressure and improve sleep quality.
Table: Factors Affecting Morning Blood Pressure, Is blood pressure higher in the morning
| Factor | Potential Impact on Morning Blood Pressure | Supporting Evidence |
|---|---|---|
| Stress Hormones (e.g., cortisol) | Increased levels contribute to temporary elevation. | Studies showing correlation between cortisol levels and morning blood pressure. |
| Sleep Quality/Duration | Poor sleep quality and insufficient duration can lead to higher readings. | Numerous studies linking sleep deprivation and hypertension. |
| Medications | Certain medications can elevate blood pressure, especially in the morning. | Patient reports and clinical trials on medication side effects. |
| Medical Conditions | Underlying conditions can impact morning blood pressure. | Medical literature detailing the relationship between specific conditions and hypertension. |
| Lifestyle Factors (Diet, Exercise) | Unhealthy habits can exacerbate morning blood pressure issues. | Research on the effects of diet and exercise on cardiovascular health. |
Measurement and Monitoring of Morning Blood Pressure: Is Blood Pressure Higher In The Morning
Morning blood pressure readings are crucial for understanding individual cardiovascular health and potential risks. Accurate measurement techniques are essential to obtain reliable data, allowing for effective monitoring and management of blood pressure fluctuations, particularly the often-elevated readings observed in the morning. This section will delve into the importance of accurate measurement, the best methods, optimal timing, and strategies for consistent monitoring.Understanding the nuances of morning blood pressure measurement is vital for obtaining reliable data.
Consistent and accurate measurements form the foundation for effective treatment and prevention strategies related to cardiovascular health.
Importance of Accurate Measurement Techniques
Accurate measurement of morning blood pressure is paramount for assessing individual cardiovascular health. Inaccuracies can lead to misdiagnosis, inappropriate treatment, and potentially harmful consequences. Proper technique ensures reliable data, allowing for informed decisions about medication adjustments or lifestyle modifications. A consistent measurement protocol is crucial for identifying trends and patterns, enabling proactive interventions to manage blood pressure effectively.
Appropriate Methods for Taking Blood Pressure Readings
Several factors influence blood pressure readings, including the time of day, posture, and emotional state. Proper technique minimizes these influences, ensuring accurate results. Using a validated blood pressure monitor is essential. The cuff should be placed snugly, but not excessively tight, around the upper arm. The patient should be seated comfortably with their arm supported at heart level.
Avoiding talking or moving during the measurement is crucial for obtaining a precise reading. Repeating the measurement multiple times and averaging the results helps to reduce the impact of random fluctuations.
Ideal Time to Measure Morning Blood Pressure
The ideal time for measuring morning blood pressure is typically after a period of rest, such as upon waking up. This usually means first thing in the morning before any activity, consumption of food, or beverages, and also before getting out of bed. Ideally, readings should be taken at the same time each day to allow for the tracking of trends and patterns over time.
This consistency aids in identifying potential fluctuations and allows for the monitoring of individual responses to treatments or lifestyle changes.
Guidelines for Consistent Blood Pressure Monitoring
Maintaining consistent blood pressure monitoring habits is vital for tracking trends and identifying patterns. This includes establishing a regular schedule for measurements, using the same device each time, and noting any factors that might influence the readings, such as stress or caffeine intake. Keeping a detailed log of readings, along with corresponding lifestyle factors, is highly recommended. This information provides valuable context for interpreting the results and allows for better communication with healthcare providers.
Steps Involved in Correctly Measuring Morning Blood Pressure
- Prepare the blood pressure monitor and ensure the cuff is appropriate for the patient’s arm size.
- Have the patient sit comfortably in a chair with their feet flat on the floor and their arm supported at heart level.
- Position the cuff snugly but not excessively tight around the upper arm.
- Ensure the patient remains still and avoids talking or moving during the measurement process.
- Take multiple readings and average the results to reduce variability.
- Record the date, time, and readings in a log.
- Note any factors that might have influenced the reading, such as stress or caffeine intake.
Different Blood Pressure Measurement Devices
Choosing the right blood pressure measurement device is crucial for accurate results. Different devices offer varying levels of accuracy and ease of use.
| Device Type | Accuracy | Ease of Use |
|---|---|---|
| Electronic Upper Arm Devices | Generally high accuracy | High |
| Manual Devices (Sphygmomanometer and Stethoscope) | Accuracy depends on user expertise | Moderate |
| Wrist Devices | Moderate accuracy | High |
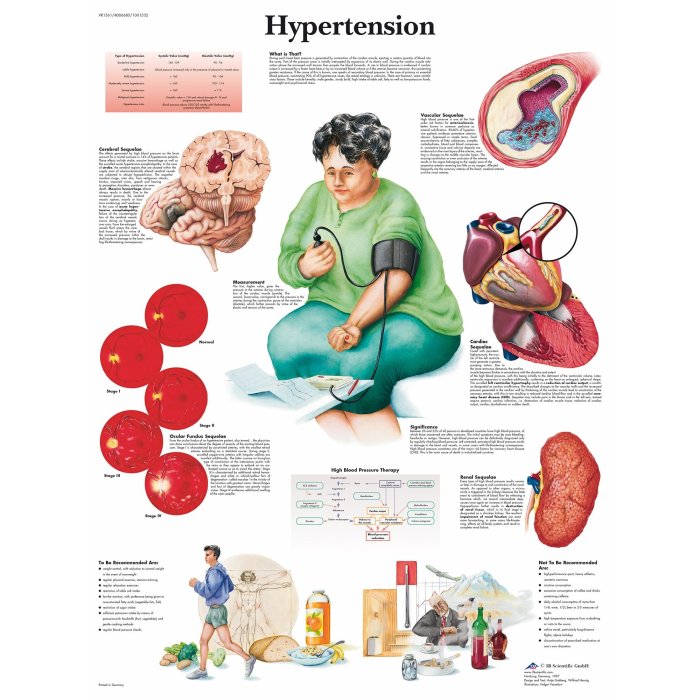
Implications of High Morning Blood Pressure
High morning blood pressure, while seemingly a minor issue, can have significant long-term health consequences. Understanding the implications of this consistent elevation in the morning is crucial for preventative measures and proactive health management. This section delves into the potential risks associated with persistently high morning blood pressure readings.High morning blood pressure readings are often a warning sign that something more serious might be developing.
It’s not simply a matter of a slightly elevated reading; consistent morning spikes can contribute to a cascade of health problems, including increased cardiovascular risk. Recognizing these implications empowers individuals to take steps towards a healthier lifestyle and potentially prevent more serious issues later on.
Potential Health Implications
Elevated morning blood pressure is a significant indicator of potential health issues. It’s not an isolated event; rather, it’s a potential marker of underlying problems and an increased risk of future cardiovascular complications. This consistent morning elevation can contribute to several conditions, ranging from increased risk of stroke to the development of chronic hypertension.
Link to Cardiovascular Risk Factors
Morning blood pressure elevation is closely linked to various cardiovascular risk factors. Studies show a correlation between consistently high morning blood pressure and an increased likelihood of developing conditions like atherosclerosis, where plaque builds up in the arteries. This narrowing of the arteries can lead to reduced blood flow, impacting organ function and increasing the risk of heart attack or stroke.
Connection to Hypertension Development
Morning blood pressure readings play a critical role in the development of hypertension. A persistent pattern of high morning blood pressure readings is often a precursor to chronic hypertension. This sustained elevation can damage blood vessels over time, leading to the development of hypertension, a condition that significantly increases the risk of heart disease, stroke, and kidney problems.
Comparison with High Blood Pressure Throughout the Day
While high blood pressure throughout the day is a well-recognized risk factor, the impact of consistently high morning blood pressure warrants special attention. The impact of high morning blood pressure is often compounded by the fact that many people are less aware of their morning blood pressure. It’s important to note that while both types of elevated blood pressure carry risks, the consistent morning elevation may signify underlying issues that need further investigation.
The combination of high morning blood pressure with high blood pressure throughout the day further elevates the risk profile.
Relationship to Long-Term Health Outcomes
High morning blood pressure is intricately linked to long-term health outcomes. A consistent pattern of elevated morning blood pressure can lead to a range of adverse health consequences. This includes an increased risk of heart attack, stroke, kidney disease, and peripheral artery disease. It’s important to understand that these outcomes are not inevitable; proactive lifestyle changes and medical interventions can significantly mitigate these risks.
- Increased Risk of Heart Attack: Morning blood pressure spikes can contribute to the buildup of plaque in arteries, increasing the risk of a heart attack.
- Stroke Risk: Elevated morning blood pressure can lead to a higher risk of stroke, a condition that can cause severe neurological damage.
- Kidney Disease: Sustained high morning blood pressure can strain the kidneys, leading to potential damage and the development of chronic kidney disease.
- Peripheral Artery Disease: Consistent high morning blood pressure can contribute to narrowing of blood vessels in the extremities, leading to peripheral artery disease.
Strategies to Manage Morning Blood Pressure
Morning blood pressure spikes can be a frustrating and potentially concerning experience. Understanding the factors contributing to these elevations and implementing effective strategies to manage them is crucial for overall cardiovascular health. This section will delve into practical lifestyle modifications and actionable steps that can help mitigate morning blood pressure surges.
Ever wondered why your blood pressure might be a little higher in the morning? It’s a common question, and often linked to other factors like hydration levels and even the underlying causes of things like watery eyes. For example, dehydration or allergies can contribute to those pesky watery eyes, which might be related to a temporary spike in blood pressure.
So, while the exact reason for morning blood pressure fluctuations is complex, understanding the potential connections, like those between watery eyes and blood pressure, is key to a better understanding of overall health. Learn more about what causes watery eyes to better grasp the bigger picture. Ultimately, morning blood pressure is still a key indicator of your general health.
Lifestyle Modifications for Lowering Morning Blood Pressure
Managing morning blood pressure involves adopting a holistic approach that addresses various lifestyle factors. Consistent healthy habits play a significant role in regulating blood pressure throughout the day, including the morning hours. A well-rounded approach incorporating diet, exercise, sleep, and stress management can significantly contribute to improved blood pressure control.
Importance of Diet and Exercise
A healthy diet rich in fruits, vegetables, and whole grains, coupled with regular physical activity, is fundamental for managing morning blood pressure. A balanced diet helps maintain a healthy weight, a key factor in blood pressure regulation. Regular exercise improves cardiovascular health and helps the body use insulin more effectively, contributing to better blood pressure control. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days a week.
Strategies for Improving Sleep Quality and Duration
Adequate sleep is essential for blood pressure regulation. Insufficient sleep can disrupt the body’s natural rhythms, potentially leading to higher morning blood pressure readings. Prioritize a consistent sleep schedule, create a relaxing bedtime routine, and ensure a conducive sleep environment to promote better sleep quality and duration. Establish a regular sleep-wake cycle, even on weekends, to regulate your body’s natural sleep-wake cycle.
Strategies for Managing Stress and Anxiety
Chronic stress and anxiety can significantly impact blood pressure levels, including morning readings. Incorporating stress-reducing techniques into your daily routine can help maintain healthy blood pressure levels. Techniques such as deep breathing exercises, meditation, yoga, or spending time in nature can contribute to stress reduction and lower morning blood pressure. Consider mindfulness practices, such as meditation, to help manage stress and promote relaxation.
Actionable Steps for Controlling Morning Blood Pressure
To effectively manage morning blood pressure, consider the following actionable steps:
- Maintain a consistent sleep schedule, aiming for 7-9 hours of quality sleep each night.
- Incorporate regular physical activity into your daily routine, aiming for at least 30 minutes of moderate-intensity exercise most days of the week.
- Adopt a healthy diet rich in fruits, vegetables, and whole grains, while limiting processed foods, saturated fats, and sodium intake.
- Practice stress-reducing techniques like deep breathing, meditation, or yoga to manage stress levels.
- Seek professional guidance for stress management and blood pressure control if needed.
Impact of Lifestyle Changes on Morning Blood Pressure
The following table Artikels potential impacts of various lifestyle changes on morning blood pressure levels. It’s important to remember that individual results may vary.
| Lifestyle Change | Potential Impact on Morning Blood Pressure |
|---|---|
| Consistent sleep schedule | Improved sleep quality, potentially leading to lower morning blood pressure |
| Regular exercise | Improved cardiovascular health, leading to better blood pressure control, including morning readings |
| Healthy diet | Maintaining a healthy weight, reducing sodium intake, and providing essential nutrients, contributing to lower morning blood pressure |
| Stress management techniques | Reduced stress levels, which may translate to lower morning blood pressure readings |
Clinical Considerations for Morning Blood Pressure
Morning blood pressure readings hold significant clinical importance, providing valuable insights into cardiovascular health. Understanding the factors influencing these readings, coupled with careful assessment and management strategies, is crucial for effective patient care. This section delves into the critical role of morning blood pressure in diagnosis, treatment, and patient management.
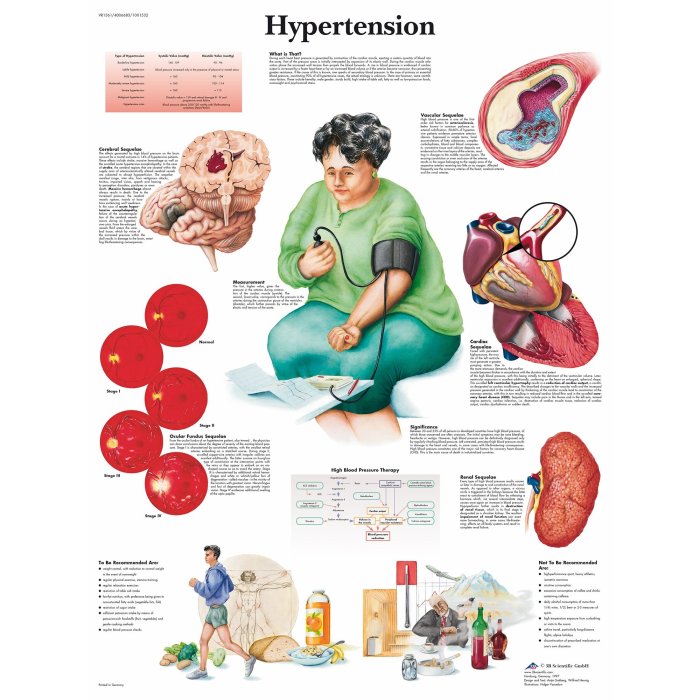
Role of Morning Blood Pressure in Diagnosing and Managing Hypertension
Morning blood pressure often reveals a higher reading compared to other times of the day, a phenomenon known as the “morning surge.” This consistent elevation can be a significant indicator of underlying hypertension, particularly in patients with a history of elevated blood pressure readings throughout the day. Careful monitoring of morning blood pressure can aid in the diagnosis of hypertension in such cases.
Furthermore, tracking morning blood pressure patterns can assist in tailoring treatment plans for optimal control and preventing future complications.
Significance of Morning Blood Pressure in Patient Assessment
Morning blood pressure readings, when viewed in the context of a patient’s overall health profile, can offer valuable insights into their risk of cardiovascular disease. This includes factors like age, family history, lifestyle choices, and other concurrent medical conditions. Assessing morning blood pressure, combined with a comprehensive patient history and physical examination, can refine risk stratification and guide preventive interventions.
A consistent high morning blood pressure in a patient with known risk factors warrants more intensive monitoring and proactive management.
Implications of Morning Blood Pressure for Patients with Pre-existing Conditions
Morning blood pressure elevations can have substantial implications for patients with pre-existing conditions, particularly those with diabetes, chronic kidney disease, or heart failure. These conditions often increase the risk of cardiovascular complications, and morning blood pressure can provide an early warning signal of potential deterioration. Patients with such conditions should be closely monitored for morning blood pressure spikes and their associated implications.
For instance, a sudden increase in morning blood pressure in a patient with chronic kidney disease might signal the need for immediate intervention.
Different Scenarios and Clinical Situations
Several clinical situations highlight the importance of morning blood pressure readings in diagnosis and treatment. For instance, a patient presenting with symptoms of headache and dizziness, accompanied by a consistently elevated morning blood pressure, warrants immediate investigation for possible hypertensive crisis. Similarly, in patients experiencing nocturnal hypertension (high blood pressure during sleep), morning readings can be instrumental in understanding the overall blood pressure pattern and the need for comprehensive management.
Morning blood pressure assessment is also critical for patients taking antihypertensive medications, to evaluate the effectiveness of the treatment and adjust dosages as needed.
Comparison of Diagnostic Methods for Morning Blood Pressure
| Diagnostic Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Home Blood Pressure Monitoring (HBPM) | Self-measured blood pressure readings taken at home. | Convenient, provides insight into variability throughout the day, and can detect hidden hypertension. | Requires patient adherence, potential for inaccurate readings if technique is not proper. |
| Ambulatory Blood Pressure Monitoring (ABPM) | Continuous blood pressure monitoring over 24 hours, providing a comprehensive profile. | Detailed assessment of blood pressure throughout the day and night, identifies nocturnal hypertension. | Invasive, may cause discomfort for some patients. |
| Office Blood Pressure Measurement | Blood pressure measured during a routine visit. | Quick and readily available. | May not reflect true blood pressure variability throughout the day. |
Morning blood pressure measurement using various methods, including home monitoring, ambulatory monitoring, and office measurements, allows for a comprehensive assessment of blood pressure patterns and the potential risks associated with high morning blood pressure.
Last Recap
In summary, understanding why blood pressure is often higher in the morning is a vital step in maintaining overall health and well-being. By considering the interplay of circadian rhythms, stress hormones, sleep patterns, medications, and lifestyle factors, we can develop effective strategies to manage morning blood pressure fluctuations. This knowledge empowers individuals to take control of their health and make informed decisions about their well-being.