Portfolio diet heart health is a comprehensive approach to achieving and maintaining cardiovascular well-being. It’s not about strict adherence to one single diet, but rather strategically incorporating diverse dietary patterns to support optimal heart health. This includes understanding different approaches like the Mediterranean or DASH diet, and recognizing the vital role of various nutrients and…
Tag: heart health
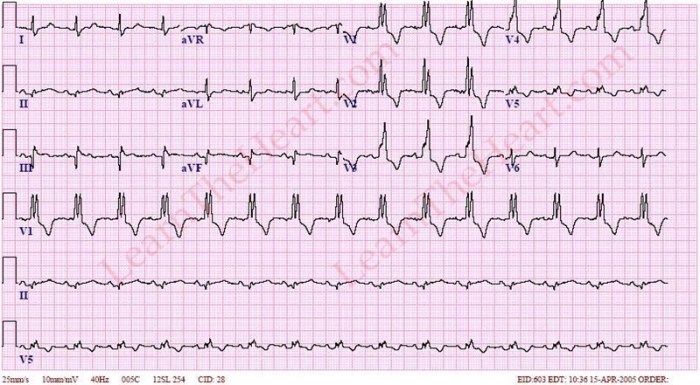
Right Bundle Branch Block (RBBB) A Comprehensive Guide
Right bundle branch block rbbb – Right bundle branch block (RBBB) is a common heart condition where the electrical signal traveling through the heart’s conduction system encounters a delay or obstruction. Understanding the intricacies of RBBB involves exploring its causes, symptoms, diagnosis, and management. This comprehensive guide will take you through the anatomy, clinical presentation,…
Why Am I So Tired After Cardiac Ablation?
Why am I so tired after my cardiac ablation? This question plagues many patients who undergo this procedure. The recovery process can be surprisingly complex, with a range of factors contributing to post-procedure fatigue. From the physiological effects of the ablation itself to pre-existing health conditions and lifestyle choices, understanding the reasons behind this fatigue…
How to Reverse Atrial Fibrillation Naturally A Guide
How to reverse atrial fibrillation naturally is a crucial question for many seeking alternative or complementary approaches to managing this condition. This guide delves into potential lifestyle modifications, dietary recommendations, herbal remedies, nutritional considerations, and mind-body practices that may help. We’ll explore various strategies, but remember that natural remedies are not a substitute for professional…
Cardiac Effects of Obesity Medications A Deep Dive
Cardiac effects of obesity medications are a crucial area of study, as these drugs can potentially impact the cardiovascular system. This blog post explores the different classes of obesity medications currently available, examining their mechanisms of action and potential physiological pathways through which they might affect the heart. We’ll delve into the potential cardiac risks…
Can GERD Cause Heart Palpitations?
Can GERD cause heart palpitations? This is a question that often arises for those experiencing both acid reflux and unusual heart sensations. Understanding the potential link between these two seemingly disparate conditions is crucial for accurate diagnosis and effective management. This exploration dives deep into the possible connections, symptoms, and considerations, helping readers navigate this…
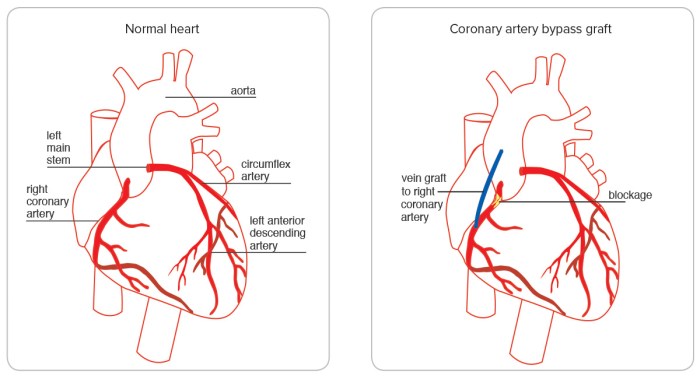
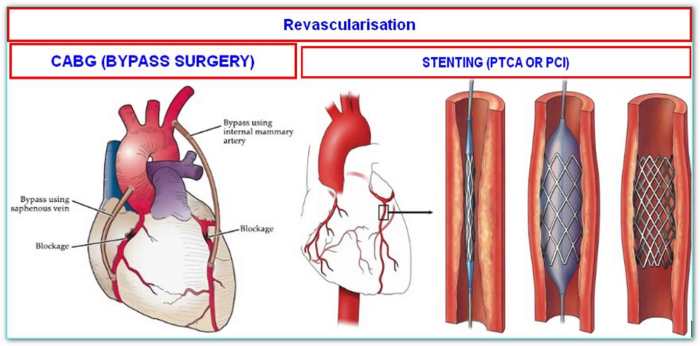
What is Quadruple Bypass Heart Surgery? A Deep Dive
What is quadruple bypass heart surgery? This procedure involves rerouting blood flow around blocked coronary arteries in the heart. It’s a significant surgical intervention, often chosen when other treatments aren’t sufficient. Understanding the details, from the reasons for the surgery to the potential long-term effects, is crucial for anyone considering or learning about this complex…
What is a Double Bypass Heart Surgery? A Comprehensive Guide
What is a double bypass heart surgery? This procedure, a significant step in cardiovascular care, aims to improve blood flow to the heart. It involves rerouting blood flow around blocked coronary arteries, often caused by atherosclerosis. Understanding the historical context, different types of bypasses, and the meticulous preparation and recovery process is crucial for patients…
The Benefits of Hawthorn A Comprehensive Guide
The benefits of hawthorn, a versatile plant with a rich history, are now being explored more deeply than ever. From its traditional use in various cultures to modern scientific research, hawthorn’s potential for promoting cardiovascular health and well-being is truly remarkable. This comprehensive guide delves into the different aspects of hawthorn, examining its nutritional profile,…
Aerobic Exercise Fights Stiff Heart
Aerobic exercise fights stiff heart, offering a powerful pathway to a healthier cardiovascular system. This exploration delves into the science behind how regular physical activity can counteract the hardening of arteries, improving heart health and overall well-being. We’ll examine the different types of aerobic exercise, their impact on heart stiffness, and the crucial role of…