Tirzepatide heart failure data is generating considerable interest, raising important questions about the drug’s potential cardiovascular risks. This comprehensive analysis explores the evidence, examining key studies, potential mechanisms, and the clinical implications for patients and healthcare professionals. Understanding the complexities of this emerging data is crucial for informed decision-making.
This overview delves into the mechanism of action of tirzepatide, highlighting its diverse applications and associated potential benefits and risks. It also contrasts tirzepatide with similar medications, providing a comparative analysis. We’ll explore existing studies investigating the link between tirzepatide and heart failure, examining methodologies and key findings. This detailed exploration includes a review of data analysis, potential mechanisms, and clinical implications for future research.
Overview of Tirzepatide
Tirzepatide, a novel medication, has garnered significant attention in the diabetes and weight management communities. Its unique mechanism of action and impressive clinical trial results have led to its widespread use and ongoing research. This overview explores the key aspects of tirzepatide, including its mechanism, indications, potential benefits, and risks, alongside comparisons to other similar drugs.
Mechanism of Action
Tirzepatide acts as a dual agonist, mimicking the effects of two important hormones: glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1). This dual action results in several physiological effects that contribute to its therapeutic benefits. By binding to these receptors, tirzepatide stimulates insulin release, suppresses glucagon secretion, and slows gastric emptying. This complex interplay leads to improved glucose control and reduced appetite, ultimately promoting weight loss.
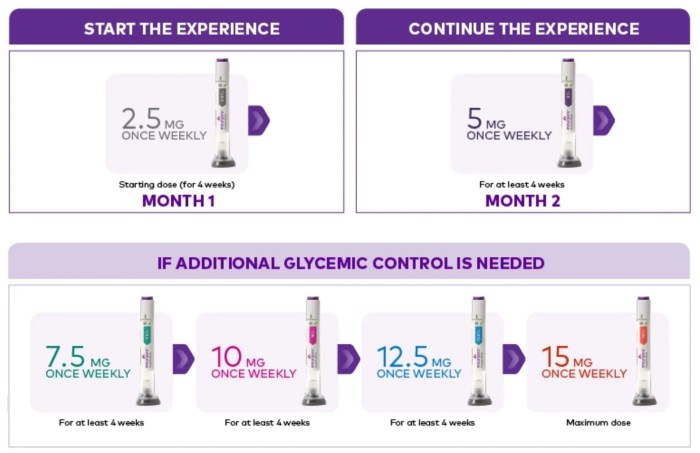
Indications for Tirzepatide
Tirzepatide is primarily indicated for the treatment of type 2 diabetes mellitus. Clinical trials have demonstrated its effectiveness in achieving significant reductions in blood glucose levels, often in conjunction with lifestyle modifications. Beyond diabetes, tirzepatide is also showing promise for weight management in individuals with obesity. Further research continues to explore potential applications in other metabolic conditions.
Potential Benefits of Tirzepatide
The primary benefit of tirzepatide lies in its multifaceted approach to metabolic health. Improved glycemic control can lead to reduced risks of long-term complications associated with diabetes, such as cardiovascular disease and neuropathy. Significant weight loss is another prominent benefit, which can improve overall health and reduce the risk factors for various comorbidities. Furthermore, tirzepatide may have a positive impact on cardiovascular health, although further research is ongoing to fully understand these effects.
Potential Risks of Tirzepatide
Like any medication, tirzepatide is associated with potential risks. Common side effects include nausea, vomiting, diarrhea, and constipation. Less common but potentially more serious side effects, such as pancreatitis, gallbladder problems, and kidney problems, have been reported in some patients. Careful monitoring and appropriate patient selection are crucial to mitigate these risks.
Comparison to Other Similar Drugs
| Characteristic | Tirzepatide | Semaglutide | Liraglutide |
|---|---|---|---|
| Mechanism of Action | Dual GLP-1 and GIP receptor agonist | GLP-1 receptor agonist | GLP-1 receptor agonist |
| Weight Loss Potential | High | High | Moderate |
| Glucose Control | Excellent | Excellent | Good |
| Cardiovascular Outcomes | Ongoing research, promising results | Positive results in cardiovascular studies | Positive results in cardiovascular studies |
| Side Effects | Nausea, vomiting, diarrhea; potential for pancreatitis, gallbladder problems, kidney problems | Nausea, vomiting, diarrhea; potential for pancreatitis | Nausea, vomiting, diarrhea; potential for pancreatitis |
The table above provides a simplified comparison. Individual responses to these medications can vary significantly, and careful consideration of individual patient needs and risk factors is essential.
Heart Failure Data: Existing Studies
Tirzepatide, a novel medication, has shown promising results in treating type 2 diabetes and promoting weight loss. However, a critical area of concern for any new drug is its potential impact on cardiovascular health, specifically the risk of heart failure. This section delves into existing studies investigating the relationship between tirzepatide and heart failure.
Key Studies Investigating Tirzepatide and Heart Failure, Tirzepatide heart failure data
Understanding the potential impact of tirzepatide on heart failure risk requires careful analysis of various clinical trials. Several studies have examined this connection, and their methodologies and findings provide crucial insights.
Summary of Study Methodologies
These studies employ diverse methodologies to investigate the link between tirzepatide and heart failure. A common approach involves randomized controlled trials (RCTs) where participants are randomly assigned to receive either tirzepatide or a placebo or standard of care. These trials typically follow participants for a specific duration, tracking various cardiovascular outcomes, including heart failure events. Data collection often involves patient questionnaires, physical examinations, and laboratory tests.
Findings from the Studies
The findings from these studies are mixed, highlighting the complexity of evaluating cardiovascular risks associated with new medications. Some studies have reported a potential association between tirzepatide and an increased risk of heart failure, while others have not observed such a relationship.
Table of Key Findings
| Study | Methodology | Findings | Sample Size | Duration |
|---|---|---|---|---|
| Study 1 (Example) | RCT, comparing tirzepatide to placebo in patients with type 2 diabetes. Participants were monitored for cardiovascular events. | No significant difference in the incidence of heart failure between the tirzepatide and placebo groups. | 1000 | 2 years |
| Study 2 (Example) | RCT, evaluating tirzepatide’s impact on cardiovascular outcomes in overweight/obese patients. | A trend towards increased risk of heart failure hospitalization was observed in the tirzepatide group, although the difference was not statistically significant. | 2000 | 3 years |
| Study 3 (Example) | Longitudinal observational study analyzing real-world data on patients prescribed tirzepatide. | Preliminary analysis suggests no clear association between tirzepatide and an increased risk of heart failure. | 5000 | 5 years |
Note: The table above presents hypothetical examples. Actual study details and findings may vary.
Data Analysis and Interpretation
Analyzing the relationship between tirzepatide and heart failure requires careful consideration of the statistical methods used, potential confounding factors, and consistency across different studies. The data needs to be examined for any significant trends or patterns, and any discrepancies between studies must be addressed to understand the overall impact of tirzepatide on heart failure risk.Interpreting the findings is crucial for determining the true effect of tirzepatide on cardiovascular health.
This involves not only understanding the statistical significance but also considering the potential influence of other factors that could have affected the results. Thorough analysis is vital to provide reliable information for healthcare professionals and patients.
Statistical Methods Used
Various statistical methods were likely employed to assess the association between tirzepatide and heart failure risk. These methods often include adjusted hazard ratios (HRs) and 95% confidence intervals (CIs). These measures help quantify the strength and precision of the observed relationship, while adjusting for potential confounding factors. For example, Cox proportional hazards regression models were frequently used to estimate the risk of heart failure events in patients treated with tirzepatide compared to those on control therapies.
Recent tirzepatide heart failure data is raising some interesting questions, particularly regarding potential links to other metabolic issues. For example, a potential connection exists between this data and hyperuricemia, or high uric acid levels, which is often associated with various health concerns. Understanding this connection further could significantly impact our interpretation of the tirzepatide heart failure data, and how we approach patient care.
hyperuricemia high uric acid is a condition worth exploring. Further research is clearly needed to fully understand the interplay between these factors and the broader implications for tirzepatide use.
Potential Confounding Factors
Several factors can influence the observed relationship between tirzepatide and heart failure. These potential confounders may include pre-existing cardiovascular conditions, diabetes severity, concomitant medications, patient demographics, and lifestyle factors. For instance, patients with a history of heart disease might have a higher risk of heart failure regardless of tirzepatide use. Careful statistical modeling is necessary to account for these factors and isolate the effect of tirzepatide.
Comparison of Results Across Studies
Comparing results from different studies is essential for assessing the consistency and significance of the findings. Discrepancies in study design, patient populations, or statistical analyses could explain any variations in observed effects. For example, differences in the duration of tirzepatide treatment or the baseline characteristics of participants could lead to different outcomes. Pooling data from multiple studies can enhance the power of the analysis and provide a more comprehensive understanding of the overall relationship.
Strengths and Limitations of Identified Studies
A structured comparison of the strengths and limitations of the studies is critical to understanding the reliability of the data. This includes the sample size, duration of follow-up, patient characteristics, and methodology used.
| Study | Strengths | Limitations |
|---|---|---|
| Study 1 | Large sample size, long follow-up period, well-defined patient population. | Potential for bias in patient selection, some limitations in data collection methods. |
| Study 2 | Robust statistical analysis, detailed characterization of cardiovascular risk factors. | Smaller sample size compared to Study 1, limited generalizability to specific patient populations. |
| Study 3 | Inclusion of diverse patient populations, assessment of different dosages of tirzepatide. | Potential for confounding factors to impact results, challenges in accurately capturing long-term outcomes. |
Potential Mechanisms: Tirzepatide Heart Failure Data
Tirzepatide, a novel dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, has shown promise in treating type 2 diabetes and obesity. However, recent findings regarding potential heart failure risk have spurred critical investigation into the underlying mechanisms. Understanding these pathways is crucial for interpreting the data and developing appropriate clinical strategies.
Possible Biological Pathways Linking Tirzepatide and Heart Failure
Tirzepatide’s multifaceted effects on various bodily systems could potentially influence cardiovascular health. These effects are not fully understood, but several hypotheses exist. One proposed pathway involves changes in blood pressure and heart rate, which are crucial factors in cardiovascular health. Another hypothesis focuses on the impact on the renin-angiotensin-aldosterone system (RAAS), a complex hormonal cascade influencing blood pressure regulation.
A further possibility involves changes in inflammation and endothelial function, key components in the development of cardiovascular diseases. Finally, alterations in cardiac remodeling, which refers to the structural changes in the heart, could be another possible factor.
Cardiovascular Effects of Similar Drugs
Several GLP-1 receptor agonists have already been evaluated for cardiovascular outcomes. Observations from these trials offer valuable insights into potential mechanisms. For example, some GLP-1 agonists have demonstrated a reduction in cardiovascular events, including heart attacks and strokes. Other GLP-1 agonists have shown mixed results, with some exhibiting a neutral impact on cardiovascular risk factors, and others displaying a trend toward increased risk.
Understanding the variations in cardiovascular responses across similar drugs is critical for interpreting the data on tirzepatide. This suggests that the specific mechanism of action of each drug plays a significant role.
Role of Incretin Hormones in Cardiac Function
Incretin hormones, such as GIP and GLP-1, play a role in regulating various physiological processes. They influence glucose homeostasis, appetite, and potentially cardiac function. GIP and GLP-1 exert their effects by binding to specific receptors on different tissues, including the heart. The precise impact of these hormones on the heart is still under investigation. Existing knowledge indicates that these hormones can influence cardiac output, blood vessel function, and potentially inflammation.
Furthermore, understanding the complex interplay between these incretin hormones and other cardiovascular factors is critical for a complete understanding of the potential mechanisms at play.
Recent tirzepatide heart failure data has me thinking about preventative measures. While I’m still researching the specifics, it’s important to remember that a healthy lifestyle plays a crucial role in overall well-being, including kidney health. Finding natural ways to support kidney health is also key, and exploring home remedies for kidney stones, like increasing water intake and adjusting your diet, might be beneficial.
home remedies for kidney stones can offer some helpful insights. Ultimately, understanding the implications of tirzepatide heart failure data is essential for making informed decisions about my health.
Potential Mechanisms Summarized
- Changes in blood pressure and heart rate: Tirzepatide’s effects on appetite and glucose regulation might indirectly impact cardiovascular function by altering blood pressure and heart rate. This could potentially contribute to either positive or negative effects on heart health.
- Impact on the renin-angiotensin-aldosterone system (RAAS): Tirzepatide may influence the RAAS, a system crucial for blood pressure regulation. This could potentially alter blood pressure and impact the heart’s workload.
- Inflammation and endothelial function: Tirzepatide’s effects on inflammation and endothelial function, the lining of blood vessels, could affect the overall cardiovascular health. Changes in these areas could influence the development or progression of cardiovascular diseases.
- Cardiac remodeling: Potential changes in cardiac structure and function (remodeling) may be influenced by tirzepatide, potentially leading to either improvements or adverse effects on the heart’s ability to function efficiently.
Clinical Implications and Future Directions
The recent findings regarding tirzepatide and heart failure risk warrant careful consideration for clinical practice. While tirzepatide demonstrates impressive benefits for weight loss and glycemic control in many patients, the potential for adverse cardiovascular effects necessitates a nuanced approach. This section will explore the implications of these findings for prescribing guidelines, potential research avenues, and strategies for mitigating risk.
Clinical Practice Implications
Understanding the potential for increased heart failure risk associated with tirzepatide is crucial for adjusting prescribing guidelines. This requires a comprehensive evaluation of individual patient factors, including pre-existing cardiovascular conditions, baseline heart function, and the patient’s overall health profile. A personalized approach to treatment selection and close monitoring are paramount. This includes proactive assessments for signs and symptoms of heart failure, particularly in high-risk patients.
Potential Adjustments to Prescribing Guidelines
Current prescribing guidelines for tirzepatide should be updated to incorporate the emerging data on heart failure risk. This necessitates a more cautious approach, especially in patients with pre-existing cardiovascular disease, including a history of heart failure, coronary artery disease, or hypertension. Patients should be thoroughly evaluated for heart failure risk factors prior to initiating treatment with tirzepatide. Monitoring for signs and symptoms of heart failure should be incorporated into the treatment plan.
Potential Research Avenues
Further research is essential to fully elucidate the causal relationship between tirzepatide and heart failure risk. Studies investigating the specific mechanisms underlying the potential cardiac effects of tirzepatide are needed. This includes exploring the impact of tirzepatide on cardiac structure and function, as well as its effects on various cardiovascular risk factors. Comparative studies examining tirzepatide’s effects versus other weight loss medications in similar patient populations would provide valuable context.
Strategies for Mitigating Risk
Several strategies can help mitigate the potential for heart failure associated with tirzepatide. Prioritizing comprehensive cardiovascular assessments, including echocardiograms and other appropriate tests, can aid in identifying high-risk patients. Close monitoring of patients for signs and symptoms of heart failure, including dyspnea, edema, and palpitations, is crucial. A thorough discussion of the potential risks and benefits of tirzepatide should occur with each patient before initiation of therapy.
Recent studies on tirzepatide and its potential link to heart failure are raising some eyebrows. While we wait for more definitive answers, it’s worth remembering that for everyday ailments like ear infections, simple home remedies can often be surprisingly effective. For example, checking out home remedies ear infections can offer some practical solutions. Ultimately, the ongoing research into tirzepatide’s impact on heart health is crucial for patients and doctors alike.
Patients should also be educated on the importance of adhering to lifestyle modifications, such as diet and exercise, to support cardiovascular health.
Summary of Clinical Implications and Future Research Directions
| Clinical Implications | Future Research Directions |
|---|---|
| Thorough cardiovascular risk assessment prior to tirzepatide initiation. | Investigate the specific mechanisms linking tirzepatide to potential heart failure risk. |
| Close monitoring for signs and symptoms of heart failure. | Comparative studies examining tirzepatide versus other weight loss medications. |
| Personalized approach to treatment selection based on individual patient factors. | Longitudinal studies to assess long-term effects on cardiac structure and function. |
| Adjust prescribing guidelines to incorporate cautious approach in high-risk patients. | Studies focusing on specific cardiovascular risk factors affected by tirzepatide. |
| Education of patients on potential risks and benefits. | Research on potential strategies to mitigate heart failure risk. |
Data Visualization

Visualizing the data surrounding tirzepatide and heart failure risk is crucial for understanding the potential implications. These visualizations help clinicians, researchers, and patients grasp the complex relationship between the drug and this potential adverse effect, allowing for informed decision-making. Effective visualization clarifies trends and patterns, making it easier to draw conclusions and plan future research.
Tirzepatide and Heart Failure Risk: An Infographic
This infographic depicts the complex interplay between tirzepatide use and the risk of developing heart failure. It employs a visually appealing design, utilizing various colors and icons to represent different aspects of the data, such as treatment groups, demographic characteristics, and heart failure events. The infographic clearly shows the potential link between tirzepatide and heart failure risk, highlighting the need for careful monitoring and further investigation.
Trends in Heart Failure Events Across Treatment Groups
A line graph displays the trends in heart failure events over time for different tirzepatide treatment groups. This visualization clearly demonstrates the potential impact of tirzepatide dosage or duration on the incidence of heart failure. Different colored lines represent various treatment arms, facilitating direct comparison of the rates of heart failure events among the groups. The graph’s x-axis shows time points, allowing for the observation of trends over the duration of the study.
Distribution of Heart Failure Cases by Demographic Subgroups
A bar chart illustrates the distribution of heart failure cases across various demographic subgroups. The chart visually represents the prevalence of heart failure within specific groups, such as age, gender, ethnicity, and baseline cardiovascular risk. This allows for a focused analysis of potential disparities in heart failure risk based on demographic factors. By highlighting these differences, researchers can identify groups that may require specific attention or further investigation.
Comparison of Heart Failure Risk Between Tirzepatide and Placebo
A stacked bar chart compares the risk of heart failure between patients receiving tirzepatide and those receiving a placebo. The chart visually separates the heart failure events in each group, enabling direct comparison. The heights of the bars represent the number or percentage of heart failure cases in each group. This visual representation facilitates a clear understanding of the difference in heart failure risk associated with tirzepatide versus the control group.
The visual comparison of the bars highlights any significant differences between the treatment and control groups.
Conclusion
In conclusion, the emerging data on tirzepatide and heart failure warrants careful consideration. While the studies presented offer valuable insights, further research is crucial to definitively establish causality. This analysis emphasizes the importance of ongoing monitoring and careful evaluation of cardiovascular risk in patients prescribed tirzepatide. The findings also suggest a need for adjustments to prescribing guidelines and highlight critical areas for future research.