What cold fingers mean goes beyond simple chill. This exploration delves into the diverse factors that can cause those icy extremities, from underlying medical conditions to environmental triggers and even lifestyle choices. Understanding the potential causes of cold fingers is crucial for recognizing potential problems and taking appropriate steps to maintain your well-being.
We’ll examine the physiological mechanisms behind cold fingers, exploring everything from circulatory issues to stress responses. We’ll also look at how environmental factors like temperature and humidity can affect blood flow, and how lifestyle choices, diet, and exercise play a role in keeping your fingers warm.
Underlying Medical Conditions
Cold fingers, a common complaint, can stem from various underlying medical conditions. Understanding the physiological mechanisms behind these conditions is crucial for accurate diagnosis and appropriate treatment. While often a symptom of a more significant issue, cold fingers can also be a normal response to environmental factors. This section delves into the medical conditions associated with cold extremities, highlighting the physiological processes and accompanying symptoms.
Peripheral Vascular Disease
Peripheral vascular disease (PVD) encompasses a group of conditions that affect the blood vessels outside the heart and brain. These conditions restrict blood flow to the extremities, including the fingers. This reduced blood flow results in decreased delivery of oxygen and nutrients, leading to a sensation of coldness.
- Mechanism: Narrowed or blocked arteries in the extremities, often due to atherosclerosis (plaque buildup), impair blood circulation. This is particularly common in individuals with a history of smoking, high cholesterol, or diabetes. The body’s inability to deliver adequate blood to the extremities results in decreased temperature.
- Symptoms: Coldness in the fingers and toes, often accompanied by numbness, tingling, pain, and cramping, particularly during exercise or exposure to cold. Skin discoloration (pale or bluish), especially in the extremities, can also be a symptom. Ulcers or sores on the affected areas can also develop over time.
Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition characterized by episodes of reduced blood flow to the fingers and toes. These episodes are often triggered by cold temperatures or emotional stress.
- Mechanism: In Raynaud’s, the small blood vessels in the extremities constrict excessively in response to cold or stress. This constriction reduces blood flow, causing the affected areas to become cold, numb, and pale. The body’s reaction to cold, stress, or other factors leads to vasoconstriction.
- Symptoms: The most prominent symptom is episodic attacks of cold, numb, and pale fingers and toes. The affected areas may also feel tingling or painful. The episodes often resolve on their own as blood flow returns. Color changes (white, blue, red) are frequently observed during an attack.
Hypothyroidism
Hypothyroidism, an underactive thyroid gland, can contribute to cold extremities. The thyroid gland plays a vital role in regulating body temperature, and its underactivity can lead to decreased metabolism and a general feeling of coldness.
- Mechanism: A low level of thyroid hormones can slow down the metabolic rate, impacting heat production in the body. This can lead to a general feeling of coldness throughout the body, including the extremities.
- Symptoms: Cold intolerance, along with other symptoms like fatigue, weight gain, constipation, and dry skin, are common in hypothyroidism. The cold sensation in the fingers and toes is often just one aspect of the overall reduced body temperature.
Diabetes
Diabetes can also cause cold extremities, although the mechanisms are multifactorial. Nerve damage (neuropathy) and reduced blood flow are common factors.
- Mechanism: High blood sugar levels over time can damage nerves and blood vessels. This nerve damage can affect the ability to sense temperature, leading to a reduced awareness of cold in the extremities. Reduced blood flow, often a consequence of vascular damage, further contributes to the coldness.
- Symptoms: Numbness, tingling, and pain in the extremities, often in the hands and feet, are common symptoms of diabetic neuropathy. Coldness in the extremities may be one aspect of this symptom complex. Skin sores or ulcers may develop over time due to reduced blood flow and nerve damage.
Table: Comparing Symptoms and Potential Causes
| Condition | Potential Causes | Symptoms (including cold fingers) |
|---|---|---|
| Peripheral Vascular Disease | Atherosclerosis, smoking, high cholesterol, diabetes | Coldness, numbness, tingling, pain, cramping in extremities, skin discoloration, ulcers |
| Raynaud’s Phenomenon | Cold temperatures, stress, emotional factors | Episodic attacks of cold, numb, and pale fingers and toes, tingling, pain, color changes |
| Hypothyroidism | Underactive thyroid gland | Cold intolerance, fatigue, weight gain, constipation, dry skin, cold fingers |
| Diabetes | High blood sugar, nerve damage, vascular damage | Numbness, tingling, pain in extremities, coldness, skin sores, ulcers |
Environmental Factors
Cold fingers, often a bothersome discomfort, can stem from various environmental conditions. Understanding these factors is crucial for prevention and effective management of this common ailment. Exposure to cold temperatures is a primary culprit, but other environmental elements also play a role. Let’s delve into the intricate relationship between the environment and peripheral blood flow.Environmental factors can significantly influence blood circulation in the extremities, leading to cold fingers.
These factors affect the body’s ability to maintain a normal temperature in the hands and feet. The principle at play is vasoconstriction – the narrowing of blood vessels – which reduces blood flow to the extremities to conserve heat in the core body. This protective mechanism is essential for survival in cold environments, but can be problematic if the cold exposure is prolonged or intense.
Temperature Extremes and Peripheral Blood Flow
Temperature is the most significant environmental factor affecting peripheral blood flow and subsequently, the temperature of the extremities. When exposed to cold temperatures, the body’s natural response is to constrict blood vessels in the skin to preserve core body heat. This reduction in blood flow to the periphery directly impacts the temperature of the fingers, causing them to feel cold.
Lower temperatures trigger a more pronounced vasoconstriction response, resulting in a greater drop in finger temperature. Conversely, warmer temperatures allow for vasodilation, increasing blood flow and restoring warmth to the extremities. For example, a sudden drop from a warm indoor environment to a significantly colder outdoor environment can rapidly cause vasoconstriction, leading to cold fingers.
Environmental Triggers for Cold Fingers
Environmental conditions significantly impact peripheral blood flow. Understanding these factors can aid in preventative measures. Prolonged exposure to cold temperatures, especially in combination with wind chill, is a significant factor in cold-induced peripheral vasoconstriction. The following table Artikels common environmental triggers, including temperature ranges, humidity levels, and exposure duration. It is important to note that individual responses vary, and these are general guidelines.
| Environmental Trigger | Temperature Range (°C) | Humidity (%) | Duration of Exposure (hours) |
|---|---|---|---|
| Mild Cold | 5-10°C | Low to Moderate | 1-3 |
| Moderate Cold | 0-5°C | Low to Moderate | 3-6 |
| Severe Cold | Below 0°C | Low to Moderate | 1-2 |
| Wind Chill | Below 0°C (with wind) | Variable | Short |
| Wet Cold | 5-15°C | High | 1-2 |
Lifestyle Factors: What Cold Fingers Mean
Our lifestyle choices play a significant role in regulating body temperature and blood flow, which directly impact the temperature of our extremities, including our fingers. Understanding how diet, exercise, and stress influence these processes is crucial for managing cold fingers effectively. Certain lifestyle habits can either enhance or hinder healthy blood circulation, contributing to or alleviating the issue.Lifestyle choices, from the foods we consume to the amount of physical activity we engage in, influence the delicate balance of our body’s thermal regulation system.
This system, responsible for maintaining a stable internal temperature, also dictates the distribution of blood flow throughout the body. Poor lifestyle choices can disrupt this balance, leading to compromised blood circulation in the extremities and the experience of cold fingers.
Cold fingers can sometimes be a sign of something a little more than just the chill in the air. It could be a sign of a nutrient deficiency, and eating foods rich in magnesium like nuts high in magnesium might help. A balanced diet, including plenty of magnesium-rich foods, can often help to alleviate cold fingers and improve overall well-being.
Impact of Diet on Hand Temperature, What cold fingers mean
A balanced diet rich in essential nutrients is vital for maintaining overall health and supporting healthy blood circulation. Nutrients like iron, vitamin B12, and folate are crucial for red blood cell production, which carries oxygen throughout the body, including the hands. A deficiency in these nutrients can impair blood flow, leading to cold fingers. Similarly, a diet high in processed foods, saturated fats, and excessive sugar can negatively affect blood vessel health, potentially contributing to poor circulation.
Impact of Exercise on Blood Flow
Regular physical activity is essential for promoting healthy blood circulation. Exercise increases heart rate and blood flow, ensuring oxygen and nutrients reach all parts of the body, including the extremities. This improved circulation can help warm the hands and reduce the sensation of coldness. In contrast, a sedentary lifestyle can lead to sluggish blood flow, making the hands more susceptible to feeling cold.
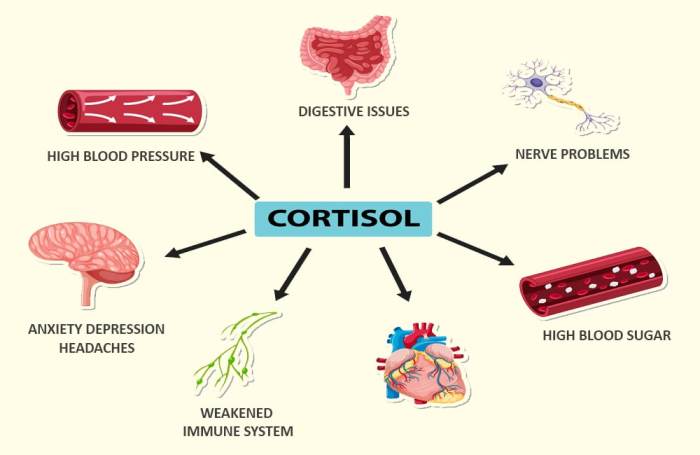
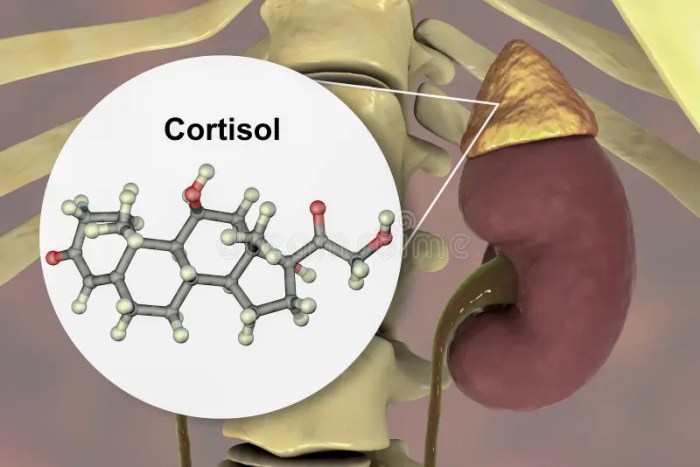
Stress and its Effect on Circulation
Chronic stress can significantly impact blood flow to the extremities. Stress hormones, such as cortisol, can constrict blood vessels, reducing blood flow to the hands and other areas. This constriction can lead to cold fingers, particularly in individuals already prone to poor circulation. Mindfulness techniques, relaxation exercises, and stress management strategies can help regulate stress levels and improve blood circulation.
Lifestyle Choices Affecting Blood Circulation
Maintaining healthy blood circulation in the hands requires a holistic approach. Certain lifestyle choices can either promote or hinder this process.
| Lifestyle Choices | Promote Healthy Blood Circulation | Hinder Healthy Blood Circulation |
|---|---|---|
| Diet | Balanced diet rich in iron, vitamin B12, folate, and healthy fats | Diet high in processed foods, saturated fats, and excessive sugar |
| Exercise | Regular physical activity (aerobic and strength training) | Sedentary lifestyle |
| Stress Management | Mindfulness, meditation, yoga, relaxation techniques | Chronic stress, lack of stress management |
| Smoking | N/A | Smoking significantly compromises blood vessel health, leading to reduced blood flow. |
| Hydration | Adequate water intake | Dehydration |
Circulatory Issues
Cold fingers can often be a symptom of underlying circulatory problems. These issues disrupt the normal flow of blood throughout the body, particularly affecting the extremities like the hands and feet. Understanding these circulatory problems is crucial for identifying the cause of cold fingers and seeking appropriate medical attention. Knowing the specific ways these problems affect blood flow, symptoms, and progression can empower you to better manage the condition.Circulatory issues, often stemming from narrowed or damaged blood vessels, can lead to reduced blood flow to the hands and fingers.
This reduced perfusion can result in a variety of symptoms, including cold fingers, numbness, tingling, and pain. The severity and specific presentation of these symptoms can vary depending on the underlying condition. Recognizing these patterns can be helpful in determining the potential cause and facilitating early intervention.
Common Circulatory Problems Causing Cold Fingers
Peripheral artery disease (PAD) is a common condition in which the arteries in the extremities, including the hands and feet, narrow, reducing blood flow. This narrowing is often due to plaque buildup, a common result of high cholesterol, high blood pressure, and smoking. Raynaud’s phenomenon is another condition that can lead to cold fingers, characterized by episodes of reduced blood flow to the extremities, often triggered by cold temperatures or stress.
This condition can affect individuals with various underlying medical conditions, and it’s important to distinguish it from other circulatory issues. Other potential circulatory problems, like venous insufficiency, affect blood return to the heart, and this can lead to swelling and other symptoms, which may or may not include cold fingers, depending on the severity and the specific location of the venous issue.
Cold fingers can sometimes be a symptom of something more serious, like peripheral neuropathy or even conditions like Raynaud’s phenomenon. However, in some cases, cold fingers can be a symptom of a more serious underlying issue such as HIV wasting syndrome, an AIDS defining condition. This is a serious issue, and if you’re experiencing persistent cold fingers, along with other symptoms, it’s crucial to seek medical attention immediately to determine the underlying cause.
Learning more about HIV wasting syndrome and its connection to health can be beneficial at hiv wasting syndrome aids defining condition for a deeper understanding. Ultimately, understanding the potential causes of cold fingers is key to taking the necessary steps towards better health.
Specific Effects on Blood Flow
In peripheral artery disease, the narrowing of arteries directly restricts blood flow to the hands and fingers. This reduction in blood supply can lead to insufficient oxygen and nutrient delivery, causing the fingers to feel cold, numb, or painful. In Raynaud’s phenomenon, the blood vessels in the fingers constrict in response to cold or stress. This vasoconstriction reduces blood flow significantly, leading to a sudden and dramatic drop in temperature in the hands and fingers.
Venous insufficiency, while not directly causing reduced blood flow to the extremities, can lead to pooling of blood in the veins. This can result in impaired circulation and a feeling of heaviness, discomfort, and potential swelling, which may, in some cases, be accompanied by cold fingers.
Symptoms and Progression
The symptoms of circulatory issues related to cold fingers can vary greatly. Early symptoms may be subtle, such as intermittent coldness in the fingers, particularly when exposed to cold temperatures. As the condition progresses, symptoms can become more pronounced, with persistent cold fingers, numbness, and pain, especially during periods of activity or stress. In severe cases, symptoms may include discoloration of the fingers (pale, bluish, or reddish), ulceration, or even tissue damage.
The progression of these symptoms depends largely on the severity and type of the circulatory issue and the individual’s overall health.
Contrasting Signs and Symptoms of Circulatory Disorders
| Circulatory Disorder | Cold Fingers (and other key symptoms) | Other Symptoms |
|---|---|---|
| Peripheral Artery Disease (PAD) | Intermittent coldness, numbness, pain in fingers and toes, especially with exertion. Often worse in the lower extremities. | Cramping in legs and hips, leg pain during exercise that subsides with rest, skin changes, hair loss on legs and feet. |
| Raynaud’s Phenomenon | Sudden, episodic coldness and numbness in fingers and toes, often triggered by cold or stress. Color changes (white, blue, red) are common. | Numbness and tingling, pain in fingers and toes, skin sensitivity. |
| Venous Insufficiency | Cold fingers may be present in some cases, but typically associated with swelling, heaviness, aching in legs and ankles. May or may not be accompanied by cold fingers depending on the specific location of the issue. | Swelling, aching, heaviness in legs and ankles, skin discoloration (sometimes), varicose veins. |
Stress and Anxiety
Cold fingers can be a frustrating and sometimes concerning symptom. While often linked to more obvious physical issues, emotional factors like stress and anxiety can also play a significant role in the experience. Understanding the connection between these mental states and the sensation of cold fingers can lead to better self-management and overall well-being.Stress, in its various forms, can trigger a cascade of physiological responses, and one noticeable manifestation can be cold fingers.
This is not always a direct cause-and-effect relationship, but rather a result of the body’s complex reaction to perceived threats.
Impact on Blood Flow
Stressful situations often activate the body’s “fight-or-flight” response. This response prioritizes blood flow to the muscles and vital organs, potentially diverting it from extremities like the fingers. Reduced blood flow to the periphery leads to a decrease in skin temperature, resulting in the sensation of cold fingers. This is a protective mechanism, designed to ensure the body’s core remains warm and functional during periods of heightened stress.
Physiological Responses
The body’s response to stress involves several physiological changes that contribute to the sensation of cold fingers. These changes include:
- Constriction of blood vessels: The body constricts blood vessels in the extremities to conserve heat and redirect blood flow to vital organs. This leads to decreased blood circulation and reduced warmth in the fingers.
- Increased heart rate: The heart pumps faster to deliver more oxygen and nutrients to the muscles, further diverting blood away from the extremities.
- Hormonal changes: The release of stress hormones, like adrenaline and cortisol, can further constrict blood vessels and alter the body’s temperature regulation mechanisms.
Stress Management Techniques
Recognizing the link between stress and cold fingers is the first step towards managing the problem. Stress management techniques can help mitigate the impact of stress on blood flow and temperature regulation, reducing the frequency and severity of cold fingers.
- Relaxation techniques: Practicing deep breathing exercises, progressive muscle relaxation, or mindfulness meditation can help calm the nervous system and reduce the physiological responses associated with stress. These practices promote a state of calm, reducing the body’s tendency to constrict blood vessels.
- Regular exercise: Physical activity helps improve circulation and promotes overall well-being. A consistent exercise routine can contribute to better blood flow, which helps to maintain a more balanced body temperature, reducing the likelihood of cold fingers during periods of stress.
- Healthy lifestyle: Maintaining a balanced diet, getting adequate sleep, and limiting caffeine and alcohol consumption can support the body’s ability to cope with stress and regulate temperature effectively.
Hypothermia
Cold fingers, a seemingly minor symptom, can be a significant indicator of a potentially serious condition: hypothermia. This occurs when your body loses heat faster than it can produce it, leading to a dangerously low body temperature. Understanding the signs and symptoms, especially in the context of cold fingers, is crucial for prompt intervention and treatment.Hypothermia is a life-threatening condition that develops gradually as the body loses heat.
The initial symptoms often manifest subtly, and can easily be mistaken for other conditions. Recognizing the progression of symptoms, particularly the role of cold fingers, is essential for seeking immediate medical attention. Early intervention significantly increases the chances of a full recovery.
Understanding the Concept of Hypothermia
Hypothermia happens when your body’s core temperature drops below 35°C (95°F). This reduction in core temperature impairs the body’s ability to regulate its functions, leading to a cascade of potentially life-threatening effects. Cold fingers, along with other symptoms, can be a warning sign of this dangerous decline. The severity of the condition correlates directly with the extent of the temperature drop.
Symptoms and Progression of Hypothermia
Hypothermia develops in stages, with each stage characterized by increasing severity of symptoms. Cold fingers often become a prominent feature as the body’s temperature decreases.
- Early Stage (Mild): Initial symptoms might include shivering, numbness, and clumsiness, including in the fingers. Cold fingers may be accompanied by confusion, disorientation, and slurred speech. The body’s shivering mechanism is often the first and most prominent symptom.
- Moderate Stage: As the body temperature drops further, shivering diminishes, and the individual may experience drowsiness, lethargy, and impaired judgment. Cold fingers become more pronounced, losing feeling and exhibiting a pale or bluish discoloration. The individual may become increasingly unresponsive and have difficulty walking. Muscle stiffness and confusion worsen.
- Severe Stage: In this stage, the body’s core temperature is significantly low, often below 32°C (90°F). The individual loses consciousness and becomes unresponsive. Cold fingers, along with other extremities, lose all feeling and exhibit a significant loss of blood flow, resulting in a marked bluish discoloration. Breathing and heart rate may become irregular and dangerously slow. This is a life-threatening stage, requiring immediate medical attention.
Measures to Take in Cases of Suspected Hypothermia
If you suspect someone is experiencing hypothermia, immediate action is crucial. Prompt intervention can significantly improve the outcome.
- Immediate Treatment Options: Remove the affected person from the cold environment and insulate them with blankets or warm clothing. Monitor their breathing and pulse. Avoid giving them alcohol or caffeine, as these can further impair their body’s ability to regulate temperature. Seek immediate medical assistance.
Stages of Hypothermia
The following table Artikels the different stages of hypothermia, including typical symptoms and the severity levels of cold fingers.
Cold fingers can sometimes be a sign of underlying health issues, and it’s important to pay attention to other symptoms. While there’s no single “cure” for cold fingers, managing conditions like type 2 diabetes, which can affect blood circulation, might help. For more information on potential type 2 diabetes cure options, and how they could relate to cold fingers, further research and consultation with a doctor are essential.
Ultimately, understanding the cause of cold fingers is key to effective management and a healthier lifestyle.
| Stage | Body Temperature (°C) | Typical Symptoms | Severity of Cold Fingers |
|---|---|---|---|
| Early (Mild) | 35-32°C | Shivering, numbness, clumsiness, confusion | Cold, numb, potentially pale |
| Moderate | 32-28°C | Shivering stops, drowsiness, lethargy, impaired judgment | Cold, numb, pale or bluish, reduced feeling |
| Severe | Below 28°C | Unconsciousness, irregular breathing and pulse | Cold, numb, severely pale or bluish, significant loss of feeling |
Peripheral Neuropathy
Peripheral neuropathy is a condition affecting the nerves outside the brain and spinal cord. These nerves are crucial for transmitting signals throughout the body, controlling sensations like touch, temperature, and pain. Damage to these nerves can disrupt these signals, leading to a variety of symptoms, including the distressing sensation of cold fingers. Understanding the nuances of peripheral neuropathy and its connection to cold sensations is vital for effective diagnosis and management.
Understanding Peripheral Neuropathy
Peripheral neuropathy is a complex condition characterized by damage to the peripheral nerves. This damage can result from various factors, impacting the nerves’ ability to transmit signals accurately. The damage to these nerves can cause a variety of symptoms, depending on the location and extent of the damage. Cold fingers, as a symptom, often signify a disruption in the normal sensory function of the nerves in the extremities.
Symptoms of Peripheral Neuropathy and Cold Fingers
Peripheral neuropathy manifests in a range of symptoms, and cold fingers are often a prominent indicator of the condition’s impact on sensory perception. The symptoms are often described as numbness, tingling, or pain, particularly in the extremities. These sensations are often accompanied by a loss of touch sensitivity, making it difficult to distinguish between hot and cold temperatures.
This can manifest as an increased sensitivity to cold, where the affected areas, like the fingers, experience cold sensations more intensely than normal. The altered temperature perception can result in an inability to accurately judge temperature changes, leading to an individual experiencing cold fingers when others don’t perceive the environment as cold. Moreover, the diminished sensation of touch can contribute to injuries, as the individual may not be aware of the degree of coldness or potential for harm.
Underlying Causes and Risk Factors
Peripheral neuropathy can stem from a variety of underlying causes. Diabetes is a leading cause, as high blood sugar levels can damage the nerves over time. Other factors include infections, autoimmune disorders, nutritional deficiencies, and certain medications. Genetic predisposition also plays a role in some cases. Furthermore, excessive alcohol consumption can contribute to nerve damage, and prolonged exposure to toxins can cause peripheral neuropathy.
Certain medical conditions can also increase the risk, such as kidney disease or thyroid disorders.
Comparison of Symptoms
| Condition | Symptoms Related to Cold Fingers | Other Notable Symptoms |
|---|---|---|
| Peripheral Neuropathy | Increased sensitivity to cold, numbness, tingling, loss of touch sensitivity in extremities (including fingers) | Pain, burning sensation, muscle weakness, difficulty with balance, foot drop |
| Raynaud’s Phenomenon | Intermittent episodes of cold, numb, and pale fingers or toes, triggered by cold or stress | Color changes in affected areas (white, blue, red), pain, swelling |
| Hypothermia | Cold, numb fingers and other extremities, accompanied by shivering, confusion, and loss of coordination | Significant drop in body temperature, loss of consciousness |
| Frostbite | Frozen, pale, numb, and painful fingers and other exposed body parts | Tissue damage, blisters, impaired blood circulation |
This table highlights the distinctions in symptoms between peripheral neuropathy and other conditions that can cause cold fingers. While some symptoms may overlap, the presence of additional symptoms, such as pain, burning sensation, or muscle weakness, can aid in differentiating between these conditions. Careful consideration of the complete symptom picture is crucial for accurate diagnosis and effective management.
Raynaud’s Phenomenon
Raynaud’s phenomenon is a condition characterized by episodes of reduced blood flow to the fingers and, less commonly, toes, ears, and nose. These episodes, known as Raynaud’s attacks, typically occur in response to cold temperatures or emotional stress, causing the affected areas to turn white, then blue, and finally red. Understanding the physiological mechanisms and triggers of Raynaud’s is crucial for effective management and prevention of these painful and uncomfortable attacks.
Physiological Mechanisms of Raynaud’s Attacks
Raynaud’s attacks stem from the abnormal constriction of small blood vessels, primarily arterioles, in the affected areas. This constriction limits blood flow, leading to the characteristic color changes. The exact cause of this abnormal vasoconstriction is not fully understood, but it’s believed to involve the interplay of several factors, including the overactivity of the sympathetic nervous system, and possible genetic predispositions.
The constriction of the blood vessels is triggered by signals from the nerves that control the blood vessels, potentially amplified by factors like cold temperatures or stress.
Triggers for Raynaud’s Episodes
Numerous factors can trigger Raynaud’s attacks. Cold temperatures are a prominent trigger, as exposure to cold air, water, or even objects can initiate the vasoconstriction cascade. Emotional stress, anxiety, and strong emotions can also stimulate the sympathetic nervous system, increasing the likelihood of an attack. Certain medications, such as some beta-blockers and decongestants, have also been linked to the onset of Raynaud’s episodes.
Other lifestyle factors, such as smoking and excessive caffeine consumption, may play a role in exacerbating the condition.
Progression of Raynaud’s Attacks: The Role of Cold Fingers
The progression of a Raynaud’s attack often begins with the sensation of cold, numbness, and tingling in the affected area, frequently the fingers. This is usually followed by a change in skin color. Initially, the skin turns white (pallor) as blood flow is significantly reduced. As the attack progresses, the skin may take on a bluish hue (cyanosis) due to reduced oxygenation of the blood in the affected tissues.
Finally, as blood flow returns, the skin may become red (rubor) and the affected areas may feel warm and painful. The duration of these attacks can vary greatly, ranging from a few minutes to several hours, depending on the severity and individual response to the triggering factor. The role of cold fingers is often pivotal in initiating the cascade of events, setting off the chain reaction of vasoconstriction.
For instance, exposure to a cold environment, such as handling ice or stepping outside in freezing weather, frequently leads to the first symptoms of the attack.
Cold Weather Considerations
Cold weather presents unique challenges to our bodies, particularly when it comes to maintaining healthy blood circulation, especially in the extremities. Understanding how our bodies react to the cold is crucial for staying warm and preventing issues like cold fingers. This section delves into the physiological responses to cold, the impact on circulation, and the vulnerability of hands and fingers.
We’ll also explore practical ways to protect ourselves from the cold.The human body has evolved mechanisms to conserve heat in cold temperatures. These responses are essential for survival but can sometimes lead to discomfort or even problems, especially for individuals with underlying conditions.
Physiological Responses to Cold Weather
The body’s primary response to cold temperatures is to constrict blood vessels in the skin. This minimizes heat loss by reducing blood flow to the extremities. This is a natural defense mechanism. Shivering, another important physiological response, generates heat through involuntary muscle contractions.
Cold Weather’s Effect on Blood Circulation in the Extremities
Cold temperatures significantly impact blood flow, especially in the extremities like hands and feet. The constriction of blood vessels in response to cold reduces blood flow to these areas, making them more susceptible to coldness and potential damage. This reduced blood flow can also cause numbness and tingling. The time it takes for blood to return to normal temperatures after exposure to cold weather can vary greatly from person to person.
Why Hands and Fingers Are More Vulnerable
Hands and fingers, being the furthest extremities from the core of the body, are the most exposed and therefore the most susceptible to cold. Their smaller size and thin skin contribute to their increased vulnerability. The surface area of these extremities compared to the volume of blood flowing through them makes them especially prone to losing heat rapidly.
Appropriate Clothing and Protective Measures
Maintaining warmth in cold weather involves more than just wearing layers. Choosing appropriate clothing is vital to protect against the cold. Wearing multiple layers of clothing, such as a base layer, a mid-layer, and an outer layer, traps air between the layers, creating insulation.
- Base Layer: A moisture-wicking material like merino wool or synthetic fabrics is essential to keep your skin dry, preventing the chilling effects of sweat. This is the first layer against your skin.
- Mid-Layer: Insulating materials like fleece or down jackets help retain body heat.
- Outer Layer: A waterproof and windproof outer layer shields you from the elements, preventing the penetration of cold air and rain.
Protective measures also include wearing gloves or mittens. Gloves offer more dexterity, while mittens provide better overall warmth due to their enclosed design. Consider using warm socks, hats, and scarves to further protect vulnerable areas. Using hand warmers or insulated gloves can significantly improve hand warmth, especially in extreme cold.
Conclusive Thoughts
In conclusion, understanding what cold fingers mean requires a multifaceted approach. From underlying medical conditions to environmental factors and lifestyle choices, a variety of elements can contribute to cold fingers. By recognizing the potential causes and symptoms, you can take proactive steps towards maintaining healthy circulation and overall well-being. Whether it’s a simple cold or a more serious issue, understanding the causes and symptoms is crucial for seeking the right medical advice.